Peer Reviewed
Feature Article Hepatology
Using natural history to guide management of chronic hepatitis B
Abstract
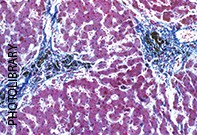
During their lifetime, 20 to 40% of patients with chronic hepatitis B infection will develop serious complications such as cirrhosis or hepatocellular carcinoma. The management strategy employed for patients with hepatitis B depends on the stage of the chronic infection.
Key Points
- Screening for HBV infection should be carried out in individuals who are at high risk, such as those from high or intermediate prevalence countries, injection drug users and men who have sex with men.
- Primary prevention involves immunisation of high-risk individuals and education of infected patients to minimise transmission risk.
- It is reasonable to observe patients who are in the immunotolerant stage of infection or who have inactive infection. Liver function tests should be performed every six to 12 months, and patients referred when alanine aminotransferase (ALT) levels become elevated or there are concerns about the development of advanced liver disease.
- Antiviral therapy (pegylated alfa-interferon, lamivudine, adefovir or entecavir) is generally indicated in patients with evidence of active viral replication and associated hepatic inflammation and fibrosis. Most patients on antiviral therapy will be followed up in specialist clinics.
- HBV-infected patients with cirrhosis should always be treated to reduce the risk of developing liver failure and hepatocellular carcinoma (HCC), for which they have a 100-fold increased risk compared to non-infected individuals, and to improve mortality.
Purchase the PDF version of this article
Already a subscriber? Login here.