Advanced management of Parkinson’s disease – beyond the ‘shaking palsy’
Good management of Parkinson’s disease requires a patient-centric approach understanding the broad involvement of the disease and its impact on the patient and carer. The motor features of tremor, bradykinesia and rigidity are central to diagnosis and respond best to dopaminergic therapies. Extradopaminergic involvement relates to a range of important nonmotor symptoms that connect to sleep, neuropsychiatric disturbances, dementia, dysautonomia and sensory symptoms. They are often under-recognised, but if identified and managed they can offer an opportunity for treatment that may impact positively on the quality of life of both patients and carers.
- The features of tremor, bradykinesia and rigidity form the core diagnostic features of Parkinson’s disease and respond best to dopaminergic therapies and advanced therapies.
- Motor fluctuations in advanced disease can be approached by fractionating levodopa, adding on other pharmacotherapies and considering advanced therapies.
- Nonmotor symptoms in Parkinson’s disease are ubiquitous and diverse, frequently relating to degeneration outside the dopaminergic system, and are often challenging to treat. However, they offer an opportunity to address features that impact heavily on quality of life.
- Common nonmotor symptoms include those relating to sleep, neuropsychiatric disturbances, dementia, autonomic dysfunction and sensory symptoms.
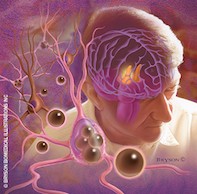
Picture credit: © Bryson Biomedical Illustrations Inc
Parkinson’s disease is common in our community and patients with more advanced disease are often limited in their ability to attend specialist appointments. This fact and the inequitable multidisciplinary care offered to affected patients in Australia mean that primary care physicians are often required to make clinical decisions about their care. Here we discuss some of the complications of Parkinson’s disease, both motor and nonmotor, that may be experienced in the more advanced stages of the disease and some strategies to address these problems.
Background
It has been 200 years since the famous An Essay on the Shaking Palsy was penned by James Parkinson describing the condition that was subsequently attributed to his name. A range of therapies have revolutionised the symptomatic management of Parkinson’s disease but a proven disease-modifying treatment or cure remains elusive. With continuing neurodegeneration, the disease inevitably progresses in all patients over time.
Aggregates of alpha-synuclein (Lewy bodies) are the pathological hallmark of the condition, whereas the loss of dopaminergic neurons in the substantia nigra correlates best with the progression of the clinical symptoms of rigidity and bradykinesia. Pathological studies of Parkinson’s disease have identified multiple additional areas of the brain and peripheral nervous system also affected by this neurodegenerative process, leading to loss of other neurotransmitters being implicated in the clinical features of the disease.
Initial signs of Parkinson’s disease that alert the patient and practitioner to the diagnosis include the cardinal motor features of the disease: rest tremor, muscular rigidity, bradykinesia and postural instability. In early disease where there is still some intrinsic effective dopaminergic function, dopaminergic medications are effective in managing these symptoms. As loss of central dopaminergic neurons progresses, patients become more reliant on exogenous dopamine and motor response complications develop, including motor fluctuations and dyskinesias. With advanced disease, dopamine-resistant motor complications of the disease become more problematic, such as dysphagia, sialorrhoea, postural instability and falls.1
Nonmotor symptoms such as depression and constipation are experienced universally in patients with Parkinson’s disease (Figure 1). Each patient reports an average of eight to 10 nonmotor symptoms.2,3 Some symptoms can predate the onset of motor symptomatology – including sleep disturbance, anosmia, depression and constipation – and can have value in the diagnosis of Parkinson’s disease.4 Nonmotor symptoms can have a higher impact on health-related quality of life than motor symptoms.5 They also impact highly on carers and often become the instigator for patients to transition into nursing home care.1
Managing motor fluctuations
During the off-phase patients may experience episodes of ‘wearing-off’, where their stiffness and slowness returns sooner than expected following levodopa doses. They may also have a delayed on-phase where the levodopa therapy does not work as quickly as it did previously. In addition, off-phases might not be predictable and may become more problematic, with development of off-phase dystonia and neuropsychiatric manifestations such as anxiety and depression.6
During the on-phase, levodopa-induced dyskinesia can occur as a peak-dose effect. It may also be diphasic, occurring on the way up and down from the peak dose. Dyskinesia is generally less troublesome for patients than their off-phase symptoms. On-phase dystonia can also occur. The aim in treating motor fluctuations is to keep dopaminergic stimulation at an adequate level to promote motor benefits while minimising dyskinesia.
Adjusting levodopa
In Australia formulations of levodopa are combined with a peripheral dopa decarboxylase inhibitor, either benzerazide or carbidopa, which block peripheral conversion of levodopa to dopamine. This minimises peripheral side effects and optimises the delivery of levodopa across the blood–brain barrier to the central nervous system. Increasing individual doses of levodopa will result in improvement in off-phase symptoms, but in advanced disease it is often associated with dyskinesia and may worsen orthostatic intolerance. Fractionating levodopa doses by using smaller doses of levodopa more frequently may result in more on-phase time while minimising dyskinesia (Figure 2). Slow-release formulations can be useful for overnight symptoms, although reduced bioavailability and erratic gastrointestinal absorption limits their utility for managing daytime fluctuations.
Add-on pharmacotherapies to levodopa
If altering the frequency to smaller doses of levodopa is not optimally effective, the following can be considered as add-on therapies to levodopa.
Monoamine oxidase type B inhibitors
Monoamine oxidase type B (MAO-B) inhibitors provide some improvement in the total daily off time. Unlike treatment with nonselective MAO inhibitors, there is no need to ask patients to follow a tyramine-restricted diet because cases of hypertensive crisis have been very rarely found in postmarketing follow up of the type B inhibitors.
MAO-B inhibitors contribute to an overall risk of serotonin syndrome. Judicious use of concurrent medications contributing to this risk is recommended in patients taking rasagiline (1mg daily), and use of selective serotonin reuptake inhibitors is contraindicated with selegiline (2.5 to 5mg daily).
Catechol-0-methyl transferase inhibitors
Entacapone reduces the metabolism of levodopa and is available in Australia as monotherapy (200mg tablets) or in a combination preparation with levodopa and carbidopa at a dose of 200mg. Reddish brown urine is a harmless side effect of entacapone although it can be concerning for patients.
Amantadine
How amantadine works in Parkinson’s disease is not fully understood. It is generally accepted that it is an N-methyl-D-aspartic acid receptor antagonist affecting the dopaminergic system that also has anticholinergic effects. This can be problematic in patients with cognitive impairment, and amantadine is avoided in patients with dementia or hallucinations. Amantadine is introduced at a dose of 100mg daily, but this can be increased to 100mg twice daily.
Dopamine agonists
Available dopamine agonists include the non-ergot-derived agents, pramipexole and rotigotine. Older, ergot-derived dopamine agonists are not frequently used because of the risk of developing cardiac valvular disease or pleuropericardial fibrosis.
Pramipexole is started at night at a dose of 0.375mg per day and the extended-release formulation is not considered inferior in efficacy to the immediate-release formulation. The dose can be augmented slowly. The maximum dose is 4.5mg per day. Monitor for the emergence of pedal oedema, daytime somnolence and impulse control disorders, especially with doses of more than 3mg. Dose reduction is recommended in the first instance if these side effects are encountered. Rotigotine has a similar side effect profile. It is started using a 2mg/24 hours patch. The doses can be increased slowly in increments of 2mg/24 hours to obtain optimal symptomatic relief to a maximal daily dose of 8mg/24 hours.
Continuous dopaminergic stimulation
In the setting that medical therapy fails, advanced therapies offering continuous dopaminergic stimulation may be appropriate, avoiding the peaks and troughs of oral levodopa. These therapies require a movement disorders specialist to initiate and monitor them. Each advanced therapy provider has established a customer support program, often with provision of home visits by a company representative trained in the delivery system.
Levodopa–carbidopa intestinal gel
This is delivered directly to the proximal jejunum via a percutaneous endoscopic gastrostomy (PEG) tube with a jejunal extension connected to a pump system. This bypasses the stomach and avoids issues with variable gastric emptying that may occur in Parkinson’s disease. The pumps are programmed to deliver a bolus in the morning and an infusion over the daytime. It is generally not given at night and patients may continue to use an oral levodopa preparation for nocturnal symptoms. Patients have the capacity to deliver an extra bolus dose when needed. The usual complications of having a PEG tube can be encountered. Oral medications are withdrawn during the infusion time.
Subcutaneous apomorphine infusion
Apomorphine is a potent dopamine agonist of rapid onset with effects equivalent to levodopa. It can be used as an intermittent rescue treatment or as a continuous infusion that is generally only given during waking hours. Complications are similar to those encountered with other dopamine agonists, in addition to subcutaneous needle-site problems.
Deep brain stimulation
This surgical procedure is useful for treating tremor as well as motor fluctuations. It involves implantation of programmable multicontact electrodes into the brain, which are connected by a tunneled extension wire to a neurostimulator placed subcutaneously on the upper chest. Intermittent direct current is applied to the target (usually subthalamic nuclei or globus pallidus interni) with an overall inhibitory effect, possibly by effecting neurotransmitter release.7 Surgical complications, including stroke, may be encountered and psychiatric problems may occur postoperatively in addition to device-related issues.
Managing other motor symptoms
Falls
Motor disability, postural instability and gait freezing contribute to falls, although falls are often multifactorial. Other complications of Parkinson’s disease, most frequently orthostatic hypotension, are also implicated. There are several other factors aside from Parkinson’s disease that could be contributing to the falls risk. The typical patient with Parkinson’s disease is often of advanced age with comorbid medical conditions such as visual disturbance, osteoarthritis and peripheral neuropathy. Polypharmacy may also be a factor. These non-Parkinson’s disease causes should be considered when reviewing a patient with Parkinson’s disease who is susceptible to falls.
Rehabilitation with a physiotherapist and other forms of exercise can improve gait and potentially reduce falling in patients with Parkinson’s disease, in addition to improving cognitive performance, motor function and quality of life.8
Sialorrhoea and dysphagia
Dysphagia can be present at diagnosis and progress with advancing disease. Sialorrhoea (drooling) and xerostomia (dry mouth) often coexist in patients with Parkinson’s disease and result from orophyaryngeal bradykinesia, habitual mouth breathing and reduced tongue mobility. Chewing gum is a nonpharmacological therapy that encourages swallowing and may improve sialorrhoea. Review by a speech pathologist is important to instill advice regarding appropriate swallowing and airway protection techniques.
Medical therapy of sialorrhoea aims to reduce saliva production but may worsen xerostomia and promote tooth decay. Anticholinergics may be effective but are often limited by side effects, including worsening cognition and bladder dysfunction. Botulinum toxin injection of the parotid glands, and occasionally the submandibular glands, is also effective in reducing salivary production. This procedure needs to be performed by a physician with experience in botulinum toxin injections.
Managing nonmotor symptoms
Sleep problems
Rapid eye movement sleep behaviour disorder
As the search for a neuroprotective therapy gains pace, there has been increasing interest in the problem of rapid eye movement (REM) sleep behaviour disorder. REM sleep behaviour disorder is characterised by the absence of normal muscle atonia during REM sleep with repeated episodes of sleep-related vocalisations and/or complex motor behaviours. REM sleep behaviour disorder can be detected in clinical practice by asking the bed partner if the person acts out their dreams.
Natural history studies of middle-aged people with REM sleep behaviour disorder are increasingly showing that all patients are likely to develop a synucleinopathy over time (either Parkinson’s disease, dementia with Lewy bodies or multisystem atrophy). Synucleinopathy is the pathological diagnosis postmortem in 93% of patients with both proven and probable REM sleep behaviour disorder identified using polysomnography.9 Polysomnography shows REM sleep without muscle atonia but with motor behaviours.10 Damage to the brainstem circuits that mediate REM sleep atonia is thought to cause REM sleep behaviour disorder.
There are several neurochemical systems involved in the pathogenesis of REM sleep behaviour disorder and it may emerge with antidepressant medication, particularly with selective serotonin reuptake inhibitors or serotonin and norepinephrine reuptake inhibitors.10 When managing REM sleep behaviour disorder, suspected inciting medications should be ceased if possible. Otherwise, in clinical trials 0.5 to 2mg of clonazepam before bedtime improved REM sleep behaviour disorder and reduced phasic twitching in 90% of the patients. However, it did not re-establish REM atonia. Side effects include daytime somnolence, cognitive impairment and aggravation of obstructive sleep apnoea.11 In patients with cognitive impairment, 3mg of melatonin at bedtime may be an alternative; unlike clonazepam, this drug also restores REM sleep muscle atonia.
Other sleep-related motor problems
In Parkinson’s disease, motor problems during sleep are encountered more often than REM sleep behaviour disorder. Bothersome motor symptoms that lead to an increased number of awakenings and discomfort during the night include tremor and nocturnal akinesia (rigidity, problems turning and pain). There is also a higher risk of restless leg syndrome. Remember to investigate iron deficiency in restless leg syndrome to eliminate this as a cause. When ferritin levels are less than 50mcg/L, symptomatic benefit for restless legs can be achieved with iron replacement. Sleep-related motor problems can otherwise be addressed with dopaminergic therapy. Nonmotor symptoms including nocturia, hallucinations and pain may also contribute to sleep disturbance in Parkinson’s disease.
Daytime somnolence, a symptom that may also precede development of Parkinson’s disease motor symptoms, increases with advancing disease and has implications for driving. Tapering the daytime dose of dopamine agonist and improving nocturnal sleep quality may help this symptom.
Neuropsychiatric features
Neuropsychiatric features may be secondary to Parkinson’s disease neuropathology or a complication of dopaminergic replacement therapies. They may precede motor symptoms by many years.
Depression and anxiety
Depression and anxiety are common in patients with Parkinson’s disease with up to 35% of patients exhibiting some depressive symptoms.12 Depression is the most influential variable on quality of life in Parkinson’s disease disability.2 It may be amenable to antidepressant medication13-15 and some dopamine agonists have also been reported to be effective (Table).13-20 Low mood, anxiety and panic can also occur in wearing-off periods from dopaminergic therapy. This may be amenable to treatment adjustments to reduce the off-periods. Cognitive behavioural therapy has been shown to be helpful with managing the symptoms of depression and anxiety. However, the benefits have not translated into improved functional outcomes in patients or reduced carer burden.21
Impulse control disorders
Various addictive behaviours occur in Parkinson’s disease, the most typical being impulse control disorder. Excessive use of dopaminergic medications (dopamine dysregulation syndrome) and compulsive behaviours such as hobbyism (punding) are also occasionally seen.
Common impulse control disorders are pathological gambling, compulsive buying, compulsive sexual behaviour and binge or compulsive eating. Risk factors for impulse control disorders in Parkinson’s disease include:22
- being on higher dopaminergic medication doses
- using dopamine agonists
- developing Parkinson’s disease at a younger age
- being unmarried
- being a current cigarette smoker
- having a family or personal history of addictive behaviours (e.g. gambling).
When an impulse control disorder occurs in a patient taking a dopamine agonist, its withdrawal can improve the impulse control disorder but may trigger an unpleasant dopamine agonist withdrawal syndrome. Dopamine agonist withdrawal syndrome manifests predominantly with psychiatric symptoms including anxiety, panic attacks, depression, agitation, irritability and drug craving.23 The problematic psychiatric symptoms of dopamine agonist withdrawal syndrome are often not responsive to other therapies and can require re-initiation of a smaller dose of the original or another dopamine agonist. Psychosocial strategies should also be put in place to minimise the risk of impulse control disorder relapse and divert destructive behaviours.
Parkinson’s disease psychosis
Psychosis occurs in about 30% of patients with Parkinson’s disease and consists of hallucinations, illusions and delusions. Patients often have a clear sensorium and usually retain their insight, which differentiates Parkinson’s disease psychosis from delirium and schizophrenia.24
Minor hallucinations experienced in the normal population are more common in patients with Parkinson’s disease. These are misperceptions, which include: a sense of presence (perceiving another person is in the room); sense of passage (detecting shadows passing by); and illusions (misinterpreting the identity of real objects).25
Visual hallucinations are the most common psychotic symptom in Parkinson’s disease and generally consist of complex images of people and animals.25 Patients may have some paranoid tendencies but these are generally nonthreatening. Visual hallucinations occur more frequently in low lighting and in the evening. Auditory, olfactory and tactile hallucinations can also occur, but are less common.
Delusions generally consist of paranoid delusions, usually concerning a phantom person in the house or spousal infidelity and abandonment.24 Delusions are difficult to treat and are often accompanied by difficult behaviours in patients who experience them.
Advanced age, cognitive impairment and concurrent sleep disorders are risk factors for the development of Parkinson’s disease psychosis. The usual triggers for delirium may also worsen Parkinson’s disease psychosis. Medications may contribute, including Parkinson’s disease medications, so it is important to reduce and possibly discontinue the offending agents. Psychosis may improve if medications are withdrawn in the following order:
- anticholinergics
- amantadine
- MAO-B inhibitors
- dopamine agonists
- catechol-O-methyl transferase inhibitors
- levodopa.
The diurnal variation in psychotic symptoms means that, when reducing levodopa, the evening and overnight doses are the first to be tapered. If the psychosis is not improved by medication rationalisation, an antipsychotic can be tried (Table). Cholinesterase inhibitors may be effective in treating Parkinson’s disease psychosis in patients with dementia (Table).
Dementia
Parkinson’s disease dementia is common, with a mean time of onset of about 10 years after a diagnosis of Parkinson’s disease.26 In addition to memory, the executive, attentional and visuospatial cognitive domains are particularly affected in Parkinson’s disease dementia.26 Failure to draw intersecting pentagons correctly in the mini mental state examination is a helpful hint to visuospatial dysfunction and possible Parkinson’s disease dementia.
Patients may be diagnosed with mild cognitive impairment before the development of Parkinson’s disease dementia. The presence of visual hallucinations and illusions also confers a higher risk for cognitive decline in the future. There is evidence for using cholinesterase inhibitors, particularly rivastigmine, to treat Parkinson’s disease dementia.20
Limbic and cortical Lewy body pathology is the main pathological finding in Parkinson’s disease dementia. About one-third of patients will also have an amyloid pathology and an overlap with Alzheimer’s dementia.26
Autonomic complications
Orthostatic hypotension
Orthostatic hypotension is common in patients with Parkinson’s disease and patients do not always report postural lightheadedness. It is defined as a fall in systolic blood pressure of at least 20mmHg and in diastolic pressure of at least 10mmHg within three minutes of standing up from a supine position. There is evidence for both central and peripheral autonomic nervous system dysfunction in patients with Parkinson’s disease, particularly with noradrenergic loss. Orthostatic hypotension sometimes occurs in early Parkinson’s disease but consider multiple system atrophy if blood pressure problems are very prominent at this stage. Levodopa can contribute to orthostatic hypotension in a dose-dependent manner. To reduce this, a peripheral dopamine receptor antagonist such as domperidone may be tried.
It is important to review antihypertensive and diuretic therapy when there is a diagnosis of orthostatic hypotension. Volume expansion with a bolus of two glasses of water, particularly first thing in the morning, may help. The pharmacotherapy options for orthostatic hypotension are summarised in the Table.
Urogenital dysfunction
Bladder dysfunction in Parkinson’s disease is due to neurogenic detrusor overactivity. As affected the population is elderly, other causes for bladder dysfunction must not be overlooked. Before initiating therapy, a urine microscopy and culture is recommended to assess whether a urinary tract infection is present. This is in addition to a postvoid residual bladder volume to assess urinary retention, which may be exacerbated by therapy for detrusor overactivity.
Pharmacotherapy options are summarised in the Table. In those refractory to medical therapy, bladder botulinum toxin injections may be efficacious if there is evidence of an overactive bladder. Erectile dysfunction typically responds to phosphodiesterase type 5 inhibitors. Psychological therapy may also be required to address the psychological contributors to sexual dysfunction.
Gastrointestinal dysfunction
The entire gastrointestinal tract can be involved in Parkinson’s disease. Gastroparesis may cause nausea and vomiting as well as malabsorption of medications. Dopaminergic medications may also contribute to nausea and sometimes manifest in patients as poor appetite with accompanying weight loss. When nausea is a problem, a medication review is warranted in addition to a trial of domperidone. If gastroparesis impairs the oral delivery of dopaminergic therapies change to a topical therapy if possible, and exploring advanced therapies is also indicated.
Slow colonic transit results in constipation, which is common in Parkinson’s disease and often predates the onset of motor symptoms. Abnormal levels of alpha-synuclein have been found in the biopsied gastrointestinal tissue obtained from patients with Parkinson’s disease.27 Basic treatment of constipation in Parkinson’s disease includes recommending patients have a high-fibre diet, use psyllium preparations, are adequately hydrated and participate in exercise. A trial of domperidone may be helpful. Other agents of proven efficacy are osmotic laxatives such as polyethylene glycol (17g daily) or lactulose (10 to 40g daily).
Sensory features
Anosmia is an early feature of Parkinson’s disease and often goes unnoticed by patients. Peripheral neuropathy has been noted to occur more often in patients with Parkinson’s disease. It may be related to vitamin B12 or B6 deficiency so this should be investigated and replacement therapy recommended when detected.
Pain is a common problem for patients with Parkinson’s disease and presents in both early and advanced disease. Shoulder pain may be a presenting symptom of Parkinson’s disease, preceding more obvious motor features on that side.28 Motor manifestations causing pain and also central pain with neuropathic features (which can also have autonomic and visceral characteristics) may respond to dopaminergic therapy. Orthopaedic pain is often encountered too, which can be treated with the usual therapies such as paracetamol and NSAIDs.
Conclusion
Although Parkinson’s disease is considered a disorder characterised by motor symptoms, nonmotor symptoms are an integral part of this syndrome. Nonmotor symptoms can be as troublesome as motor symptoms and impact on activities of daily living, but they are often under-recognised by healthcare professionals. Their identification may aid diagnosis of the disorder as well as provide pathways to an improved quality of life for patients, especially for those with advanced disease. MT