What’s the diagnosis?
A teenager with facial papules and pustules

Case presentation
An 18-year-old man presents with a six-year history of facial papules, pustules and comedones. He has tried various over-the-counter topical treatments containing 5% benzoyl peroxide and topical 1% clindamycin hydrochloride prescribed by his GP. During the last four months he has developed nodulocystic lesions.
On examination, widespread comedones, papules and pustules are observed on the patient’s temples, cheeks and jawline and extending down his neck (Figure). Icepick and rolling scars are noted. There are also cystic lesions on his left cheek and jawline.
Differential diagnoses
Conditions to consider among the differential diagnoses for a patient presenting with these facial lesions include the following.
Rosacea
The term rosacea encompasses a constellation of clinical findings, with persistent facial erythema and inflammatory papules and pustules being key components.1 It has a prevalence of about 5.5% in women and 4% in men, with a peak incidence between the ages of 40 and 50 years.2,3
The pathogenesis of rosacea involves a genetic predisposition and environmental triggers.2 Two major abnormalities are neurovascular dysregulation and an augmented immune response, both of which can lead to cutaneous inflammation.4 From a clinical perspective, it is useful to classify rosacea into the four subtypes (erythematotelangiectatic, papulopustular, phymatous and ocular), as this has implications for treatment.4
For the case patient, rosacea can be excluded because comedones are not a feature of the condition. His age makes this diagnosis less likely, and the abundance of nodulocystic lesions and the extension of the skin eruption down the neck are not typical of rosacea.
Folliculitis
There are many types of lesions in folliculitis; however, universally, presentations are relatively monomorphous.5 It typically consists of follicular pustules with an erythematous rim or follicle-based erythematous papules with or without a superimposed collarette of scale.5
There are three subtypes of folliculitis that are most relevant to the case patient above.
• Gram-negative folliculitis is usually caused by Escherichia coli, Klebsiella, Enterobacter and Proteus spp. It is typically seen in patients with acne vulgaris who have received long-term antibiotic treatment but can also occur in men with oily skin.5 It presents with pustules in the facial T-zone and in a perinasal distribution.5
• Malassezia folliculitis lesions are usually pruritic, follicular papules with occasional pustules. A microscopic potassium hydroxide (KOH) preparation of follicular contents reveals abundant yeast forms.5
• Irritant folliculitis is caused by the use of topical treatments such as ointments, especially when applied in a direction that opposes the hair growth.5 Follicular pustules are seen in sites of irritant exposure, favouring areas with terminal hairs.5
For the case patient, the presence of comedones and the polymorphous and irregular nature of the skin eruption are not consistent with folliculitis.
Acne vulgaris
This is the correct diagnosis. Acne, which is a multifactorial disorder of the pilosebaceous unit, varies in severity from mild comedonal to fulminant systemic disease.6 Peak incidence occurs during adolescence, affecting about 85% of individuals aged between 12 and 24 years.6 However, acne can persist well into adulthood, with 26% of women and 12% of men affected in their 40s.7 Epidemiologically, acne is more prevalent in Western countries, suggesting that environmental factors contribute to its pathogenesis.8
Acne is typically found in sites with well-developed sebaceous glands such as the face and upper trunk.6 Clinically, lesions are divided into noninflammatory (open and closed comedones) and inflammatory (papules, pustules, nodules and pseudocysts) groups.6 To make a diagnosis of acne, there must be comedones – the presence of papulopustular lesions alone is not sufficient because these can occur in other disorders.
The development of acne involves the interplay of factors, including follicular hyperkeratinisation, hormonal influences on sebum production and composition, and inflammation, partly mediated by Cutibacterium acnes (formerly known as Propionibacterium acnes).6 Almost all acne treatments target, to varying degrees, at least two of these factors.
For the case patient, the presence of comedones as well as the distribution and morphology of the eruption are consistent with a diagnosis of nodulocystic acne and he is in the typical age group for the condition. Early treatment is essential to prevent lasting cosmetic disfigurement caused by postinflammatory hyperpigmentation and scarring, which is a common sequela of acne – particularly nodulocystic acne.6 Gram-negative folliculitis, which can complicate a diagnosis of acne, was not present.
Management
Step 1: Determine if there are contributing factors
The role of contributing factors that are potentially reversible should be considered in the management of acne. In female patients, the most common hormonal cause is polycystic ovarian syndrome (PCOS), so it is important to enquire about menstrual irregularities and to look for signs of hyperandrogenism such as hirsuitism. Screening should be undertaken if PCOS is suspected.
It is helpful to ask about the use of cosmetics or pomades. Thick moisturisers, makeup and sunscreens can exacerbate follicular occlusion.
Acne can be induced by a range of medications. Hormonal causes include corticosteroids, anabolic steroids, testosterone and contraceptive agents such as medroxyprogesterone, etonogestrel and intrauterine levonorgestrel.6 Other causes include halogens, antituberculoid drugs (such as isoniazide, rifampicin), lithium, vitamin B6/B12 supplements, epidermal growth factor receptor inhibitors, ciclosporin, phenytoin and Janus kinase inhibitors.
Step 2: Discuss the role of diet
Many of the dietary factors that increase acne do so by increasing insulin-like growth factor 1, which binds to receptors on sebaceous glands and promotes their activity and can contribute to increased growth of C. acnes and follicular occlusion.9 Glycaemic index has the strongest association with acne, followed by milk (particularly skim varieties).10 There is some low level evidence (mainly through case reports and case series) that whey protein may exacerbate acne. However, strict modification of diet is unlikely to be sufficient to control acne in an individual who is predisposed to the condition.
Step 3: Consider topical therapies
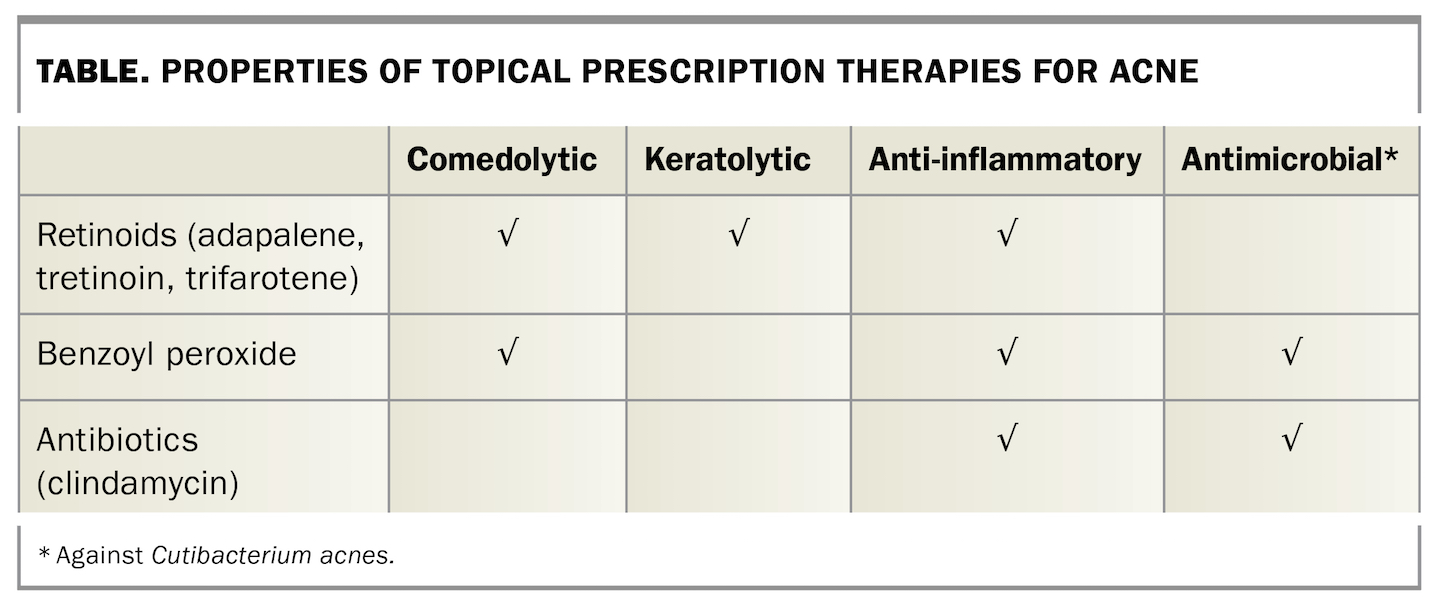
Topical treatments should be used in all acne-prone areas, not just as spot treatments. The properties of topical therapies that are currently available on prescription are summarised in the Table.
Retinoids
Topical retinoids normalise follicular keratinisation and corneocyte cohesion, aiding in the expulsion of existing comedones and the prevention of new ones.6 Retinoids reduce both inflammatory and comedonal lesions. Patients should be warned of the common side effects of local irritation resulting in dryness, peeling and scaling, and sun sensitivity.6 The topical retinoids available are:
- adapalene 0.1%
- tretinoin 0.025% and 0.05%
- trifarotene 0.005%.
Benzoyl peroxide
Benzoyl peroxide (BPO) is a potent bactericidal agent that reduces C. acnes within the follicle and also has mild comedolytic and anti-inflammatory properties.6 Microbial resistance to BPO has not been reported (unlike for topical antibiotics). Contact dermatitis should be suspected in patients who develop marked erythema when using BPO. Patients should be warned of its bleaching effect on fabrics.
Antibiotics
Topical antibiotics (e.g. clindamycin 1%) are commonly used to treat acne alone or in combination with benzoyl peroxide or a retinoid. It is important to note that that they do not treat noninflammatory lesions.
Combination therapies
Combination therapies are used for most patients when topical treatments are prescribed for acne. The fixed-dose combination products available are:
- adapalene 0.1% or 0.3% plus BPO 2.5%
- clindamycin phosphate 1% plus BPO 5%
- clindamycin phosphate 1% plus tretinoin 0.025%.
Others
Azelaic acid (15 to 20%) inhibits growth of C. acnes and has comedolytic properties and is useful for treating both inflammatory and comedonal acne as well as rosacea and postinflammatory hyperpigmentation.6 Salicylic acid is widely used for its comedolytic and antibacterial properties.6
Step 4: Consider systemic therapies
There are three main types of systemic therapy for acne.
Antibiotics
The antibiotics used in acne treatment are commonly doxycycline (50 to 100 mg daily) and minocycline (50 to 100 mg daily); less commonly (usually in the case of pregnancy) erythromycin (400 mg twice daily or 12.5 mg/kg up to 500 mg twice daily) or cephalexin (500 mg twice daily).6 Oral antibiotics should be combined with topical agents targeting comedones. There is currently a paradigm shift away from the long-term use of antibiotics in acne because of the development of antibiotic resistance.
Hormonal therapies
Although the estrogen component is generally similar for combined oral contraceptive pills (COCPs), they differ mainly in the progesterone component. COCPs that contain drosperinone, cyproterone acetate or dienogest are antiandrogenic and are preferred for treating women with acne with hormonal flares.
Spironolactone, particularly in the context of treating acne in women, is safe to use in the long term. Doses of 50 to 200mg daily are used (most commonly 100 mg daily).9 When combined with a COCP, the unwanted side effects of spironolactone (e.g. irregular menses, headaches and breast tenderness) are counteracted and pregnancy is prevented.
Isotretinoin
Isotretinoin, which was approved by the US FDA in 1982, is the most effective treatment for acne. About 85% of patients treated with a dose of 0.5 to 1.0 mg/kg/day are virtually clear of their acne by 16 weeks; 13% of patients require five to six months to clear it, and the remaining require a longer course.11 It is indicated for nodulocystic acne.
Outcome
As the case patient’s acne was severe and topical therapies alone will be insufficient to control the inflammation, his GP arranged dermatology referral for him. Following a failed response to oral antibiotic therapy, his treatment has been escalated immediately to isotretinoin. He will be reviewed every two to three months during treatment. MT
COMPETING INTERESTS: None.
References
1. Powell FC, Ní Raghallaigh S. Rosacea and related disorders. In: Bolognia JL, Schaffer JV, Cerroni L (eds). Dermatology, 4th ed. Philadelphia, PA: Elsevier; 2018. pp. 604-614.e1.
2. Gether L, Overgaard LK, Egeberg A, Thyssen JP. Incidence and prevalence of rosacea: a systematic review and meta‐analysis. Br J Dermatol 2018; 179: 282-289.
3. Wolff K, Johnson RA, Saavedra AP, Roh EK. Disorders of sebaceous, eccrine and apocrine glands. In: Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, 8th ed. New York, NY: McGraw-Hill Education; 2017.
4. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002; 46: 584-587.
5. Hsiao JL, Leslie KS, McMichael AJ, Curtis AR, Guzman-Sanchez D. Folliculitis and other follicular disorders. In: Bolognia JL, Schaffer JV, Cerroni L (eds). Dermatology, 4th ed. Philadelphia, PA: Elsevier; 2018. pp. 615-632.e3.
6. Zaenglein AL, Thiboutot DM. Acne vulgaris. In: Bolognia JL, Schaffer JV, Cerroni L (eds). Dermatology, 4th ed. Philadelphia, PA: Elsevier; 2018. pp. 588-603.e1.
7. Collier CN, Harper JC, Cafardi JA. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol 2008; 58: 56-59.
8. Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J. Acne vulgaris: a disease of Western civilization. Arch Dermatol 2002; 138: 1584-1590.
9. Kang D, Shi B, Erfe MC, Craft N, Li H. Vitamin B12 modulates the transcriptome of the skin microbiota in acne pathogenesis. Sci Transl Med 2015; 7: 293ra103.
10. Meixiong J, Ricco C, Vasavda C, Ho BK. Diet and acne: a systematic review. JAAD Int 2022; 7: 95-112.
11. Layton A. The use of isotretinoin in acne. Dermatoendocrinol 2009; 1: 162-169.