Peer Reviewed
Feature Article Ophthalmology
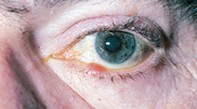
Ophthalmic tips and traps: practical advice for GPs
Abstract
The GP is likely to be faced with a number of perplexing ophthalmic conditions. This article presents a selection of such problems, with the emphasis on diagnoses possible with the resources available.
Key Points
- Remind patients with an everted lower punctum that wiping tears away in a downward direction from the eye tends to evert the punctum further. Tell patients to wipe tears away in an upward direction.
- Do not omit to palpate the preauricular gland when an eye is red. Preauricular adenitis is an almost sine qua non with viral keratitis.
- Recurrent unilateral ‘conjunctivitis’ may be a herpetic ulcer. If any suspicion exists that a lesion may be herpetic, do not use topical steroids. (There is a place for topical steroids in some ophthalmic herpetic infections at certain stages of the condition, but such a decision should be made by an ophthalmologist.)
- Remember that an anaesthetic eye can prevent a patient from being aware of a foreign body or an ulcer.
- An individual’s risk of glaucoma is higher when diabetes or hypertension is present. Diabetes in a close relative also increases the risk.
- If you have the slightest doubt about the possibility of a turned eye in a child, refer promptly to an ophthalmologist for cycloplegic refraction. Do not be misled by a child seeing 6/6. Many children with latent hypermetropia can see 6/6, but the effort involved may produce an ocular deviation.
- Remember what a great imitator zoster ophthalmicus can be in the painful prodromal stage before skin lesions appear.
Purchase the PDF version of this article
Already a subscriber? Login here.