Bariatric surgery: positive and negative effects
Bariatric surgery is recognised as a legitimate treatment for obesity. Knowledge of its key long-term outcomes, such as durability of weight loss, remission of obesity-related comorbidities and surgical complications, has grown exponentially in recent years. Further insights into the physiological mechanisms underlying outcomes will drive more effective and less invasive techniques that can be individualised to a patient’s needs.
- Weight loss surgery now has long-term data supporting its efficacy and safety in the treatment of obesity.
- Bariatric surgery produces sustained weight loss, leading to remission of type 2 diabetes, reduction in mortality and improvement in many cardiac risk factors.
- Physicians should be familiar with the acute and chronic complications of the widely performed bariatric procedures.
- Postoperative nutritional status and psychological wellbeing need to be monitored carefully in patients who undergo bariatric surgery.
Obesity increases the risk of many severe medical conditions ranging from metabolic disorders (type 2 diabetes, nonalcoholic steatohepatitis, cardiovascular disease), malignancies (colorectal, breast, uterine, oesophageal, renal and pancreatic), hypoventilation and respiratory failure, musculoskeletal disorders, dementia and depression. Importantly, it is independently associated with a reduced life expectancy. Obesity is a major health issue worldwide and in Australia it affects 31% of the adult population and 8% of children and adolescents.1 Despite clinical advances in our understanding of energy balance regulation, effective therapeutic outcomes elude many obese and overweight patients. The customary approach of recommending improvement to diet and exercise patterns does not produce sustained weight loss for most individuals. Newer pharmacological therapies have relatively limited efficacy and are costly, and can be poorly tolerated because of side effects.
A paradigm shift has seen bariatric surgery legitimised as an effective treatment of obesity, and the evidence for its efficacy and safety has grown exponentially. Results from randomised controlled trials have demonstrated clear superiority for bariatric surgery over nonsurgical strategies, at least for short-term outcomes such as remission of type 2 diabetes. Evidence of long-term outcomes is derived largely from observational studies. Ongoing challenges include the identification of eligible patients for bariatric surgery and selection of the most appropriate procedure for each individual and ensuring equitable access to this treatment modality for those most in need.
Types of bariatric surgery
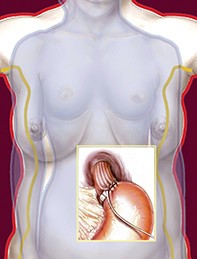
Based on the most recent Australian Bariatric Surgery Registry data, the laparoscopic sleeve gastrectomy (LSG) is the most commonly performed bariatric operation in Australia and accounts for about 70% of surgeries, followed by Roux-en-Y gastric bypass (RYGB) and one anastomosis gastric bypass (OAGB), which together comprise just under 20% of surgeries.2 The popularity of the laparoscopic adjustable gastric banding (LAGB) has significantly reduced, in part related to the substantial need for revisional surgery and the poorer long-term outcomes in the hands of many surgical units, such that it accounts for 2% of bariatric surgical procedures. It is notable that 6% of the bariatric surgery performed in Australia is revisional. These procedures and their effects are described in Figures 1a to c and Table 1. LSG has dominated weight-loss surgeries in both Australia and the US because it is less invasive and more straightforward than gastric bypass with good long-term outcomes. However, bypass procedures appear to have greater metabolic benefits and somewhat more sustained weight loss so are favoured for people with type 2 diabetes.
The OAGB is the newest procedure and has certain advantages over RYGB, such as a single anastomosis, a shorter learning curve for surgeons, fewer defects leading to herniation and easier reversal.3 It is growing in popularity as data is showing outcomes comparable with RYGB.3
Positive effects of bariatric surgery
Weight loss
Compared with conventional treatments, bariatric surgery can produce long-term weight loss that is greater and more sustainable. Data from the large observational Swedish Obese Subjects (SOS) study, published in 2012, showed that bariatric surgery (predominantly the outdated procedure vertical banded gastroplasty [VBG], known as ‘stomach stapling’, that produces a proximal gastric pouch, and which has been largely superseded by the simpler and safer LSG) was associated with greater weight loss than standard care at two years (23% vs 0%) and 20 years (18% vs 1%).4 The prospective Utah Obesity Study demonstrated more effective weight loss for a group of patients undergoing RYGB (27.7%) compared with a nonsurgical control group (0.2% weight gain) after six years of follow up.5 An analysis of UK data has documented four-year weight loss to be 38 kg for RYGB, 31 kg for LSG and 20 kg for LAGB.6 In an Australian study, patients who underwent LAGB were able to maintain more than 50% excess weight loss (defined as the proportion of weight above that which a patient would have at a BMI of 25 kg/m2 that is lost) after more than 10 years of follow up.7 However, in the Longitudinal Assessment of Bariatric Surgery, a multicentre observational study from the US, mean weight loss was 28.4% for RYGB and 14.9% for LAGB seven years after surgery. LAGB was associated with one-third the rate of diabetes remission compared with RYGB (RYGB 60.2% vs LAGB 20.3%).8 There have been two recent randomised controlled trials comparing RYGB with LSG, and although there was greater weight loss with RYGB, this was not statistically significant in either study. At a mean of five years after surgery, RYGB resulted in 68.3% excess weight loss compared with 61.1% for LSG in one study and 57% versus 49% in the other.9,10
Type 2 diabetes
Although the metabolic benefits of weight loss induced by bariatric surgery are well documented, only few patients with type 2 diabetes are offered this therapy. It could be argued that the risk of mortality from diabetes itself far outweighs the risk of mortality at expert centres performing bariatric surgery – a surgical mortality rate of 0.44% for RYGB was reported in a 2015 review.11 The rapidity of the effect on glucose homeostasis after RYGB or LSG implies that it is mediated independently of the weight loss. In contrast, improvements in glucose regulation after LAGB are entirely dependent on weight loss. Hyperinsulinaemic–euglycaemic clamp studies have demonstrated an increase in insulin sensitivity with LSG and RYGB compared with LAGB; whether this is due to the greater weight loss achieved with these procedures or to hormonal changes is unclear. LSG and RYGB have each been shown to induce changes in gut hormones, such as glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide, as well as insulin, which can reduce postprandial glucose levels.12,13 GLP-1 also assists with appetite control by inhibiting gastric emptying and acting centrally to reduce food intake. These procedures have also been shown to increase another anorectic hormone, peptide YY, and to decrease the orexigenic hormone ghrelin, at least in the short term.13
Several high-quality randomised controlled trials have shown significant rates of diabetes remission at one or two years, with positive although lesser rates of remission at three to five years’ follow up. The type 2 diabetes remission rates observed in these clinical trials are summarised in Table 2.14-19 In an Australian study conducted in patients with diabetes of shorter duration (less than two years), a remission rate of 73% was observed two years after LAGB compared with 13% after conventional therapy.14 In one of these trials, a single-centre open-label study of patients with diabetes (over more than five years) in Italy, the diabetes remission (defined as fasting glucose level below 5.6 mmol/L and HbA1c below 6.5% [<48 mmol/mol] while off glucose lowering medication for at least 12 months) rate was 75% in patients treated with RYGB and 0% in patients treated with conventional medical therapy at two years.15 At five years, 37% of the RYGB group maintained remission compared with none of the medically treated patients.16 (This study also included a group undergoing biliopancreatic diversion, a procedure that is now rarely performed in Australia.) In a study with three sites in the US and one in Taiwan in which 120 people with diabetes (mean HbA1c 9.6% [81 mmol/mol], approximately 50% taking insulin) were randomised to RYGB or intensive medical management, 35% of those who had a RYGB were in remission (defined as HbA1c below 6.5% [48 mmol/mol] while off glucose lowering therapy for at least 12 months) at two years and 16% at five years, whereas none of the patients on medical management alone achieved remission at either time point.17
In the STAMPEDE trial, a randomised, nonblinded, single centre trial in the US comparing bariatric surgery with intensive medical therapy for diabetes (n = 150), at one year after randomisation 42% of patients undergoing RYGB and 37% of patients undergoing LSG achieved the primary endpoint (HbA1c less than 6% [<42 mmol/mol] whether or not on glucose lowering therapy, a more lenient endpoint than the preceding studies) compared with 12% of patients receiving medical therapy alone.18 At five years the respective figures were 29% for those who had RYGB, 23% for LSG and 5% in those who received medical therapy alone.19 The average duration of diabetes in the STAMPEDE study population was 8.3 years; at baseline, the mean HbA1c was 9.3% (78 mmol/mol) and 43% of patients were taking insulin.18 Overall, the predictors of diabetes remission with bariatric surgery appear to be lower fasting glycaemia at baseline, shorter duration of diabetes and procedures that divert gastric contents into the small intestine, such as RYGB.20
These findings imply that bariatric surgery should be more broadly available to people with type 2 diabetes and it is now included in guidelines for diabetes management. For example, the American Diabetes Association states that bariatric surgery should be recommended to people with a BMI of 35 kg/m2 or more with type 2 diabetes, and considered in those with a BMI of 30 kg/m2 or more, who do not achieve durable weight loss and improvement in comorbidities with nonsurgical treatments.21 It is also stated that this surgery should be performed in high-volume centres with multidisciplinary teams experienced in the management of diabetes and bariatric surgery.
Bariatric surgery also has an important role in the prevention of diabetes. Follow-up data from the SOS study at 15 years have shown that the group that received bariatric surgery had an incidence of type 2 diabetes that was 78% lower than the group receiving conventional therapies.22
Mortality and cardiovascular risk factors
Many reports of long-term outcomes for bariatric surgery stem from the SOS study, which is characterised by strong long-term follow-up data for many endpoints. This study documented a 29% reduction in mortality for patients who underwent bariatric surgery after almost 11 years of follow up.23 A lower incidence of myocardial infarction and stroke was also reported, although it must be noted that only a minority of patients underwent RYGB or LAGB (most patients underwent VBG). The Utah Obesity Study has reported a reduction in all-cause mortality of 40% and cardiovascular mortality of 49% after RYGB, over a mean follow up of 7.1 years.5
Elevated triglyceride and LDL cholesterol levels as well as reduced HDL cholesterol levels are typical of obesity-related dyslipidaemia. Improvements in total cholesterol and triglyceride levels as well as HDL levels have been demonstrated two years after RYGB.15 The Diabetes Surgery Study showed no significant difference between RYGB and intensive medical management in achieving an LDL cholesterol level less than 2.6 mmol/L.24 This finding was likely because 70% of people in both groups achieved this target and the majority of both groups were already on lipid-lowering therapy.24 Improvements in the lipid profile have also been described with LAGB and LSG but the magnitude of change appears to be greater with RYGB, which is possibly due to an effect on intestinal fat absorption.13
The impact of bariatric surgery on hypertension is less well established. In a trial of 120 patients who received an intensive lifestyle and medical management protocol, no significant difference was observed in the proportion of patients with systolic blood pressure below 130 mmHg in the group that was randomly assigned to undergo additional RYGB and the group that was not.24 Other studies have described reduction or cessation of antihypertensive medications without formally analysing the data. The National Institutes of Health study of long-term outcomes of bariatric surgery published hypertension remission rates of 38.2% after RYGB and 17.4% after LAGB, but this observational study lacked a nonsurgical control population.25 The SOS study showed a reduction in blood pressure in the surgical group compared with controls after two years of follow up but no difference after 10 years, despite weight loss being maintained over this period.26
Quality of life
Robust data from both observational studies and randomised trials indicate positive outcomes for health-related quality of life after bariatric surgery. Statistically significant improvements two years after LAGB have been reported using the Short Form Health Survey (SF-36).18 For patients undergoing RYGB, significantly higher scores in all domains of quality of life have been demonstrated after five years of follow up compared with patients who are medically managed.16 Improvement in female sexual function and pregnancy rates after bariatric surgery has been described.27 RYGB has been associated with increased testosterone levels and improved sexual function in men two years after surgery.28
Negative effects of bariatric surgery
Overall, bariatric surgery is remarkably safe. Mortality rates for bariatric procedures in expert centres are comparable with those for other common operations such as laparoscopic cholecystectomy. Nonetheless, complications can be lethal and require prompt treatment by clinicians who are familiar with the procedure and its potential adverse outcomes.
Inclusion criteria for bariatric surgery emphasise the importance of a patient’s comprehension of the risks and consequences of the operation as well as the necessary preparation for surgery. Patients are often required to follow a very low energy diet for at least two weeks preoperatively to minimise hepatomegaly, which can make surgery more technically difficult. Patients taking antihypertensive or glucose lowering medication need close supervision during this period. Smoking and alcohol excess are also generally viewed as contraindications to bariatric surgery.29 After the surgery and acute recovery stage, mandatory long-term multidisciplinary input requires motivation and compliance from the patient.
Acute complications
Acute complications can occur in 5 to 10% of patients, depending on the operation. Many complications are similar to those that arise after other abdominal surgeries, such as haemorrhage, obstruction, anastomotic leaks, infection, arrhythmia and pulmonary emboli.29
Complications following LAGB include enlargement of the proximal gastric pouch (regurgitation, heartburn), band slippage leading to obstruction (vomiting, dysphagia) and band erosion through the stomach wall (epigastric pain, bleeding, infection). Revision is required in 1 to 2% of cases each year; most complications can be managed through band adjustments and appropriate dietary advice.30 LSG can result in leaks at the staple line, haemorrhage or gastro-oesophageal reflux. Severe gastro-oesophageal reflux is therefore viewed as a contraindication to LSG. RYGB can be complicated by acute anastomotic leaks (1 to 3%) or ulcers, internal hernias or strictures leading to obstruction.30 Strictures may manifest as frequent vomiting and usually mandate prompt investigation and surgical assessment.
Chronic surgical complications
Six percent of operations reported to the Australian Bariatric Surgery Registry in 2019 were revisional. In the SOS cohort, after a mean follow up of 19 years 27.8% of the cohort underwent first time revisional surgery, which included conversions to RYGB, corrective surgery and reversal of the surgery to normal anatomy. LAGB was associated with the highest rate of revisional surgery at 40.7% compared with only 7.5% of those who had RYGB.31 Anastomotic ulceration may occur following RYGB with an incidence of 11.4% reported at eight years after surgery. Renal failure and cigarette smoking were the strongest risk factors for this complication in a large US study.32
In a recent study from Western Australia in which Health Data Linkage was used to assess the 24,766 patients who underwent bariatric surgery between 2007 and 2016, 20.2% required at least one bariatric reoperation. Surgical complications were the main indication for reoperation in 67.4% and weight-related in the remainder. Of those who had a single reoperation, the five-yearly rate of having a second revision was 58.2%, a third 38.3% and a fourth revision 45.2%. Patients who had a LAGB were more likely to need an initial revisional operation and those who had revisional surgery had a higher rate of endoscopic procedures and body contouring postoperatively.33
Nutritional deficiencies and dumping syndrome
Adherence to nutritional advice and vitamin and mineral supplementation is crucial to mitigating potential adverse outcomes after bariatric surgery. The increase in insulin secretion, particularly after RYGB, can predispose patients to postprandial hypoglycaemia, which can be minimised by eating small frequent meals containing low glycaemic index carbohydrate. The anatomical changes induced by malabsorptive procedures such as RYGB increase the risk of various micronutrient and vitamin deficiencies, commonly within the first year after surgery. Iron deficiency is frequent, especially in menstruating women, due to bypassing of the duodenum and proximal jejunum and intolerance of iron-rich foods such as red meat.
Vitamin B12 deficiency occurs in up to 30% of patients after RYGB, despite administration of standard multivitamin preparations, because of decreased digestion of protein-bound cobalamins and impaired formation of intrinsic factor. Patients undergoing restrictive procedures such as LAGB and LSG (unlike RYGB), may be maintained postoperatively on a lower-dose daily vitamin B12 supplementation.34 Steatorrhoea induced by malabsorptive surgeries can cause fat-soluble vitamin deficiencies (e.g. vitamin A); patients should be assessed for these at least annually. Restrictive procedures such as LAGB and LSG can induce digestive symptoms, food intolerance or maladaptive eating behaviours that can also lead to protein malnutrition or micronutrient deficiencies.
Dumping syndrome can occur in 70 to 76% of patients after RYGB and leads to abdominal pain, cramping, nausea, diarrhoea, flushing, tachycardia and syncope.34 Recent studies suggest that food bypassing the stomach and entering the small intestine triggers secretion of gut peptides that cause these symptoms. Nutritional modifications, such as eating smaller food portions and avoiding simple carbohydrates, can alleviate symptoms. In severe cases, somatostatin analogues can also be used.34
Bone health
Bariatric surgery can lead to clinically significant loss of bone mass at weightbearing sites such as the hip. In a retrospective cohort study from Minnesota of 258 patients who underwent bariatric surgery between 1985 and 2004 (94% of whom had a gastric bypass, largely RYGB), the relative risk of fracture after a mean follow up of 7.7 years was 2.3-fold higher compared with the age-matched general population.35 In a Taiwanese study assessing 2064 patients who had undergone bariatric surgery between 2001 and 2009 compared with 5027 patients who did not undergo bariatric surgery but with similar obesity and propensity matching, the risk of osteoporotic fracture was increased by 21% in those who had had bariatric surgery. The increased fracture risk was greater with malabsorptive procedures and there was a trend for increased fracture risk to occur at one to two years after surgery.36
Proposed mechanisms include an adaptation to skeletal unloading that is related to the rate and extent of weight loss. Furthermore, longstanding vitamin D deficiency, which is common in patients with obesity, may be exacerbated by malabsorption after bypass surgery. Calcium and magnesium deficiencies can lead to secondary hyperparathyroidism, which has been shown to correlate with cortical bone loss.37 A growing body of literature also implicates changes in circulating concentrations of fat-derived adipokines and gut-derived appetite-regulatory hormones such as peptide YY, GLP-1 and ghrelin in skeletal homeostasis postsurgery.38 Hence, it is crucial that the potential for bone loss is recognised and that vigilant long-term monitoring of bone health is undertaken.
Psychosocial consequences
Mental health problems are prevalent in patients with severe obesity (and vice versa). Poorly controlled depression, substance misuse and eating disorders can compromise surgical outcomes and are frequently regarded as contraindications to bariatric surgery. Consequently, a preoperative psychological evaluation is recommended in most institutions. One systematic review showed the risk of suicide to be fourfold higher among patients after bariatric surgery compared with the background population.39 A cohort study of bariatric surgery, in which 98.5% of patients underwent RYGB, confirmed an increased rate of self-harm emergencies after surgery in patients older than 35 years, those with a low-income status, and those living in rural areas.40 Notably, 93% of the events occurred in patients with an existing mental health disorder that was diagnosed in the five years preceding surgery.40
The Western Australian study referred to previously examined the use of outpatient, emergency department and inpatient mental health services by the 24,766 patients who had bariatric surgery between January 2007 and December 2016. At least one mental health service was used by 16.1% of patients of whom 35.2% presented only before surgery, 25.8% both before and after surgery and 39% presenting only after surgery. There was a fivefold increase in presentations to the emergency department with deliberate self-harm and 25 (9.6%) of the 261 postoperative deaths were due to suicide. Complications after bariatric surgery requiring further surgery and a history of mental health service provision before surgery were the strongest associations with presentation to a mental health facility after bariatric surgery.41
Conclusion
Knowledge of key long-term outcomes of bariatric surgery, such as durability of weight loss, remission of obesity-related comorbidities and surgical complications, has grown exponentially in recent years. Further insights into the physiological mechanisms underlying the outcomes will drive more effective and less invasive techniques that can be individualised to a patient’s needs. Once the appropriate procedure for a patient has been selected, the specific surgical referral pathway should be guided by the familiarity and experience of the surgeon with that procedure. Ultimately, bariatric surgery should be offered to motivated and well-informed patients, especially those with refractory complications of obesity. However, comprehensive medical and psychological evaluation should exclude patients who are at risk of nonadherence or self-harm in the postoperative period. ET