Psoriatic arthritis: the joint and beyond
In psoriatic arthritis, inflammation can extend beyond the joint. Enthesitis and dactylitis are hallmarks of the disease. Extra-articular features, including inflammatory eye and bowel disease, are common. Early treatment with disease-modifying therapy is important to prevent progressive joint damage. It is also important to screen for and manage comorbidities, especially cardiovascular risk factors.
- Psoriatic arthritis is a chronic inflammatory arthritis with diverse musculoskeletal manifestations.
- Extra-articular manifestations are common.
- Comorbidities, particularly metabolic syndrome, cardiovascular risk factors and depression, are often present.
- Early treatment with disease-modifying agents can prevent long-term joint damage and disability.
- Screening for and managing comorbidities is also important.
Psoriatic arthritis (PsA) is a chronic inflammatory arthritis associated with psoriasis. Although the association between psoriasis and joint disease was probably first described in the 19th century, opinion in the medical community was divided, with some believing the condition to be the co-occurrence of rheumatoid arthritis and psoriasis.1,2 PsA was recognised as a distinct entity in 1964 and is now considered part of the seronegative spondyloarthritis group.3,4
Moll and Wright defined PsA as psoriasis associated with inflammatory arthritis and usually a negative serological test result for the presence of rheumatoid factor.5 In 2006, the Classification Criteria for Psoriatic Arthritis (CASPAR criteria) were developed, with improved specificity over previous criteria (Box 1).6 Using the CASPAR criteria, it is possible for patients without a personal history of psoriasis to be classified as having PsA if they have other distinctive features of the condition, although most patients have psoriasis before developing arthritis.
Epidemiology
Estimates of the prevalence of PsA range from 0.001% to 0.43%.7 PsA has been reported in about 30% of patients with psoriasis.8 In contrast to the female predominance seen in rheumatoid arthritis, PsA is equally prevalent in both sexes.5,9 The onset of PsA often occurs between the ages of 30 and 50 years, but juvenile PsA also does occur.10
Clinical features
There is wide variation in the clinical manifestations (Box 2) and severity of PsA.
Musculoskeletal features
Inflammatory arthritis is characterised by joint swelling and stiffness and may involve peripheral joints or the axial skeleton.
Moll and Wright recognised five clinical phenotypes:
- predominantly distal interphalangeal joint involvement
- arthritis mutilans with osteolysis – a severe, deforming arthritis
- symmetrical polyarthritis resembling rheumatoid arthritis
- asymmetrical oligoarthritis
- predominantly spondylitis.5
Peripheral arthritis, either oligoarthritis or polyarthritis, is the most common phenotype.10 Axial disease is reported in up to 40% of patients and may be asymptomatic.9,11
PsA was initially thought to be a less severe disease than rheumatoid arthritis.5 However, it has been shown that, although it often presents as a mild or oligoarticular disease, about 20% of patients with PsA progress to severe polyarticular disease.9 More than half of patients develop joint deformities over time.12 Nevertheless, a proportion of patients do appear to have milder, nonprogressive disease.13
Enthesitis is inflammation at the enthesis, the region where a ligament, tendon or joint capsule attaches to bone. It is a characteristic feature of PsA, and microdamage at the enthesis may be the trigger for activation of the innate immune system, which then stimulates inflammation in the adjacent synovium.14 Frequently involved sites include the Achilles tendon and medial and lateral epicondyles (Figure 1). Enthesitis contributes substantially to pain and poorer quality of life for patients with PsA.15
Dactylitis – inflammation resulting in diffuse swelling of the soft tissues of a digit, producing a ‘sausage-shaped’ finger or toe – is another characteristic feature of PsA (Figure 2).16 However, dactylitis is also seen in patients with other types of spondyloarthritis. It may mimic other conditions, such as cellulitis.
Extra-articular features
Most patients with PsA have psoriasis – only 3% of the cases used to develop the CASPAR criteria did not involve a personal history of psoriasis.6 Skin involvement often precedes the development of articular features by 10 years.17 Psoriatic nail lesions, such as pitting and onycholysis, are associated with the presence of PsA (Figure 3).9
Other extra-articular manifestations include inflammatory bowel disease and inflammatory eye disease, such as uveitis, blepharitis, scleritis and episcleritis (Figure 4).1 In one cohort of patients with PsA, the prevalence of extra-articular manifestations, excluding psoriasis, was 49%, with bowel and ocular involvement the most common manifestations.19 In a systematic review, the prevalence of uveitis in patients with PsA was 25% and was associated with human leukocyte antigen (HLA) B27 positivity.20
Comorbidities
In addition to the extra-articular manifestations of disease, other medical comorbidities, including cardiovascular disease and depression, are common in patients with PsA.21,22 In a study from the Australian Rheumatology Association Database, 57.8% of participants reported having two or more comorbidities, with hypertension (38.2%) and depression (35.9%) the most common.22 In the University of Toronto PsA Clinic, 42.2% of patients had three or more comorbidities.23 Increased comorbidity is also associated with a poorer response to disease-modifying therapy in patients with PsA.24,25
Cardiovascular comorbidities are of particular interest in people with inflammatory rheumatic diseases. In a 2017 meta-analysis, patients with PsA had a 43% increased risk of cardiovascular events, including angina, ischaemic heart disease, coronary artery disease or myocardial infarction, compared with the general population.26 It is thought that the increased risk of cardiovascular disease in people with PsA is partly attributable to common inflammatory pathways in PsA and atherosclerosis.27 PsA is also associated with an increased risk of the metabolic syndrome and other traditional cardiovascular risk factors, including diabetes, hypertension, hyperlipidaemia and obesity.28-32 Furthermore, the metabolic syndrome and insulin resistance have been associated with the severity of underlying PsA.33 Obesity is associated with an increased risk of PsA, and overweight and obese patients with PsA are less likely than normal-weight patients to achieve sustained minimal disease activity.34-37
The European League Against Rheumatism (EULAR) and Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) management guidelines include screening and management for common comorbid conditions. GRAPPA recommends that cardiovascular risk assessment and screening for depression should be strongly considered for all patients with PsA, and that all patients with PsA should be encouraged to achieve and maintain a healthy body weight.11 The EULAR recommendations are that cardiovascular risk assessment and management should be performed in accordance with national guidelines.38,39 A healthy diet, regular exercise and smoking cessation should be recommended.
In a study of Australian patients with PsA or rheumatoid arthritis, relatively few patients with cardiovascular risk factors reported adopting lifestyle modifications.40 GPs have a vital role in screening for and managing cardiovascular risk factors in patients with PsA, including promotion of appropriate behavioural changes, which may both reduce cardiovascular risk and improve arthritis control.
Diagnosis
Early diagnosis and initiation of treatment are important because diagnostic delay predicts poorer outcomes.41 Screening of patients with psoriasis, using tools such as the Early Arthritis for Psoriatic Patients (EARP) questionnaire, may assist in identifying those with early joint disease.42
There is no gold-standard diagnostic test for PsA, with the diagnosis made on the basis of clinical features. Patients with suspected PsA should be referred for specialist review.43 Levels of inflammatory markers (C-reactive protein and erythrocyte sedimentation rate) may be elevated, but more than half of patients with PsA have normal levels.17 Results of tests for rheumatoid factor and anticyclic citrullinated peptide antibody are usually negative in patients with PsA.17 About 25% of patients with PsA test positive for HLA-B27, which is more common in those with axial involvement.44
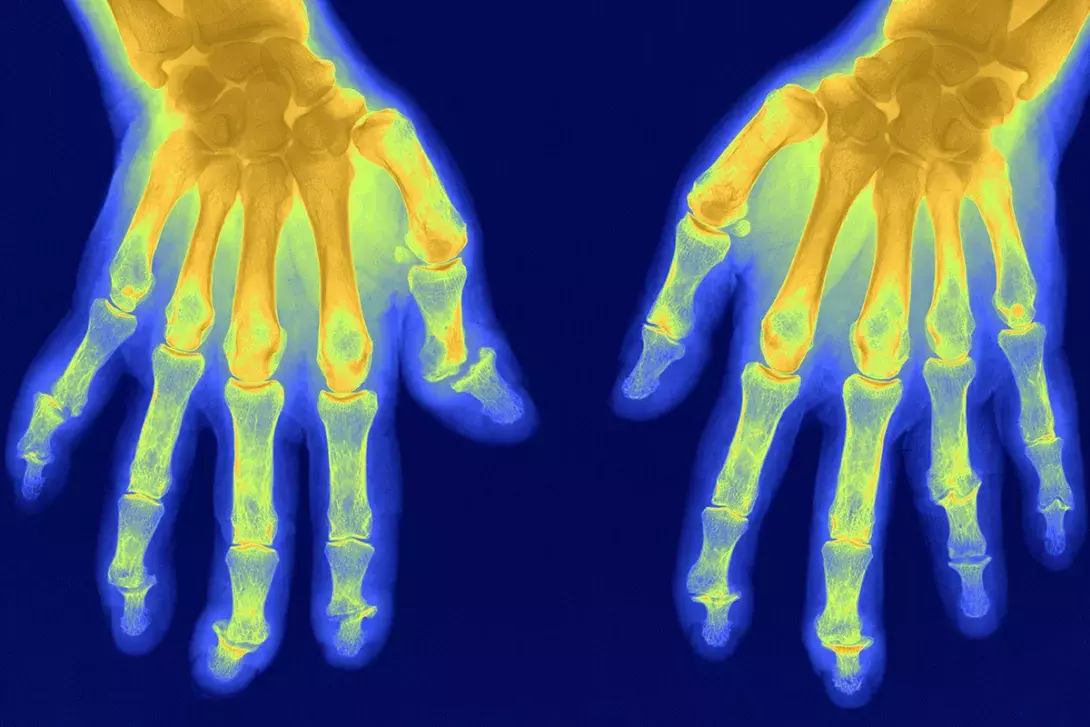
Radiographic imaging may show erosions and new bone formation – periostitis, enthesophytes and ankylosis – that are characteristic of PsA.17 However, plain films may be normal in the early stages of disease, and MRI or ultrasound can be useful to detect synovitis and early erosions.
Management
In addition to nonpharmacological therapies, such as physiotherapy, there is a range of medical therapies available for PsA. Specialist review by a rheumatologist is recommended before starting disease-modifying antirheumatic drugs (DMARDs; Box 3) to control inflammation and prevent joint damage.
The choice of therapeutic agent depends on the phenotype of articular involvement in the individual patient, as well as the extra-articular manifestations, with the aim of treating as many domains as possible.
NSAIDs
NSAIDs can be used for mild peripheral joint symptoms and are the initial choice of drug for patients with spondylitis.11
Corticosteroids
Targeted intra-articular corticosteroid injections may be useful in patients with oligoarticular disease.17 Oral corticosteroids should be used cautiously and at the lowest dose required for efficacy (GRAPPA recommends usually less than 7.5mg prednisone daily) to reduce the adverse effects, including flare of psoriatic skin disease, that can occur after corticosteroid withdrawal.11,45
Conventional disease-modifying antirheumatic drugs
The most frequently used conventional DMARDs for peripheral arthritis are sulfasalazine, methotrexate and leflunomide. Methotrexate is the preferred first agent in patients with clinically relevant psoriasis.45 These DMARDs are also used to treat dactylitis and enthesitis, although evidence of their efficacy for enthesitis is lacking.11 Sulfasalazine is not effective for treating psoriasis, and conventional DMARDs are not effective in treating axial disease.
Biological disease-modifying antirheumatic drugs
Biological disease-modifying antirheumatic drugs (bDMARDs) are recommended for patients whose disease is inadequately controlled with conventional DMARDs. There are strict access restrictions for bDMARD treatment subsidised by the PBS in Australia, and specialist review is required for initiating and continuing treatment with these agents. Available bDMARDS include tumour necrosis factor inhibitors (etanercept, adalimumab, infliximab, golimumab and certolizumab), interleukin 17 inhibitors (secukinumab and ixekizumab) and an interleukin 12/23 inhibitor (ustekinumab). These bDMARDs are effective for both peripheral and axial manifestations of disease and are also used in treating psoriasis.
Targeted synthetic disease-modifying antirheumatic drugs
Targeted synthetic DMARDs include a Janus kinase inhibitor (tofacitinib), which is approved for patients who have inadequate response to conventional DMARDs and has demonstrated efficacy for treating peripheral arthritis, enthesitis, dactylitis and psoriasis.46 Apremilast is a phosphodiesterase 4 inhibitor that has shown moderate efficacy for treating skin and joint disease in patients with PsA, but it is not PBS listed in Australia.45
Pretreatment screening and monitoring for DMARD therapy
Baseline assessment before starting DMARD therapy should include a full blood count, measurement of creatinine level, liver function tests and hepatitis B and C serological tests.47 Screening for HIV should be undertaken if there are relevant risk factors. As there is a risk of reactivation of latent tuberculosis with bDMARD therapy, screening and, if necessary, treatment for latent tuberculosis should be undertaken before beginning bDMARD therapy.48 Regular monitoring of full blood count, creatinine level and liver function tests is recommended for patients receiving DMARD therapy to monitor for adverse effects.47
Conclusion
PsA is a chronic inflammatory arthritis that is associated with extra-articular features, including skin, eye and bowel disease. Early specialist referral and initiation of treatment are important to prevent joint damage and disability. The long-term management of this chronic disease is shared between specialists and GPs. Patients require regular review for changes in disease activity and monitoring for adverse effects of DMARDs.
Patients with PsA are also at increased risk of comorbidities, including obesity, cardiovascular disease and depression, and should receive screening and management for these conditions. MT
