Obesity – a growing issue for male fertility
Obesity in men has been associated with reduced fertility. The impact of paternal body mass index on fertility is multifactorial, with increased weight associated with endocrine dysregulation and impaired sexual desire and function. Weight loss may improve fertility outcomes as well as conferring longer-term health benefits.
Obesity is a growing health issue that causes substantial morbidity and mortality. Epidemiological data suggest an association between increasing body mass index (BMI) and reduced fertility in men, with one study suggesting that a gain of 10 kg decreases male fertility by approximately 10%.1 The effect of BMI on male fertility is multifactorial, with increased weight associated with changes in sex hormone profile and impaired sexual desire and function. Some studies also suggest poorer semen parameters in overweight men.
Despite the prevalence and costs of male subfertility, there are few data regarding the fertility benefits of weight loss in men. Although weight reduction may normalise the hormone profile, the extent that this improves fertility and the time course of any improvement are unclear.
Factors contributing to subfertility in men with obesity
Increased BMI is strongly associated with both hormonal dysregulation and poorer sexual function in men, which can impair fertility, as outlined in the Figure.
Hormonal dysregulation
Excess body weight has numerous effects on the reproductive hormone profile in men, leading to:
- a relative excess of oestrogen
- resultant suppression of hypothalamic secretion of gonadotrophin-releasing hormone (GnRH)
- reduced serum levels of gonadotrophins (luteinising hormone and follicle stimulating hormone)
- reduced serum testosterone levels.
Furthermore, there may be a feedback effect as there is a well-recognised association between hypogonadism and the metabolic syndrome, which itself is associated with increased weight.
Effects on testosterone
BMI is a strong predictor of low serum total testosterone concentrations in men, with a clear inverse correlation shown in many studies. BMI is also inversely proportional to free testosterone concentrations, suggesting an association even after accounting for lower sex hormone binding globulin levels due to insulin resistance.2
Effects on other reproductive hormones
Low serum testosterone in overweight men is associated with inappropriately low-to-normal levels of gonadotrophins. This reversible hypogonadotrophic hypogonadism includes hyperoestrogenism as a significant component. Androgens are converted to oestrone and oestradiol by the aromatase enzyme in adipose tissue. In overweight men, the increased adipose tissue mass and upregulation of aromatase activity lead to excess peripheral aromatisation of androgens. The resulting hyperoestrogenism exerts a negative feedback effect on hypothalamic GnRH pulses, reducing stimulation of gonadotrophin secretion. Circulating oestrogens may also have a direct adverse effect on testicular function. In addition, circulating endogenous opioids are likely to have a pathophysiological role in the development of hypogonadotrophic hypogonadism in overweight men.
Reduced libido and erectile dysfunction
Although hormonal dysregulation may affect semen quality, as described below, the primary reasons for the reduced fertility rate observed in men with obesity may be decreased sexual desire and impaired sexual function. Potential contributing factors include androgen deficiency, organic causes of erectile dysfunction (ED) and psychosocial factors.
Men with obesity report poorer sexual desire and satisfaction compared with control subjects, which may contribute to avoidance of sexual encounters.3 Overweight individuals are more likely to have chronic medical comorbidities and to be of lower socioeconomic class with resulting financial or domestic problems that can reduce libido. Depressive illness is also more common, and correlates with both low libido and ED. Low libido ultimately results in reduced coital frequency, lowering fertility rates.
In addition, sexual dysfunction is an important contributor to subfertility, with the presence of ED being correlated with lower fertility rates in men. ED is more prevalent in men with higher BMI. Its aetiology in this setting is multifactorial, including androgen deficiency and vasculogenic dysfunction.
Medical comorbidities such as the metabolic syndrome are significantly associated with ED. Both diabetes and hypertension are associated with vascular dysfunction, and diabetes may also lead to neuropathic complications. Furthermore, obstructive sleep apnoea (OSA) is more common in men with obesity and is strongly independently linked with both ED and androgen deficiency.
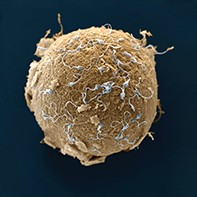
Reduced sperm quality
Effect of BMI on semen parameters
The relationship between BMI and subfertility is not completely explained by obesity-associated sexual dysfunction and reduced frequency of intercourse. Changes with increased BMI, including hormonal imbalance and increased testicular temperature, may impair semen parameters.
A recent systematic review and meta-analysis demonstrated an association between increased BMI and modest decreases in sperm motility, morphology and concentration,4 whereas earlier reviews have failed to establish this correlation.5 The association between BMI and sperm DNA fragmentation has also been investigated. DNA fragmentation may correlate with poorer sperm quality and integrity, and consequently be associated with reduced fertility and an increased incidence of subsequent miscarriage. Although some studies have demonstrated increased fragmentation in men with severe obesity,6,7 other studies have not reliably reproduced these findings.6-8 Additionally, mouse models suggest that paternal obesity may have metabolic sequelae and lead to subfertility and other metabolic effects in offspring through epigenetic effects.9
Effect of BMI on assisted reproductive technology outcomes
With the increasing use of assisted reproductive technology, the impact of paternal BMI on their outcomes is pertinent. Increased paternal BMI has been associated with reduced chemical and clinical pregnancy rates, as well as lower live-birth rates.8,10,11 This may be a result of sperm dysfunction that is not detectable by standard analysis. In addition to effects on implantation and pregnancy rates, there have also been suggestions that paternal obesity may have an impact on blastocyst development, possibly as a consequence of sperm DNA damage.
Lifestyle and environmental factors
A range of potentially remediable lifestyle factors can affect fertility and should be addressed in all men with subfertility. Some of these factors, such as a sedentary lifestyle, are associated with obesity.
Sedentary lifestyle. Prolonged sitting, in combination with increased lower abdominal and scrotal fat deposition, might adversely affect sperm production by increasing testicular temperature.
Tobacco. Tobacco use has a modest dose-dependent effect on sperm quality, with lower sperm concentration and poorer sperm motility and morphology seen in smokers.12,13 Furthermore, smoking may decrease the success rate of assisted reproductive technologies, including in vitro fertilisation and intracytoplasmic sperm injection. Sperm isolated from smokers have poorer function and higher DNA fragmentation, suggesting a direct detrimental effect of tobacco on sperm DNA. These outcomes may be reversible within a year of tobacco cessation.
Alcohol. Heavy alcohol use may be associated with hypogonadism, poorer sperm quality and sexual dysfunction.
Cannabis. It has been suggested that cannabis may activate cannabinoid receptors located on sperm and the paraventricular nucleus of the hypothalamus. These receptors are believed to be responsible for regulating sperm motility, and sexual and erectile function, respectively. Although cannabis use has been linked with abnormal sperm motility and impaired fertility in male mice,14 human studies are limited. In vitro studies demonstrate a dose-dependent negative effect on sperm motility and function, whereas the impact on sexual function is less conclusive, with some studies reporting enhanced sexual pleasure with cannabis use, but others report impaired erectile function.15
Management of men who are overweight with subfertility
Patient assessment
Assessment of overweight men with subfertility should include a basic fertility assessment to ensure that other causes of male subfertility are not overlooked.16 The potential contribution of female factors must also be considered. A male fertility assessment tool developed by Healthy Male is available for free download at: www.healthymale.org.au/health-professionals/clinical-resources/patient- assessment-tools. Points to cover in a fertility assessment of overweight men are summarised in the Table.
In addition to the basic fertility assessment, evaluation of overweight men should focus on identifying obesity-associated comorbidities and lifestyle factors that may play a significant role in the aetiology of subfertility as well as confer significant cardiovascular risk. Cardiovascular assessment should include inquiring about erectile dysfunction, measuring blood pressure and screening for diabetes and dyslipidaemia. The importance of ED as an independent risk factor for metabolic syndrome and cardiovascular disease is increasingly being recognised, with ED representing a surrogate biomarker for endothelial dysfunction and atherosclerosis. OSA and depression should also be considered in all men who are overweight.
The initial assessment of a couple with subfertility by a GP can expedite their evaluation and ensure they are referred to an appropriate specialist, such as an endocrinologist and/or a gynaecologist specialising in assisted reproductive technology.
Treatment
There are limited data regarding the fertility outcomes of interventions in men with obesity. Nevertheless, a patient consultation about fertility is an opportunity for a GP to establish a therapeutic relationship with the patient and to promote lifestyle modifications and weight loss that will have long-term cardiovascular benefits. These include tobacco cessation, avoidance of excessive alcohol and promotion of moderate exercise. Identified comorbidities, such as diabetes, dyslipidaemia and OSA, should also be treated. Treatment of OSA with continuous positive airway pressure (CPAP) has been shown to increase testosterone levels.
Weight loss
Weight loss can reverse the hormonal abnormalities seen in overweight men, while also improving comorbidities such as OSA.17 Biochemical changes that correlate with weight loss include increases in serum testosterone and sex hormone binding globulin levels and decreases in oestradiol levels. Nonsurgical approaches to weight loss include low-calorie diets, increased physical exercise and sometimes pharmacological therapy to help maintenance of weight loss. Bariatric surgery allows greater and more sustained weight loss. Reduced BMI in men after bariatric surgery has been shown to improve their sexual desire and satisfaction, as well as erectile function.18
There is emerging evidence to suggest a beneficial effect of weight loss through lifestyle modification on sperm parameters including DNA fragmentation.19 The impact of bariatric surgery is less clear, with some studies demonstrating reduced sperm defragmentation following surgery, whereas others have observed decreased or no impact on sperm concentration and/or motility.20,21
Importantly, the effects of paternal obesity on spermatogenesis are likely to be at most modest, with most male subfertility and significant sperm defects being a result of intrinsic disorders of spermatogenesis rather than solely attributable to BMI. It would thus be remiss to overstate the effects of overweight on fertility and to rely exclusively on weight loss as a cure for subfertility in men with obesity.
Other treatments
Although weight loss improves the hormone profile, there are few data regarding therapies that directly target endocrine abnormalities in men with obesity. Aromatase inhibitors might potentially correct oestrogen excess and ameliorate hypogonadotrophic hypogonadism, but this intervention has not been well studied in men with obesity, and these drugs are not approved for this indication. Notably, even in the presence of hypogonadism, exogenous androgens should not be prescribed in men with obesity seeking fertility because of their contraceptive action.
Other potential therapies include the use of phosphodiesterase inhibitors to improve erectile function. Scrotal lipectomy to remove accumulated fat has been advocated to reduce scrotal temperature.
Conclusion
Male obesity is a significant health issue and is associated with decreased fertility. The association is likely to involve multiple factors, including endocrine dysregulation, reduced sexual desire and function, comorbidities such as OSA, and suboptimal semen parameters. Although there are limited data demonstrating the direct benefits of weight loss on semen parameters and sperm quality, weight loss has been shown to improve the hormone profile and is linked with improved sexual function. Importantly, a consultation about fertility provides a rare opportunity for GPs to engage with men who have obesity about their weight, lifestyle choices and cardiovascular health. Practice points regarding male obesity and fertility are summarised in the Box. MT