Two PCSK9 inhibitors now PBS-subsidised for cholesterol control
Proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors appear to be safe and effective drugs to reduce elevated low-density lipoprotein cholesterol levels, but they will not replace conventional therapy. Two PCSK9 inhibitors, alirocumab and evolocumab, are now PBS-subsidised for patients with familial and nonfamilial hypercholesterolaemia who are at high cardiovascular risk. Because of cost constraints, patients must satisfy strict PBS criteria.
Blood lipid abnormalities, especially raised levels of low-density lipoprotein cholesterol (LDL-C), are causally related to atherosclerotic cardiovascular disease (CVD). Selected lipid interventions have been shown to reduce CVD risk. The evidence is strongest for statin drugs (i.e. inhibitors of HMG-CoA reductase),1 but also exists for the non-statin drug ezetimibe.2 The broader subject of lipid therapy was recently reviewed by this author.3
Epidemiological studies suggest that lipid therapy will likely reduce the relative risk of CVD by about 50% if started early enough and administered over many years. Relative risk reductions in outcome trials are necessarily much smaller, as these studies occupy just a few years. Whether we consider secondary or primary CVD prevention, there remains considerable residual CVD risk despite conventional lipid and other therapy. This residual risk may be attributed, in part, to a continuing excess of LDL-C and other lipoproteins, and to other remaining risk factors. In addition, a small proportion of patients is unable to tolerate a full or any dose of statin.4
Role of PCSK9 inhibition
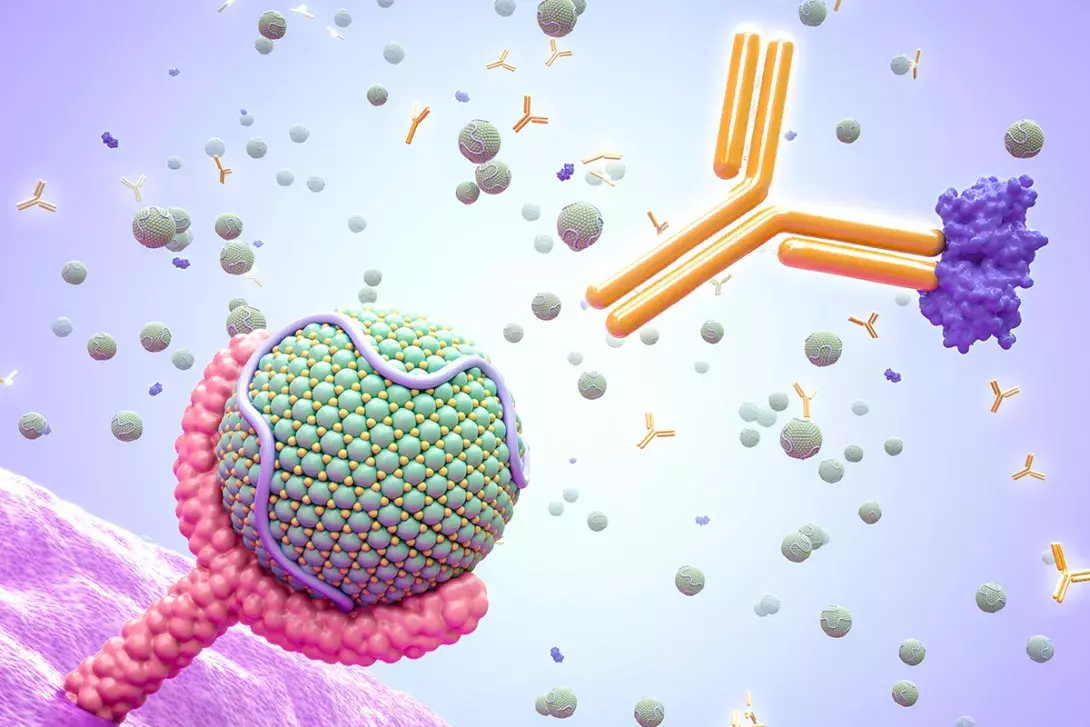
A previous report in Medicine Today highlighted the role of inhibitors of the enzyme proprotein convertase subtilisin-kexin type 9 (PCSK9) in regulating LDL-C levels.5 Loss-of-function mutations in the gene coding for PCSK9 are associated with low LDL-C levels and reduced coronary risk.6 PCSK9 regulates LDL-C by promoting the degradation of LDL receptors, thereby diminishing tissue uptake of LDL-C from the bloodstream. Hence, inhibition of PCSK9 has become a new therapeutic target for lowering LDL-C.
Alirocumab and evolocumab are fully human monoclonal antibodies to PCSK9. Alirocumab is licensed in Australia for patients with familial heterozygous hypercholesterolaemia and for nonfamilial hypercholesterolaemia. Evolocumab is similarly licensed, but additionally for the extremely rare cases of familial homozygous hypercholesterolaemia.
Both alirocumab and evolocumab are usually self-injected subcutaneously using a disposable prefilled, fixed-dose ‘pen’. The starting dose of alirocumab is 75 mg every two weeks and LDL-C response should be evaluated within four to eight weeks. The dose may then be increased to 150 mg every two weeks if the LDL-C response is inadequate. Evolocumab is given in a fixed dose of 140 mg every two weeks, with no further dose titration.
Alternatively, either drug may be administered once every four weeks, but required doses are higher and will sometimes require multiple injections. Most patients seem to prefer a single injection every two weeks. The maximum reduction in LDL-C is achieved when a PCSK9 inhibitor is used in combination with a statin and/or ezetimibe, where this is feasible.7
What is the evidence of clinical benefit?
Early studies with PCSK9 inhibitors showed reductions in LDL-C level of about 50% and this was additive to the effect of any concurrent statin therapy.7 In large secondary prevention trials involving patients already receiving statins, both evolocumab and alirocumab significantly reduced the relative risk of a first event in a composite CVD outcome by a further 15% compared with placebo injections.8,9 Treatment with either inhibitor was well tolerated and adverse event rates were similar to placebo, except for a slight excess of injection-site reactions. Treatment did not increase the risk of new-onset diabetes and was effective in the presence or absence of diabetes.10,11
Alirocumab reduced all-cause mortality by a nominally significant 15%, but surprisingly without a significant change in coronary heart disease mortality.9 No significant change in all-cause mortality was found with evolocumab.8 In general, other lipid interventions of similar design have not shown a major effect on all-cause mortality and such findings with PCSK9 inhibitors should be viewed with caution.
Outcome studies are traditionally evaluated using only the first in-trial CVD event, meaning that subsequent CVD events are ignored. The ODYSSEY OUTCOMES trial with alirocumab was recently re-evaluated to include all CVD outcomes during the trial, not just a first event.9,12 The total number of nonfatal CVD events and deaths prevented was twice the number of ‘first events’ prevented.
The FOURIER outcome trial with evolocumab, studying patients with stable coronary artery disease, found greater clinical benefit in patients with more residual, multivessel coronary disease.8,13 The ODYSSEY OUTCOMES trial with alirocumab, studying patients with a recent acute coronary syndrome, also found larger absolute clinical benefit in patients having disease in multiple arterial beds.9,14 DNA analyses in these same outcome studies have indicated that those patients at higher genetic risk have the highest rates of subsequent CVD events and may have the greatest event reductions.15,16
There are no similar clinical trial data available in the context of primary CVD prevention. However, the use of PCSK9 inhibitors is permitted in such patients at high CVD risk, but on an empirical basis.
Lipoprotein(a) and PCSK9 inhibitors
Lipoprotein(a) [Lp(a)], a unique, genetically determined component of the LDL particle, is increasingly recognised as a risk factor for CVD.17 Elevated Lp(a) levels confer increased CVD risk, especially in those with highest LDL-C levels.18,19 Elevated Lp(a) levels are reduced by about 25 to 30% with the use of PCSK9 inhibitors.20,21
Both the evolocumab and alirocumab outcome trials showed greater CVD event reduction in patients having higher Lp(a) levels at study entry.20,21 These findings do not prove that reducing Lp(a) lowers CVD risk but suggest that patients with elevated Lp(a) might be a priority group to receive PCSK9 inhibitors.
The future
PCSK9 synthesis may also be reduced through injection of small interfering RNA. Known as inclisiran, this is also given by subcutaneous injection, effectively reduces LDL-C levels and may only need administration every six months.22 The results of CVD outcome studies are awaited.
A recent meta-analysis of PCSK9 inhibition in patients with familial heterozygous hypercholesterolaemia showed little heterogeneity in the LDL-C lowering effect of different drugs.23
Alicrocumab, evolocumab and the PBS
PCSK9 inhibitors, largely because of their high cost, will generally be used as a supplement to conventional treatment in patients needing further help to reach LDL-C targets. They may also be used as solo drug therapy (or combined with ezetimibe) in patients intolerant to statins.
Evolocumab and alirocumab are now both PBS-subsidised in Australia for patients with familial heterozygous hypercholesterolaemia or nonfamilial hypercholesterolaemia at high cardiovascular risk (i.e. in patients with atherosclerotic disease and/or very high LDL-C levels, or meeting other high-risk criteria). Patients must have LDL-C levels that are not adequately controlled with maximum recommended or tolerated doses of atorvastatin or rosuvastatin and ezetimibe, or where statin therapy is contraindicated.24 Evolocumab is also PBS-subsidised for familial homozygous hypercholesterolaemia. The PBS subsidy guidelines for PCSK9 inhibitors are quite complex and practitioners are advised to consult detailed PBS guidelines or prescription software.24 The initial PBS authority application must be made by a specialist physician, but repeat prescriptions may be provided by any medical practitioner using streamlined authority.
Patients ineligible to receive an inhibitor of PCSK9 under PBS subsidy may purchase the item on private prescription but at major personal cost.
Conclusion
PCSK9 inhibitors appear to be safe and effective drugs to reduce elevated LDL-C levels, but they will not replace conventional therapy. Outcome studies confirm significant future CVD event reduction with alirocumab and evolocumab in patients with prior CVD already using statin therapy, especially in those with elevated Lp(a) levels. Use of PCSK9 inhibitors in primary prevention in patients at high risk of CVD is also justified, but on an empirical basis. Alirocumab and evolocumab are both PBS-subsidised for patients with familial or nonfamilial hypercholesterolaemia at high cardiovascular risk. Because of cost constraints, patients must satisfy strict PBS criteria. MT
This article is for general information purposes only, and the full product information should be consulted before prescribing any of the mentioned medications.
