Scalp pruritus – scratching for answers
Scalp itch is common in people of all ages. Treatment depends on an accurate diagnosis. Causes range from everyday skin conditions such as seborrhoeic dermatitis, psoriasis and head lice to rare disorders such as dermatitis herpetiformis and trigeminal trophic syndrome.
- Scalp pruritus is a feature of many common dermatological conditions, including seborrhoeic dermatitis, psoriasis, pediculosis capitis, atopic dermatitis or eczema, lichen simplex chronicus and contact dermatitis.
- Scalp pruritus may also be a prominent feature of rare conditions such as dermatitis herpetiformis, lichen planopilaris and trigeminal trophic syndrome.
- Pruritus of the scalp can occur without any discernible skin changes; psychological issues can exacerbate or manifest as scalp pruritus.
- Scalp pruritus can be a diagnostic and therapeutic challenge; distinguishing features in the patient’s history should be sought and physical examination should include whole-body skin inspection.
- Sometimes a therapeutic trial is required before the diagnosis is established.
- A definitive cause for scalp pruritus is not always found; these patients may benefit from symptomatic antipruritic treatments.
- Referral to a dermatologist is recommended when the diagnosis remains unclear or the disease does not respond to treatment. Early dermatology referral is essential for patients with dermatitis herpetiformis, lichen planopilaris and alopecia.
Scalp pruritus is a frequent presentation to GPs. This article outlines the clinical features and treatment of common dermatological conditions associated with scalp pruritus, as well as some rare but important causes of this condition. A summary of the common causes of scalp pruritis is listed in Table 1; a summary of less common causes of scalp pruritus are listed in Table 2 & 2b.
Common causes of scalp pruritus
Seborrhoeic dermatitis
Clinical features
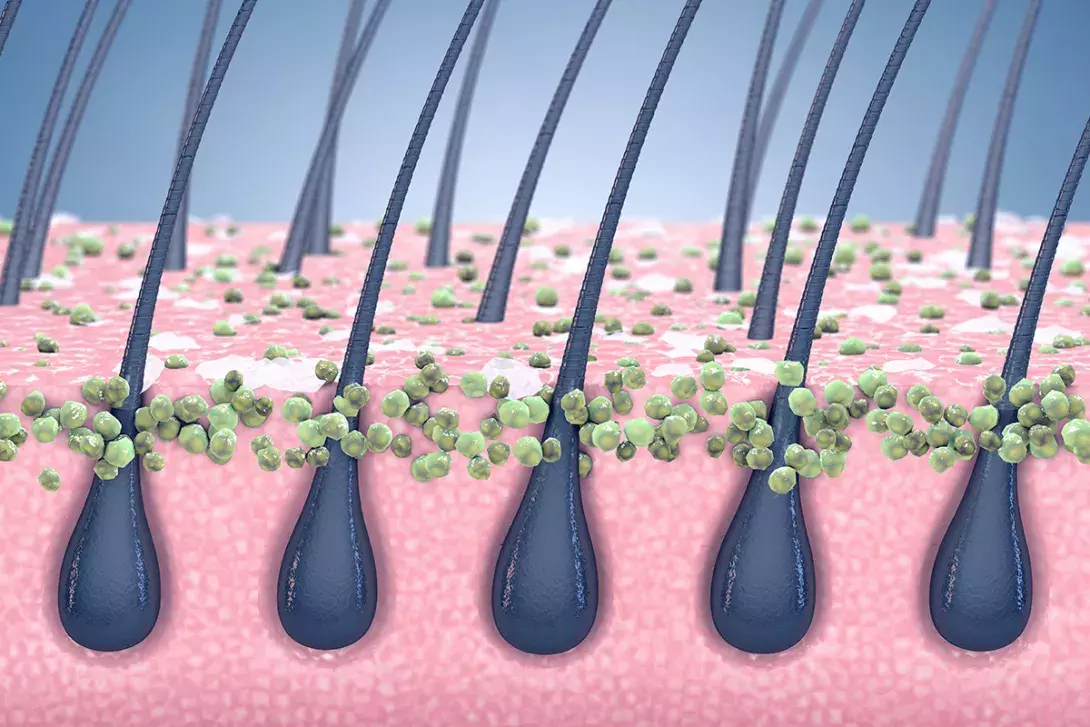
Seborrhoeic dermatitis is a common dermatosis with a predilection for sites of increased sebum production, including the scalp, ears, face, central chest and major body folds (Figures 1a and b). Although the cause of seborrhoeic dermatitis remains unknown, the commensal yeast Malassezia furfur has been implicated in its pathogenesis.
Infantile and adult forms are distinguishable. The infantile form, commonly known as ‘cradle cap’, occurs in the first three months of life and is self-limiting. The adult form tends to begin in late adolescence and persist into adulthood, with peak prevalence in the third and fourth decades.
Seborrhoeic dermatitis has an estimated prevalence of 3% in the general population. For reasons that are not completely understood, seborrhoeic dermatitis is more common in individuals with HIV infection and neurological disorders, notably Parkinson’s disease. Indeed, severe or recalcitrant seborrhoeic dermatitis may be the presenting sign in patients with HIV infection.
In its mildest form, seborrhoeic dermatitis of the scalp is referred to as dandruff (also called pityriasis capitis), and is characterised by diffuse, fine white scaling without inflammation. With more extensive disease, greasy yellow to salmon- coloured scales overlay patches of inflamed skin (Figure 1a). Areas of affected skin may be asymptomatic or extremely itchy. Seborrhoeic dermatitis can mimic psoriasis but, in the latter, plaques are well demarcated, thicker and more inflamed (Figures 2a and b). The presence of nail changes and plaques elsewhere on the body in psoriasis can help differentiate it from seborrhoeic dermatitis (Figure 2c).
Seborrhoeic dermatitis may be associated with blepharitis and facial rash (Figure 1b). The rash may extend to involve the postauricular region with fissuring, as can otitis externa. Other areas, such as the axillae and groin, may show a glazed erythema with little scaling.
Treatment
Seborrhoeic dermatitis is a chronic relapsing condition, and patients need to be reminded that treatment aims to control, not cure. In mild cases, regular use of an antidandruff shampoo is usually effective. Examples are shown in the Box. The shampoo should be massaged into the scalp and left for about five minutes before rinsing out. Washing the shampoo out too soon or not using it often enough are common causes of treatment failure. For more difficult cases, a topical antifungal preparation such as a ketoconazole cream may be used in addition to a shampoo. The cream is mixed with water and massaged into the scalp at night and washed out the next morning.
Patients with a greater degree of inflammation will benefit from the addition of a topical corticosteroid. Corticosteroid lotions are the easiest form to apply to hair-bearing areas and include methylprednisolone aceponate 0.1% and mometasone furoate 0.1% lotions. These can be used as needed.
When the scalp is thickly covered with scale, preparations such as extemporaneously compounded coal tar and keratolytics such as liquor picis carbonis (LPC) 3 to 6% with salicylic acid 3% in aqueous cream are beneficial.
Systemic antifungal agents such as itraconazole, terbinafine or fluconazole should be reserved for patients with severe or unresponsive disease. The quality of evidence examining the clinical efficacy of oral treatments in patients with seborrhoeic dermatitis is low, and there is no direct comparison between treatments.1
Psoriasis
Clinical features
Psoriasis is a chronic, immune-mediated papulosquamous skin condition that is common in Australia, with an estimated prevalence of 2 to 6%. Psoriasis is a polygenic disorder that is influenced by a variety of environmental factors, such as trauma, medication and infection. The classic features – erythema, thickening and scale – are the result of abnormal keratinocyte proliferation and differentiation, vascular dilation and a population of inflammatory cells within the dermis and epidermis.
The scalp is involved in more than half of patients with psoriasis, and in some instances this may be the sole manifestation. Scalp psoriasis is characterised by well-demarcated erythematous plaques that have an adherent silvery scale. Lesions may advance beyond the hairline and extend to involve the retroauricular area (Figures 2a and b). In milder cases, scaling may be diffuse and nonspecific, and resemble pityriasis capitis. Psoriasis of the scalp seldom results in alopecia.
Psoriasis is a systemic disease process associated with a number of comorbidities. Psoriatic arthritis is the major systemic manifestation, affecting up to 30% of patients, and scalp psoriasis is a sign of increased risk of psoriatic arthritis. Patients have an increased risk of developing metabolic syndrome, cardiovascular disease, mental health issues, inflammatory bowel disease and certain malignancies, such as non-melanoma skin cancers, thus it is important to screen for and manage this vast range of comorbidities.2
Treatment
Medicated shampoos may be effective for mild cases of scalp psoriasis. These preparations contain active ingredients such as tar and salicylic acid. For moderate to severe scalp psoriasis, topical corticosteroids are the mainstay of treatment. Potent and very potent topical corticosteroids are suitable for scalp psoriasis. Start with a topical corticosteroid lotion such as mometasone furoate 0.1% or methylprednisolone aceponate 0.1%; these can be applied to the scalp after shampooing and left overnight. Topical corticosteroid treatment is more efficacious when combined with calcipotriol, a vitamin D derivative.3 A combination product containing calcipotriol and betamethasone was available on PBS; however, it has recently been discontinued. Another treatment option is clobetasol propionate 0.05% shampoo, which is also available on the PBS for this indication. This is applied to the scalp for five to 15 minutes, then rinsed out, initially daily then once to twice a week for maintenance.
Patients with thickened plaques and adherent scale require a keratolytic preparation. This is usually left on overnight and washed out the next morning. A typical preparation may include a combination of a tar (e.g. 3 to 10% LPC) and salicylic acid 3 to 5% (maximum 10%) in aqueous cream, extemporaneously compounded.
In more severe cases, dithranol at a concentration of 0.1 to 0.2% can be added to compounded preparations for overnight application to the scalp. Higher concentrations of dithranol (0.5 to 1%) can be used for short contact treatment, applied and left for no more than 30 minutes before being washed off. Short-contact treatment can be very irritating to inflamed skin. Preparations containing dithranol and tars should be used with caution by fair-haired individuals as they can stain the hair. Dithranol’s propensity to cause red–brown staining and skin irritation has contributed to a decline in its use.
Systemic therapy, such as methotrexate, acitretin, ciclosporin, or biologic therapy, can be used in patients with treatment-resistant scalp psoriasis. Methotrexate can be prescribed by GPs; however, other systemic therapies, such as ciclosporin, acitretin (except in Western Australia) and apremilast must be prescribed and managed by a dermatologist. Referral to a dermatologist is indicated when topical treatments and methotrexate (if the GP is comfortable prescribing this) are unable to provide adequate disease control and additional therapy is required.
Biologic therapy including tildrakizumab (IL-23 inhibitor), guselkumab (IL-23 inhibitor), risankizumab (IL-23A inhibitor), etanercept (TNF inhibitor), adalimumab (TNF-alpha inhibitor), infliximab (TNF-alpha inhibitor), secukinumab (IL-17A inhibitor), and ixekizumab (IL-17A inhibitor) be used in severe scalp and generalised psoriasis.4 Biologic therapy is PBS subsidised for severe, treatment resistant psoriasis and must be prescribed by a specialist dermatologist.
Pediculosis capitis (head lice)
Clinical features
Infestation of the scalp by the head louse is common, especially in children. Infestation is typically acquired by direct head-to-head contact, after which the female louse lays eggs (nits) – usually five to 10 per day – cemented to the base of hair shafts. Viable eggs appear tan to brown, whereas empty eggs are clear to white. Nits are difficult to dislodge from hair shafts, distinguishing them from seborrhoeic scales and hair casts, which glide easily along the shaft. Clinically, patients with head lice present with itch that is prominent over the occipital and parietal scalp, where infestation tends to be greatest. Papules are occasionally observed (Figure 3a). There may be secondary impetiginisation and hairs matted down by exudates.
Diagnosis is through direct visualisation of eggs or adult lice (Figure 3b). These are best detected by combing the hair systematically with a fine-toothed comb.
Treatment
There is a lengthy list of treatments available for head lice, but little high-quality evidence comparing their effectiveness. Topical pediculicides remain the choice of treatment in Australia. First-line topical agents include permethrin 1%, malathion 0.5% or 1% and pyrethrins 0.165% piperonyl butoxide 1.65%.5 Chemical pediculicides have limited ovicidal activity and thus a second application, seven days after the first, is advisable to kill newly hatched nymphs.
Oil-based pediculicides are an alternative. Examples include melaleuca (tea tree) oil 10% plus lavender oil 1% and eucalyptus oil 11% plus lemon tea tree oil 1%. Lotions or liquid preparations are preferred because they are more effective than shampoos. The entire family should be treated at the same time to prevent cross infection.
A fine-toothed comb is required to remove nits. Evidence supports ‘wet combing’ combined with a lavish amount of hair conditioner as an effective treatment for lice.6 Conditioner is applied to wet hair in order to ‘stun’ the lice and then swept in a systematic fashion through the hair with a fine-toothed comb.
Wet combing should be used the day after application of a topical pediculicide to assess treatment success. If the pediculicide has been applied appropriately then the detection of live lice indicates treatment resistance. Widespread pesticide resistance has emerged and patterns vary with geographic location, even between schools in the same city.7 When pesticide resistance is suspected, swapping to an alternative topical pesticide is recommended. For head lice infestations refractory to topical treatment options, oral ivermectin 200 mcg/kg is prescribed as a single dose, with a repeat dose given seven days later.8 This should still be combined with topical therapies.
Lichen simplex chronicus
Clinical features
Lichen simplex chronicus is a secondary skin disorder, in which repetitive scratching or rubbing gives rise to lichenified plaques (Figure 4). These can be solitary or multiple. Lesions have a dry or scaly surface, and normal skin markings are accentuated giving the skin a ‘leathery’ appearance. Rubbing may result in secondary broken hair shafts or apparent alopecia. Skin changes occur at sites accessible to scratching, including the occipital scalp and posterior neck. Involvement of the lower legs, scrotum or vulva and extensor forearms should be sought.
Lichen simplex chronicus is common in adults with atopic dermatitis. Other predisposing factors include neuropathic pruritus and psychological conditions such as anxiety and obsessive compulsive disorder.
Lichen simplex chronicus can be diagnosed through its characteristic clinical appearance. If there is diagnostic uncertainty then examination of a skin biopsy specimen can help exclude lichen planus, lichen amyloidosis and psoriasis.
Treatment
The primary objective in treating lichen simplex chronicus is to break the itch–rub cycle. Potent topical corticosteroid lotions such as methylprednisolone aceponate and mometasone furoate are the mainstay of treatment. In patients with resistant lichen simplex chronicus, topical corticosteroids can be used in combination with intralesional triamcinolone. It is important to manage psychological stressors that perpetuate compulsive scratching and rubbing.
Less common causes of scalp pruritus
Tinea capitis
Tinea capitis is a dermatophyte infection of the scalp that occurs primarily in children. The causative organism varies with geographic location. In Australia, Microsporum canis and Trichophyton tonsurans predominate. There have been increasing reports of tinea capitis caused by Trichophyton soudanense (Figure 5), Trichophyton violaceum and Microsporum audouinii in immigrant children from East Africa, and confirmation of transmission to local populations.9
The two main patterns of tinea capitis invasion are: ectothrix and endothrix. In ectothrix infection (e.g. M. canis infection), arthroconidia (fungal spores) surround and destroy the cuticle, resulting in annular patches of partial alopecia. In endothrix infection (e.g. T. tonsurans infection), the arthroconidia are found within the hair shaft. This weakens the cuticle, and the hair breaks off level with the follicular orifice giving rise to ‘black dot’ tinea capitis in patients with dark hair. Inflammation varies from a fine scale to kerion formation, characterised by a boggy, purulent mass.
Clinical diagnosis of tinea capitis can be difficult owing to its varied presentation. An approach is to consider and exclude a fungal infection in patients (especially children) with hair loss and scale. To confirm the diagnosis, six to eight hairs should be plucked for fungal culture and microscopy.9 A Wood’s lamp is helpful in identifying tinea capitis only when the causative organism fluoresces (e.g. M. canis), as not all dermatophytes exhibit this phenomenon.
Treatment of tinea capitis requires oral antifungals, as topical therapy alone is rarely successful. Current evidence supports terbinafine for empiric treatment of tinea capitis caused by Trichophyton or griseofulvin for tinea capitis caused by Microsporum spp.10 Oral griseofulvin is given at a recommended dose of 20 mg/kg/day up to 500 mg orally for a minimum of six to eight weeks, or until a clinical and mycological cure is achieved. Terbinafine is given to adults at a dose of 250 mg once daily, and to children at a recommended dose of 62.5 mg (body weight under 20 kg) or 125 mg (body weight 20 to 40 kg) once daily for four weeks.11-13 Terbinafine is available on the PBS for children with tinea capitis only when initial treatment with griseofulvin has failed. Side effects are comparable between griseofulvin and terbinafine; nasopharyngitis, headache and pyrexia are most common.14 Concurrent use of ketoconazole or selenium sulfide shampoo can help prevent spread.10 Alternative oral agents include itraconazole and fluconazole, but these are suboptimal choices for Trichophyton infections.11 Culture should be repeated at the end of treatment to confirm microbiological cure.
Contact dermatitis
Scalp pruritus can be caused by contact dermatitis, due to either an irritant or an allergen. The scalp is relatively resistant to contact dermatitis because of rapid epidermal turnover and a thick epidermis and stratum corneum. It is also well protected by hair. Often the ears, forehead, neck or face are affected first.
Major allergens are found in hair dyes (e.g. paraphenylenediamine), bleaches, permanent wave solutions and hair creams. Potential irritants include bleaching agents (the most common irritant), agents containing thioglycolates for permanently waving hair and blow drying the hair.
Clinically, the scalp may be erythematous, vesicular and weeping (Figure 6). The timing of onset can help differentiate irritant and allergic contact dermatitis; irritant contact dermatitis appears after the first exposure, whereas allergic contact dermatitis requires sensitisation and develops after repeated exposure.
Patch testing is generally useful for diagnosing the substance responsible. In addition to avoidance of triggers, treatment with a topical corticosteroid is usually all that is needed. Oral prednisolone can be used for patients with severe contact dermatitis.
Endogenous or atopic eczema
Eczema involves the scalp usually in the setting of a generalised flare rather than as an isolated presentation. The scalp may be diffusely red, vesicular and weeping. The hair may become matted and temporary alopecia may occur.
Eliminating triggers, keeping skin moisturised and using wet dressings and bleach baths as needed are the mainstays of preventative management. Treatment with topical corticosteroids can be considered. An alcohol-based lotion is useful in the presence of thickened, matted hairs but can be strongly irritating. A potent corticosteroid cream (betamethasone dipropionate, methylprednisolone aceponate or mometasone furoate) diluted with water is a more acceptable alternative. In an eczematous flare, there is usually increased colonisation or infection with Staphylococcus aureus, and successful treatment often requires concurrent oral antibiotics. Biologic and advanced targeted systemic treatments are now available, including dupilumab and upadacitinib, and must be prescribed by a dermatologist. Dupilumab is a monoclonal antibody that inhibits interleukin 4 and is administered subcutaneously. Upadacitinib is a janus kinase 1 (JAK1) inhibitor administered once daily as an oral tablet. Both agents are PBS subsidised for chronic severe atopic dermatitis that is inadequately controlled with topical pharmacotherapies.15-17
Lichen planopilaris
Lichen planopilaris is a rare inflammatory scalp condition that results in scarring alopecia. Early lesions consist of perifollicular erythema, scale and violaceous papules. Later, there is follicular plugging that is replaced by scarring. There is an absence of follicular openings within foci of hair loss (Figure 7). The scalp is often itchy and tender but can be asymptomatic. Activity may be localised to the scalp or present elsewhere on the body, where it serves as a diagnostic clue.
Early treatment is necessary to avoid scarring and permanent hair loss, and patients should be referred to a dermatologist. Potent topical corticosteroids are the first-line treatment, generally in combination with intralesional corticosteroids. Rapidly progressive and extensive disease requires systemic therapy.
Folliculitis
Pruritus of the scalp associated with monomorphic papules and pustules raises the possibility of folliculitis, a disorder with infectious (most commonly) and non-infectious aetiologies. Frequent causes of infectious folliculitis include S. aureus, Malassezia spp. (Figure 8) and the mite Demodex folliculorum.
When culture reveals S. aureus infection, treatment with topical clindamycin lotion or oral flucloxacillin is recommended. Topical therapy with antifungal shampoo is usually effective for Malassezia folliculitis, although occasionally a course of oral antifungal therapy may be needed. Demodex folliculitis may be treated with topical permethrin cream or oral ivermectin.
Acne necrotica
Acne necrotica presents with recurring crops of pruritic, red-brown papules that undergo central necrosis and resolve with varioliform scars. Lesions are distributed around the anterior hairline and areas of increased sebum production on the face and trunk.18 Cicatricial alopecia may result. Patients respond to antistaphylococcal antibiotics, including tetracyclines and macrolides. Positive responses to isotretinoin have been reported.19
Trigeminal trophic syndrome
Trigeminal trophic syndrome is a complication of trigeminal nerve injury. Anaesthesia and dysaesthesia in the sensory distribution of the trigeminal nerve trigger an irresistible desire to pick the skin, with resultant ulceration. Crescentic ulceration of the nasal rim with sparing of the nasal tip is characteristic, but other sites, including the scalp and forehead may be affected (Figure 9). Treatment centres around the use of protective barriers and pharmacological therapies for neuropathic pain. Long-term treatment success has been reported with skin flaps and grafts.
Dermatitis herpetiformis
Dermatitis herpetiformis is a rare autoimmune skin disease associated with gluten-sensitive enteropathy. It is characterised by intensely pruritic papulovesicles that occur in herpetiform clusters, most often over the extensor surfaces of the elbows, dorsal forearms, knees, buttocks and scalp. Vesicles are disturbed by vigorous scratching, and secondary erosions and excoriations predominate.
The diagnosis of dermatitis herpetiformis is confirmed by detection of subepidermal blisters and granular IgA deposits in the papillary dermis through direct immunofluorescence of a skin biopsy specimen. Serology may aid in the diagnosis.
Dermatitis herpetiformis is usually treated with dapsone, topical corticosteroids and a gluten-free diet. Patients should be referred to a dermatologist and a gastroenterologist.
Scabies
Scabies involves the scalp usually only in infants, young children and older or immunosuppressed patients. Other sites that are involved are the palms of the hands, soles of the feet, neck and flexural areas. The rash is typified by pruritic erythematous papules that become excoriated. Vesicles, indurated nodules, eczematous dermatitis and secondary bacterial infection are also common. The pathognomonic scabetic ‘burrow’ is a greyish white, thread-like structure, 1 to 10 mm long, found on the extremities. The mite has a characteristic ‘jet with contrail’ or ‘hang glider’ appearance on dermoscopy.
Treatment consists of two applications, one week apart, of topical permethrin 5% cream. It is essential to treat household contacts at the same time as the patient to prevent cross infection. Bedclothes and linen should be hot washed and tumble dried to prevent fomite transmission. Oral ivermectin is PBS subsidised for treatment-resistant scabies. Two doses of 200 mcg/kg should be administered with fatty food, with the first on day one and the second sometime between day eight and 15.20
Psychosomatic disorders
Psychosocial stressors, anxiety or endogenous depression can manifest as various dermatological complaints, including scalp pruritus. Direct questioning may reveal such precipitants in the absence of clear organic disease.
Idiopathic pruritus capitis
Scalp pruritus may occur in the absence of identifiable disease. Unexplained scalp pruritus can occur during periods of stress and as a manifestation of ageing (pruritus of senescence). Neuropathic pruritus (e.g. burning scalp syndrome, notalgia paraesthetica and postherpetic neuralgia) should be considered in patients with localised itch on noninflamed skin, especially if they have accompanying dysaesthesia, such as numbness or a burning sensation.
Scalp pruritus often occurs in the context of generalised whole-body pruritus. The medication history may reveal a pharmacological cause. Common triggers include opioids, NSAIDs, antihypertensive drugs, especially thiazide diuretics, lipid-lowering drugs, such as statins, and antibiotics. In rare cases, generalised pruritus is associated with an underlying disease process, including malignancy. In patients with lymphoma, pruritus can be associated with systemic symptoms such as night sweats and weight loss.
Investigations for patients with chronic pruritus on noninflamed skin who do not respond to therapy depend on the clinical findings. Basic investigations can include a full blood count, measurement of electrolytes, thyroid function tests, iron studies and chest radiography.
In patients with unexplained scalp pruritus, empirical treatment may be helpful. Tar-based shampoos are useful as they have antipruritic properties. If itch persists then systemic therapies may be used, including antihistamines and antidepressants such as doxepin and selective serotonin reuptake inhibitors.
Is there a role for punch biopsy in the work-up for scalp pruritus?
Biopsies can be very helpful in reaching a diagnosis; however, scalp biopsies are ideally performed in a controlled setting (e.g. by a dermatologist) because of the associated risk of bleeding and the need for dermatopathologist expertise in interpreting the results. Biopsies can be useful in differentiating conditions such as psoriasis from eczema, and for diagnosing lichen simplex chronicus, lichen planopilaris and, occasionally, folliculitis. A scalp biopsy is useful for diagnosing dermatitis herpetiformis; however, ideally the biopsy would be taken from a more typical body site other than the scalp.
When should patients be referred?
Referral to a dermatologist is recommended in cases of persistent diagnostic uncertainty and disease that does not respond to treatment. Early dermatology referral is essential for patients with dermatitis herpetiformis, lichen planopilaris and other types of scarring alopecia.
Conclusion
Scalp pruritus is a common symptom that can be associated with a range of dermatological conditions. It is important to identify distinguishing features in the patient’s history and examination results to make an accurate diagnosis. Sometimes, a therapeutic trial is needed before the diagnosis is known. MT

