Personalising prostate cancer care. Part 2. Current treatment options
Treatment for men with prostate cancer can now be tailored according to patient, tumour, imaging and genetic factors. Current options include active surveillance, whole-gland surgery (including open, laparoscopic and robot-assisted techniques), radiotherapy (with improved targeting allowing higher doses), emerging focal therapies, chemotherapy and hormone therapy.
- Personalised tailored therapy for men with prostate cancer is now available.
- For men with low-risk prostate cancer, active surveillance is safe and minimises the quality-of-life burden that can accompany whole-gland therapy.
- Surgery or radiotherapy can be used for definitive treatment of localised prostate cancer.
- Focal therapy is emerging as a middle-ground option for selected patient groups.
- Men with high-risk or locally advanced prostate cancer usually require combination therapy.
- For men with advanced metastatic prostate cancer, hormone therapy remains the ‘gold standard’ treatment.
Picture credit: © Alex and David Baker
We are on the cusp of delivering truly personalised and tailored management for patients with prostate cancer. This is the second article in a two-part series describing recent advances in prostate cancer care. The first article in the series described advances in diagnosis (in the February issue of Medicine Today).1 This article discusses current treatments for men with prostate cancer, including personalised management options for localised, locally advanced and metastatic prostate cancer. Approaches include active surveillance, surgery, radiotherapy, emerging focal treatments and systemic therapies. Factors that influence the decision whether to treat prostate cancer or to offer active surveillance and which treatment to choose and its timing are outlined.
Active surveillance
Many patients with low-risk Gleason 6 prostate cancer (International Society of Urological Pathology [ISUP] grade group 1) do not require treatment and can instead be safely monitored. This approach avoids unnecessary side effects and the potential impact of whole-gland therapy on quality of life. Criteria for offering active surveillance rather than definitive treatment to men with prostate cancer are listed in the Box.2
The ideal patient for active surveillance has:
- a low-volume localised Gleason 6 prostate cancer (ISUP grade group 1)
- limited biopsy core involvement
- no other confounding factor, including no abnormal multiparametric MRI (mpMRI) results, strong family history or genetic abnormality (e.g. BRCA gene mutation).
Some patients with prostate cancer with a Gleason score of 3+4=7 (ISUP Grade Group 2) and a low Gleason pattern 4 component (<10%) are also suitable for active surveillance.2 This applies particularly to patients older than 70 years with a life expectancy of less than 10 years where mpMRI does not show a lesion. If mpMRI does show a significant abnormality (Prostate Imaging Reporting and Data System [PI-RADS] score of 4 or 5) then there may have been biopsy undersampling.
An initial thorough evaluation is always necessary before consideration of active surveillance. This may include saturation biopsy and mpMRI, on occasions supplemented by genetic testing of tumour tissue with tests such as the Oncotype DX Genomic Prostate Score or the Prolaris or Decipher tests.3
The selection of patients for active surveillance and the monitoring protocol are controversial and vary between centres.4-6 Active surveillance may involve the following, depending on the level of concern that the clinician has about the particular tumour:2
- up to three-monthly prostate-specific antigen (PSA) testing
- six to 12-monthly physical examination (digital rectal examination)
- mpMRI every one to two years performed in an experienced unit
- a prostate biopsy every one to four years.
A sudden change in mpMRI results may prompt an earlier biopsy. However, changes in PSA level are very common and should not in themselves immediately prompt a biopsy.
Active surveillance may allow up to 50% of patients to avoid unnecessary treatment.7 Studies have found that 10 to 30% of patients (10% of modern well-assessed patients) on active surveillance programs required treatment over a 15-year period, because of either disease progression or patient preference.8 This delay did not result in worse long-term outcomes.7,8
Choice of treatment for prostate cancer
In patients who are not suitable for active surveillance or prefer definitive treatment, traditional management options for localised prostate cancer include whole-gland treatment with surgery (radical prostatectomy) or radiotherapy.
The choice between surgery and radiotherapy is multifactorial and best decided in a multidisciplinary meeting. Each patient situation must be addressed on its own merit, considering specific patient, disease and treatment factors. Surgery is generally reserved for men who are younger and those whose cancer is contained within the prostate or has minimal extracapsular extension. Radiotherapy is generally preferred in older men. Reasons for the preference for surgery in younger men include the small but significant risk of secondary malignancy with radiotherapy, and also the limitations of subsequent salvage therapy after radiotherapy compared with surgery. It should be noted that the final choice between these two modalities often comes down to a comparison of side effect profiles, where patient preference is also important.
Focal therapy is emerging as a middle-ground option between active surveillance and whole-gland treatment for specific patient groups. It involves ablation of the tumour and preservation of the remainder of the prostate. A range of techniques for tumour ablation are being investigated.
For men with high-risk or locally advanced prostate cancer, combination therapy is usually required, and for those with advanced metastatic prostate cancer, hormone therapy remains the ‘gold standard’. Early metastatic prostate cancer is now regarded as a discrete entity that is being treated more aggressively in trials.
Surgery for prostate cancer
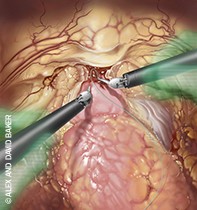
Radical prostatectomy is the complete removal of the prostate and seminal vesicles with anastomosis of the bladder to the urethra. It often also involves the removal of the regional pelvic lymph glands in patients with a high risk of lymph node invasion. As the prostate produces most of the fluid in semen, prostatectomy results directly in ‘dry orgasm’. Collateral damage to adjacent structures can involve the external urethral sphincter leading to incontinence, the erectile nerves leading to impotence and, rarely, the rectum.
Choice of surgical technique
Radical prostatectomy can be performed by the traditional open technique or by laparoscopic or robot-assisted laparoscopic techniques. Robot-assisted laparoscopic prostatectomy has gained popularity recently.9,10 The advantages of laparoscopic and robot-assisted laparoscopic prostate surgery include potentially quicker recovery, quicker return to normal activities, less blood loss and less need for transfusion.11,12 Recent data also suggest a decreased rate of postoperative complications such as inguinal hernia and bladder neck contracture.13,14
Nevertheless, careful review of data from highly experienced units suggests that there is little difference in oncological, sexual and urinary outcomes between these three techniques when they are performed by highly experienced surgeons.15-18 The experience of the surgeon is therefore the major factor to be considered, and the technique is secondary.9
Nerve-sparing techniques
Nerve-sparing techniques imply the preservation of the neurovascular bundles during surgery. There are several degrees of nerve sparing, with the ultimate aim of clear margins and preservation of as much nerve tissue as possible, to ensure the greatest chance of erectile function recovery postoperatively. There is a long learning curve for performing good nerve-sparing procedures as the sensitive autonomic nerves respond poorly to stretching, heat or bruising. Highly experienced units using nerve-sparing techniques can achieve satisfactory erection recovery in 50 to 90% of patients, depending on age and preoperative erection status.16
Lymph node removal
The removal of the regional lymph glands, including the obturator, internal iliac, external iliac and common iliac lymph nodes, in association with radical prostatectomy is recommended when the risk of lymph node metastases is greater than 3 to 5%, based on validated nomograms.19 There is evidence that lymph node dissection not only helps accurate staging and decision making for adjuvant therapy, but also may have a therapeutic impact.20 Recent innovations in positron emission tomography (PET) scanning with 68gallium-labelled prostate-specific membrane antigen (68Ga-PSMA) PET/CT techniques have improved detection of nodal metastases.21 Unfortunately, although this imaging technique is specific and more sensitive than traditional staging imaging (CT and bone scan), it is still limited in detecting metastatic deposits smaller than about 4 mm.22 At this stage, 68Ga-PSMA PET/CT is not recommended for selecting patients for node dissection.
Surgical quality assessment
The learning curve for open, laparoscopic and robot-assisted laparoscopic procedures can be anything from 100 to 1000 cases, depending on how it is assessed.23 Factors that impact on the learning curve include whether the doctor is fellowship trained and their natural aptitude. Furthermore, careful monitoring of one’s own results can shorten the learning curve. Surgeons need to be honest about their level of experience and outcomes in each one of these techniques when discussing treatment options with patients.
A quality of care registry has been developed in Victoria encompassing specific surgery outcome measures, and will soon be followed by a New South Wales registry.24 In the senior author’s opinion, important standards measures should include cases performed per year, positive margin rate (for pathological stage T2 and T3 disease), complication rates (Clavien-Dindo complication grade greater than 3), pad-free rates, potency rates and percentage of patients with purely Gleason 6 cancers at final histopathology.
Radiotherapy for prostate cancer
External beam radiotherapy (EBRT) to the prostate is a safe and established treatment for localised prostate cancer. The dose of radiation in recent years has been increased to more reliably eliminate disease. For intermediate to high-risk prostate cancer, generally a radiation dose of 74 Gy or more is required, which usually necessitates a seven-and-a-half week course of treatment.25 New techniques using intensity-modulated radiation therapy that provide better targeting and use of fiducial marker seeds and Spacing Organs at Risk (SpaceOAR) hydrogel between the rectum and the prostate have improved the accuracy and safety of radiotherapy, and allow higher, more effective doses to be delivered.26,27
Low-dose rate brachytherapy (iodine-125 permanent seed therapy) alone is also an established form of radiation therapy. This is generally used for low-risk and selected intermediate-risk prostate cancers. For higher-volume Gleason 3+4=7 (ISUP Grade Group 2) or Gleason 4+3=7 (ISUP Grade Group 3) tumours, a combination of short-term hormone therapy with brachytherapy is often required.25Low-dose rate brachytherapy is not appropriate for patients with a large prostate, severe urinary symptoms, a large middle lobe or previous large transurethral resection of the prostate.
Focal therapy
It is clear that there is still considerable overtreatment of men with prostate cancer and that whole-gland therapy (surgery or radiotherapy) can have significant side effects. Furthermore, active surveillance is not suitable for all patients. Focal therapy is a novel approach that is gaining popularity as a middle-ground treatment for low-volume significant prostate cancer in an older cohort. It minimises genitourinary side effects while still eliminating small localised tumours.28 Focal therapy generally involves the ablation of a low-volume significant prostate cancer or an index tumour, where the remaining prostate is clear of disease. Energy sources that are being used include high-intensity focus ultrasound (HIFU), cryotherapy, laser therapy, photodynamic therapy (PTD), irreversible electroporation (IRE), targeted radiotherapy and even focal surgery.29
The selection of patients for focal therapy is still controversial. A thorough evaluation of the whole prostate, including a template transperineal mapping biopsy as well as mpMRI (lesion should be visible) is required.28 If there is good co-registration between results of the two techniques, the tumour occupies less than a quarter of the prostate and the patient refuses or is unsuitable for radical prostatectomy or radiotherapy then focal therapy is a reasonable option, but only in a fully informed patient.29 Currently, we are investigating irreversible electroporation focal therapy at our centre for primary and salvage (recurrent cancer after radiotherapy) treatment, with the potential advantages including a sharply demarcated ablation zone and tissue selectivity (NanoKnife therapy).30 The long-term cancer outcomes are as yet unproven. Genetic testing may ultimately improve patient selection to ensure that there are no abnormal precancerous changes in the remaining untreated prostate. Further validation studies are needed before focal therapy can be adopted in guidelines on prostate cancer management.
High-risk and locally advanced prostate cancer
Patients with high-risk and locally advanced prostate cancers often require a combination of therapies.31 However, the greater the number of treatments, the greater the risk of side effects. Surgery in this setting is relatively non-nerve-sparing. In addition to surgery, adjuvant radiotherapy is often required, and adjuvant systemic therapy may also be necessary in the form of hormone or chemotherapy.25
For high-risk and locally advanced prostate cancers, the standard dose of radiotherapy is often insufficient. To successfully treat these patients with radiotherapy, a combination of EBRT and either low-dose rate or high-dose rate brachytherapy is required as a boost.25 Androgen deprivation therapy (ADT) is often also combined with radiotherapy in these patients.32 There is level 1 evidence that combining ADT with radiotherapy in this setting improves biochemical disease-free survival and overall survival rates.31,33 The duration of hormone therapy is dictated by the individual clinical situation and can be from six to 36 months.25
The side effects of ADT combined with radiotherapy can be quite substantial and additive. ADT side effects include tiredness, decreased libido, hot flushes and metabolic syndrome, which may be minimised by exercise, diet modification and treatment with metformin.34 The combination of EBRT and brachytherapy also has a significant impact on quality of life, largely causing sexual and irritative urinary symptoms, and a smaller incidence of bowel symptoms.33
The choice of treatment for locally advanced prostate cancer should be individualised and subject to a multidisciplinary meeting.
Early metastatic prostate cancer
Emerging technologies such as 68Ga-PSMA PET/CT scanning have improved detection of early metastatic disease.21 Oligometastatic disease (fewer than five secondaries in bone or lymph glands) is now defined as a new entity, and is being treated more aggressively in trial settings.35 Whole-pelvic radiotherapy with targeting of positive nodes is being trialled for early metastatic disease to lymph glands. Similarly, stereotactic radiosurgery is under investigation for oligometastatic bone disease, and salvage lymph node surgery for oligometastatic pelvic/retroperitoneal lymph node disease.35,36 Proof of the benefit is still lacking, and although these therapies have been shown to be relatively safe, further prospective clinical data are required.37 Patients who are keen to delay hormone therapy may seek out these experimental therapies.
Advanced metastatic prostate cancer
Hormone therapy remains the gold standard for treatment of men with advanced metastatic prostate cancer, but the timing of its introduction is still debated.33 Intermittent ADT appears to be a reasonable oncological option in most cases, with improved quality of life compared with continuous hormone therapy. The only exception is in the setting of a rapid PSA doubling time, where it is suggested that continuous hormone therapy is used.38,39 Complete hormone ablation combining luteinising hormone releasing hormone (LHRH) agonists with antiandrogens such as bicalutamide has a marginal benefit compared with LHRH agonists alone.33
Further antiandrogen therapy has been developed for castrate-resistant metastatic prostate cancer, with use of the newer agents abiraterone or enzalutamide. These have been proven to be effective after standard hormone therapy has failed, both before and after chemotherapy.40 The only marker that has been found to help guide this decision is androgen receptor splice variant testing. A positive result suggests that chemotherapy should be used rather than antiandrogen therapy. Effective chemotherapeutic agents (such as docetaxel) in combination with hormone therapy have been proven to prolong life in several trials, including the STAMPEDE and CHAARTED trials.41
Bone health is increasingly important in patients with advanced prostate cancer. Regular bone mineral density monitoring is required. Regular exercise, a healthy diet and calcium and vitamin D supplementation are mandatory. In addition, bisphosphonate and denosumab therapy may help patients who develop treatment-related osteoporosis to avoid bone events such as fractures.33
Psychological support for patients with advanced disease is crucial. Appropriate counselling by support groups, GPs and specialists is important not only for patients but also for their families. Various forms of pain management and coping mechanisms using techniques such as mindfulness have also been useful in this setting.
Side effects of treatment
Loss of urinary control (incontinence)
Preoperative pelvic floor exercises have been shown to minimise the incidence of incontinence after surgery.42 For patients who have mild stress incontinence after surgery (requiring less than two pads per day), various forms of sling procedures (including the AdVance male sling system) have become popular. Sling procedures tend to be successful initially in about 80% of patients, and in the long term in about 50 to 60% of patients.43 Bulking agents and adjustable continence therapy (such as ProACT devices) that use small balloons around the bladder neck seem to have inferior results.44 For patients with urge incontinence, anticholinergics, beta agonists (e.g. mirabegron) or intravesical injection of botulinum toxin may help.
The artificial sphincter procedure remains the ‘gold standard’ to treat patients with severe incontinence and is useful for either postsurgical or postradiation incontinence.42 The device is relatively durable but has a revision rate of 10 to 20% over the lifetime.42,45
Erectile dysfunction
Postsurgical erectile dysfunction can be minimised by careful surgical technique and sexual rehabilitation. Rehabilitation generally starts as soon as possible after surgery, and patients are encouraged to stimulate sexual activity and stimulate erection. Treatments for men with erectile dysfunction after radiotherapy or surgery include phosphodiesterase type 5 inhibitors, vacuum constriction devices, self-injection therapy or ultimately a penile prosthesis.46 The choice of treatment depends on the degree of impotence, timing after therapy and patient preference.
Rectal and bladder damage from radiotherapy
Radiotherapy may cause rectal and bladder toxicity, resulting in rectal bleeding and haematuria.47 This can be minimised by using marker fiducial seeds, SpaceOAR hydrogel between the rectum and the prostate, good technique with meticulous planning and modern intensity-modulated radiation equipment. If rectal toxicity occurs then prednisone enemas, hyperbaric oxygen therapy and laser therapy to the area can be useful. Radiation damage to the bladder may be treated with local bladder laser therapy, chemical instillations, hyperbaric oxygen therapy or occasionally urinary diversion.
Conclusion
The era of personalised tailored therapy for men with prostate cancer is now upon us. Management of prostate cancer is multifactorial and should take into consideration patient, tumour, imaging and genetic factors, ultimately leading to selection of the appropriate treatment at the appropriate time for the individual patient.
COMPETING INTERESTS: None.
References
- Siriwardana A, Thompson J, Stricker P. Personalising prostate cancer care. Part 1. Advances in diagnosis. Med Today 2017; 18(2): 29-32.
- Prostate Cancer Foundation of Australia and Cancer Council Australia PSA Testing Guidelines Expert Advisory Panel. Clinical practice guidelines for PSA testing and early management of test-detected prostate cancer. Sydney: Cancer Council Australia; 2016. Available online at: http://wiki.cancer.org.au/australia/Guidelines:PSA_Testing (accessed February 2017).
- Bostrom PJ, Bjartell AS, Catto JW, et al. Genomic predictors of outcome in prostate cancer. Eur Urol 2015; 68: 1033-1044.
- Simpkin AJ, Tilling K, Martin RM, et al. Systematic review and meta-analysis of factors determining change to radical treatment in active surveillance for localized prostate cancer. Eur Urol 2015; 67: 993-1005.
- Lane JA, Hamdy FC, Martin RM, Turner EL, Neal DE, Donovan JL. Latest results from the UK trials evaluating prostate cancer screening and treatment: the CAP and ProtecT studies. Eur J Cancer 2010; 46: 3095-3101.
- Stöckle M, Bussar-Maatz R. [Localised prostate cancer: the PREFERE trial]. Z Evid Fortbild Qual Gesundhwes 2012; 106: 333-335; discussion 335.
- Klotz L, Vesprini D, Sethukavalan P, et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol 2015; 33: 272-277.
- Dall’Era MA, Albertsen PC, Bangma C, et al. Active surveillance for prostate cancer: a systematic review of the literature. Eur Urol 2012; 62: 976-983.
- Trinh QD, Bjartell A, Freedland SJ, et al. A systematic review of the volume-outcome relationship for radical prostatectomy. Eur Urol 2013; 64: 786-798.
- Sooriakumaran P, Srivastava A, Shariat SF, et al. A multinational, multi-institutional study comparing positive surgical margin rates among 22393 open, laparoscopic, and robot-assisted radical prostatectomy patients. Eur Urol 2014; 66: 450-456.
- Hu JC, Gandaglia G, Karakiewicz PI, et al. Comparative effectiveness of robot-assisted versus open radical prostatectomy cancer control. Eur Urol 2014; 66: 666-672.
- Gandaglia G, Sammon JD, Chang SL, et al. Comparative effectiveness of robot-assisted and open radical prostatectomy in the postdissemination era. J Clin Oncol 2014; 32: 1419-1426.
- Ramsay C, Pickard R, Robertson C, Close A, Vale L. Systematic review and economic modelling of the relative clinical benefit and cost-effectiveness of laparoscopic surgery and robotic surgery for removal of the prostate in men with localised prostate cancer. Health Technol Assess 2012; 16(41): 1-313.
- Close A, Robertson C, Rushton S, et al. Comparative cost-effectiveness of robot-assisted and standard laparoscopic prostatectomy as alternatives to open radical prostatectomy for treatment of men with localised prostate cancer: a health technology assessment from the perspective of the UK National Health Service. Eur Urol 2013; 64: 361-369.
- Yaxley JW, Coughlin GD, Chambers SK, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet 2016; 388: 1057-1066.
- Ficarra V, Novara G, Ahlering TE, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol 2012; 62: 418-430.
- Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012; 62: 405-417.
- Haglind E, Carlsson S, Stranne J, et al. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol 2015; 68: 216-225.
- Briganti A, Larcher A, Abdollah F, et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 2012; 61: 480-487.
- Briganti A, Blute ML, Eastham JH, et al. Pelvic lymph node dissection in prostate cancer. Eur Urol 2009; 55: 1251-1265.
- Perera M, Papa N, Christidis D, et al. Sensitivity, specificity, and predictors of positive 68ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol 2016; 70: 926-937.
- van Leeuwen PJ, Emmett L, Ho B, et al. Prospective evaluation of 68Gallium-prostate-specific membrane antigen positron emission tomography/computed tomography for preoperative lymph node staging in prostate cancer. BJU Int 2017; 119: 209-215.
- Thompson JE, Egger S, Bohm M, et al. Superior quality of life and improved surgical margins are achievable with robotic radical prostatectomy after a long learning curve: a prospective single-surgeon study of 1552 consecutive cases. Eur Urol 2014; 65: 521-531.
- Sampurno F, Earnest A, Kumari PB, et al. Quality of care achievements of the Prostate Cancer Outcomes Registry-Victoria. Med J Aust 2016; 204: 319.
- Mottet N, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 2016; pii: S0302-2838(16)30470-5. [Epub ahead of print.]
- Zelefsky MJ, Levin EJ, Hunt M, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2008; 70: 1124-1129.
- Zumsteg ZS, Spratt DE, Romesser PB, et al. The natural history and predictors of outcome following biochemical relapse in the dose escalation era for prostate cancer patients undergoing definitive external beam radiotherapy. Eur Urol 2015; 67: 1009-1016.
- Donaldson IA, Alonzi R, Barratt D, et al. Focal therapy: patients, interventions, and outcomes – a report from a consensus meeting. Eur Urol 2015; 67: 771-777.
- Valerio MC, Eggenerd Y, Lepore S, Polascikf H, Villers T, A. Emberton, M. New and established technology in focal ablation of the prostate: a systematic review. Eur Urol 2017; 71: 17-34.
- Ting F, Tran M, Bohm M, et al. Focal irreversible electroporation for prostate cancer: functional outcomes and short-term oncological control. Prostate Cancer Prostatic Dis 2016; 19: 46-52.
- Jones CU, Hunt D, McGowan DG, et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N Engl J Med 2011; 365: 107-118.
- Zelefsky MJ, Pei X, Chou JF, et al. Dose escalation for prostate cancer radiotherapy: predictors of long-term biochemical tumor control and distant metastases-free survival outcomes. Eur Urol 2011; 60: 1133-1139.
- Heidenreich A, Bastian PJ, Bellmunt J, et al. EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 2014; 65: 467-479.
- Ahmadi H, Daneshmand S. Androgen deprivation therapy: evidence-based management of side effects. BJU Int 2013; 111: 543-548.
- Ost P, Bossi A, Decaestecker K, et al. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol 2015; 67: 852-863.
- Tosoian JJ, Gorin MA, Ross AE, Pienta KJ, Tran PT, Schaeffer EM. Oligometastatic prostate cancer: definitions, clinical outcomes, and treatment considerations. Nat Rev Urol 2017; 14: 15-25.
- Decaestecker K, De Meerleer G, Ameye F, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence (STOMP): study protocol for a randomized phase II trial. BMC cancer 2014; 14: 671.
- Magnan S, Zarychanski R, Pilote L, et al. Intermittent vs continuous androgen deprivation therapy for prostate cancer: a systematic review and meta-analysis. JAMA Oncol 2015; 1: 1261-1269.
- Sciarra A, Abrahamsson PA, Brausi M, et al. Intermittent androgen-deprivation therapy in prostate cancer: a critical review focused on phase 3 trials. Eur Urol 2013; 64: 722-730.
- Loblaw DA, Walker-Dilks C, Winquist E, Hotte SJ; Genitourinary Cancer Disease Site Group of Cancer Care Ontario’s Program in Evidence-Based Care. Systemic therapy in men with metastatic castration-resistant prostate cancer: a systematic review. Clin Oncol (R Coll Radiol) 2013; 25: 406-430.
- Tucci M, Bertaglia V, Vignani F, et al. Addition of docetaxel to androgen deprivation therapy for patients with hormone-sensitive metastatic prostate cancer: a systematic review and meta-analysis. Eur Urol 2016; 69: 563-573.
- Bauer RM, Bastian PJ, Gozzi C, Stief CG. Postprostatectomy incontinence: all about diagnosis and management. Eur Urol 2009; 55: 322-333.
- Rehder P, Haab F, Cornu JN, Gozzi C, Bauer RM. Treatment of postprostatectomy male urinary incontinence with the transobturator retroluminal repositioning sling suspension: 3-year follow-up. Eur Urol 2012; 62: 140-145.
- Hubner WA, Schlarp OM. Adjustable continence therapy (ProACT): evolution of the surgical technique and comparison of the original 50 patients with the most recent 50 patients at a single centre. Eur Urol 2007; 52: 680-686.
- O’Connor RC, Lyon MB, Guralnick ML, Bales GT. Long-term follow-up of single versus double cuff artificial urinary sphincter insertion for the treatment of severe postprostatectomy stress urinary incontinence. Urology 2008; 71: 90-93.
- Salonia A, Burnett AL, Graefen M, et al. Prevention and management of postprostatectomy sexual dysfunctions part 2: recovery and preservation of erectile function, sexual desire, and orgasmic function. Eur Urol 2012; 62: 273-286.
- Budaus L, Bolla M, Bossi A, et al. Functional outcomes and complications following radiation therapy for prostate cancer: a critical analysis of the literature. Eur Urol 2012; 61: 112-127.