Chronic rhinosinusitis: meeting the challenges
Chronic rhinosinusitis is a common condition that typically has a complex multifactorial pathophysiology. It is important to consider other conditions that can masquerade as sinusitis when making the diagnosis. Initial diagnosis and treatment begins in general practice but may require specialist assistance. Symptoms such as clear fluid rhinorrhoea, neurological symptoms and sudden loss of the sense of smell dictate more urgent referral.
- Chronic rhinosinusitis is defined by two or more of nasal obstruction, mucopurulent discharge, decreased sense of smell or facial pain, along with CT or endoscopic evidence of sinus disease.
- Consider differential diagnoses according to symptoms; they include allergic rhinitis, headache syndromes such as migraine, laryngopharyngeal reflux and globus pharyngeus.
- Nasal obstruction, a postnasal drip, headaches or loss of smell as sole individual symptoms are rarely due to sinusitis.
- Once the diagnosis is made, commence a trial of maximal medical management.
- If the patient does not respond to maximal medical management then referral to an ear, nose and throat specialist is warranted for further investigation and medical and possibly surgical management.
- Removal of the adenoids is often helpful in children with chronic rhinosinusitis.
Picture credit: © Audra Geras
Chronic rhinosinusitis is a common condition that typically has a complex multifactorial pathophysiology. It is important to consider other conditions that can masquerade as sinusitis when making the diagnosis. Initial diagnosis and treatment begins in general practice but may require specialist assistance. Symptoms such as clear fluid rhinorrhoea, neurological symptoms and sudden loss of the sense of smell dictate more urgent referral.
Chronic rhinosinusitis (also known as chronic sinusitis) is a common condition that is often challenging to treat successfully. Many patients require long-term treatment to reduce sinus inflammation and the impact of symptoms on their quality of life. The diagnosis can sometimes be confusing, particularly when patients presents with symptoms such as ‘sinus pain’, headaches, loss of the sense of smell, chronic cough and postnasal drip – all of which can be caused by conditions other than sinusitis.
With the availability of information online, many patients diagnose themselves and may request specific treatments or specialist referral. Many struggle with the adherence necessary to use medical therapy for the length of time needed for effectiveness. Unfortunately, a small group of patients need indefinite medical therapy and may still have symptom exacerbations that require additional treatments (e.g. culture-directed oral antibiotics, prednisone, topical corticosteroid creams) from time to time.
Pathophysiology
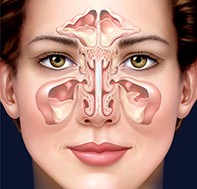
Our understanding of the pathophysiology of chronic rhinosinusitis evolves every year as new research is presented and published.1 The aetiology in individual patients is usually multifactorial, with host and environmental factors both playing a part. Host factors that may contribute to chronic rhinosinusitis include genetics, allergy, osteitis, laryngopharyngeal reflux, immunodeficiency and mucociliary and epithelial dysfunction. Environmental factors include microbiome disturbance by bacteria, viruses and fungi, the formation of biofilms, smoking and pollution. Anatomy of the sinuses is shown in Figure 1.
Diagnosis
Chronic rhinosinusitis is defined in the literature as:1
- the presence for 12 weeks or longer of two or more of the following:
- mucopurulent discharge (rhinorrhoea or postnasal drip)
- nasal obstruction
- decreased sense of smell
- facial pain
- as well as at least one of:
- CT scan evidence of sinusitis
- endoscopic evidence of visible pus coming from the sinuses.
In clinical practice, the symptoms of chronic rhinosinusitis are more diverse and can be classified into four groups:
- nasal (obstruction, discharge, impaired sense of smell)
- facial (pressure, pain, headaches)
- oropharyngeal (ear pain, halitosis, postnasal drip, dental pain, cough)
- systemic (general malaise, fatigue).
The most common symptom of chronic rhinosinusitis is nasal obstruction, followed by postnasal drip. Most patients who present with only facial pain or headaches (particularly unilateral headaches) without other symptoms of sinusitis generally do not have sinusitis.
Chronic rhinosinusitis can be differentiated into two broad types – chronic rhinosinusitis with polyps and without polyps. The presence of polyps influences symptoms and management (Figure 2).
Differential diagnoses
Differential diagnoses for specific symptoms
It is important to establish what symptoms are the patient’s primary concern. Not only does this help guide treatment but it also helps avoid overlooking alternative diagnoses. Differential diagnoses for the different symptoms of chronic rhinosinusitis are summarised in the Box.
Nasal obstruction
Most patients with chronic rhinosinusitis have some degree of nasal obstruction. This is frequently one of their chief complaints. The presence of nasal obstruction in the absence of other symptoms of sinusitis should raise suspicion for other causes. These include a deviated nasal septum, large adenoids, allergic rhinitis or nasal valve collapse. Nasal valve collapse is a frequently overlooked condition that causes nasal obstruction due to collapse of the soft tissues of the nose with inspiration.
Postnasal drip
The sensation of postnasal drip, frequently felt as throat irritation, is common and is not always due to chronic rhinosinusitis. Other possible causes include gastro-oesophageal reflux, laryngopharyngeal reflux or chronic laryngeal irritation from a throat-clearing habit. Increased production of mucus that is felt in the throat can also be caused by allergic rhinitis and nonallergic rhinitis (such as vasomotor rhinitis).
Headaches and facial pain
Headaches with pain in the midface, around the orbits or in the frontal area are also common. Patients usually present these symptoms as ‘sinus pain’ or ‘sinus’. Be wary of attributing chronic facial pain to sinus pathology, especially if the pain is episodic. It is uncommon for sinusitis to present with pain in the absence of other symptoms. A CT scan during an episode of pain can be helpful in ruling out sinus pathology. Periorbital and frontal headaches that are episodic and unilateral are usually caused by migraine.
Loss of sense of smell (anosmia)
Chronic rhinosinusitis, particularly with nasal polyps, is a cause of a decline in the sense of smell. Essentially, polyps block the transmission of smells to the olfactory receptors. However, many other causes of anosmia should be considered. If anosmia is the patient’s only symptom then referral to an ear, nose and throat (ENT) specialist is probably worthwhile to assess for the large number of other potential causes of this symptom. These include old age, certain medications (e.g. amiodarone, oxymetazoline), Alzheimer’s disease and other types of dementia such as Lewy body dementia, Parkinson’s disease and nutritional disturbances (e.g. vitamin A or thiamine deficiency and excess zinc) and hormonal disturbances (e.g. hypothyroidism, hypoadrenalism and diabetes mellitus). In many cases the cause is idiopathic. Progressive or sudden loss of the sense of smell warrants a CT scan of the brain and sinuses to rule out primary olfactory tract pathology.
Chronic cough
A chronic cough has many possible causes. Sinusitis presents more commonly in children with a persistent cough. Clinicians should look for other more specific upper airway symptoms in the history and for evidence of sinus disease on examination or CT before concluding that sinusitis is the cause of chronic cough.
Chronic throat irritation, throat clearing, coughing and a sensation of postnasal drip in the absence of any diagnostic clinical findings is also a common presentation. It falls under the diagnosis of globus pharyngeus (persistent sensation of a lump or irritation in the throat). This condition has a strong psychological component and often requires a multidisciplinary approach to treatment.
Differential diagnoses for nasal polyps
Several space-occupying lesions in the nasal cavity can appear clinically and radiologically similar to nasal polyps and must be considered in the diagnosis of polyps. They include:
- normal structural variants, such as a concha bullosa (air filled cavity within a turbinate), medialised uncinate process or a very large inferior turbinate
- benign nasal tumours, including inverted papillomas, haemangiomas and schwannomas
- malignant tumours, including squamous cell carcinomas, salivary gland tumours, olfactory neuroblastomas and lymphomas
- other masses, including encephalocoeles, antrochoanal polyps and foreign bodies.
Tumours tend to be unilateral, may lack sinus inflammation and may display surface features such as easy bleeding and ulceration.
What investigations are needed?
A noncontrast low-dose CT scan rather than an MRI scan is the best initial investigation for the diagnosis of chronic rhinosinusitis (Figure 3). However, a scan is not needed for diagnosis if there is endoscopic evidence of sinusitis. A CT scan is also helpful to identify anatomical variants that may be contributing to chronic rhinosinusitis, such as accessory ostia or a concha bullosa. If chronic rhinosinusitis is diagnosed then it is often helpful to repeat the CT scan after three weeks to three months of maximal medical management (see below). This helps to evaluate for treatment response and residual disease. Patients who present primarily with episodic headaches should be encouraged to undergo the scan on a day when the headache is severe.
It may be appropriate to consider further investigation of the patient’s immune system and to evaluate for chronic diseases. This may include assessment for vitamin D deficiency, sarcoidosis (with measurement of serum ACE level), immunodeficiency (complement and immunoglobulin IgA, IgM and IgG subtype levels) and hypothyroidism (thyroid stimulating hormone level). Consider evaluating for asthma and for allergic rhinitis (with blood or skin-prick allergy testing).
What is the initial treatment?
After chronic rhinosinusitis is diagnosed, initial treatment should consist of a combination of therapies. Choice of treatment depends on the presence or absence of polyps. Consider continuing medical therapy for up to three months to assess for benefit as it can take time to reverse the inflammatory process in patients with established chronic rhinosinusitis. This initial treatment is referred to as ‘maximal medical management’.
Chronic rhinosinusitis without polyps
In patients with chronic rhinosinusitis without nasal polyps, initial treatment should consist of the following combination of treatments:
- a macrolide antibiotic for a minimum of three weeks (e.g. clarithromycin 250 mg orally twice a day)
- a topical corticosteroid nasal spray (e.g. two sprays in each nostril of mometasone 50 µg daily)
- high-volume saline irrigation.
If patients are allergic to macrolide antibiotics then consider culture-directed or no antibiotic therapy, as there is little evidence for the benefit of nonmacrolide oral antibiotics in chronic rhinosinusitis.
High-volume saline solutions (more than 200 mL) are superior to low-volume saline spray products. Of the many options for high-volume saline irrigation (both hypertonic and hypotonic), none have been shown to be superior. A strategy to promote adherence is to ask the patient to perform the irrigation when they clean their teeth, typically twice a day. They should rinse the irrigation bottle with detergent every few weeks to prevent bacterial colonisation.
Patients should be reviewed after three weeks, and treatment options reassessed. Maximal medical therapy may be continued for three months. If the response is not adequate after that time then specialist review should be sought.
Chronic rhinosinusitis with polyps
For patients with chronic rhinosinusitis with polyps, a two-week course of oral prednisone (50 mg tapering to 12.5 mg daily) should be combined with a corticosteroid nasal rinse. A budesonide 1 mg/mL ampoule in a high-volume saline rinse product used once daily is an excellent choice. An alternative is betamethasone cream dissolved in a saline rinse product. After specialist ENT review, the corticosteroid nasal rinse may be continued indefinitely to prevent polyp recurrence.
Specialist referral
When should patients be referred?
Failure of maximal medical management should trigger referral to an ENT specialist. Failure is defined as persistence of symptoms. Persistence of radiological or endoscopic disease without symptoms does not in itself define failure of treatment but may predict subsequent relapse.
What symptoms require more urgent referral?
Patients with symptoms or signs suggesting complications of chronic rhinosinusitis should be referred more urgently. Clinicians should be on the lookout for these symptoms and signs, which include:
- clear fluid rhinorrhoea (suggesting skull base erosion)
- meningism
- cranial nerve palsies (suggesting invasive fungal infection)
- orbital or ocular symptoms including diplopia, blurred vision (suggesting orbital wall erosion)
- sudden loss of sense of smell (suggesting infection or a tumour)
- severe progressive pain (suggesting a tumour).
What will an ear, nose and throat specialist do?
After a chronic inflammatory process has begun, treatment needs to roll back this inflammation, often by targeting it in multiple ways. The steps that an ENT specialist will follow are:
- to confirm the diagnosis and rule out differential diagnoses
- to ensure that maximal medical therapy has been provided for an adequate treatment period
- if maximal medical therapy has failed, to deliver further medical therapy, including
- allergy testing and treatment (avoidance, medication, immunotherapy)
- culture-directed antimicrobial therapy
- further topical and oral corticosteroid therapy
- aspirin desensitisation (if allergy is present)
- to consider surgery.
Surgery for chronic rhinosinusitis
Surgery for chronic rhinosinusitis is generally indicated when symptoms persist despite an appropriate trial of medical therapy. There have been dramatic advances in sinus surgery techniques over the past three decades. Modern sinus surgery emphasises mucosal preservation and enlargement of natural sinus drainage pathways (Figure 4). Endoscopic approaches are standard.
Surgery has several primary aims:
- to establish a patent nasal airway and relieve sinus outflow obstruction
- to remove biofilms and decrease the overall inflammatory load
- to open the sinuses to allow postoperative delivery of topical medication.
Paediatric chronic rhinosinusitis
Most children with rhinorrhoea, nasal congestion and a cough lasting more than 12 weeks have chronic rhinosinusitis.
Pathophysiology
Chronic rhinosinusitis in children is thought to be multifactorial, possibly involving bacteria, biofilms, adenoiditis and inflammatory cellular changes. In children, the adenoids are believed to act as a reservoir of bacteria. In some children adenoiditis is the primary problem. However, the actual size of the adenoids is not believed to be important in children with rhinosinusitis.
Contributing factors
Asthma is closely linked to paediatric chronic rhinosinusitis. Asthma that does not respond to medical therapy can be the only presenting symptom of paediatric chronic rhinosinusitis. Asthma symptoms can return when sinusitis episodes recur. Helping to control chronic rhinosinusitis in children with asthma will help to control their asthma.
The association between allergic rhinitis and paediatric chronic rhinosinusitis is controversial. Allergic rhinitis may be a contributing factor to chronic rhinosinusitis in some patients, but generally the cause is multifactorial.
Immunodeficiency has also been reported as a contributing factor in several studies.2-4 Abnormalities commonly seen in patients with chronic rhinosinusitis include IgG subclass deficiencies, IgA deficiency and poor response to pneumococcal vaccination. Intravenous immunoglobulin can help to reduce episodes of chronic rhinosinusitis in children with immunoglobulin deficiency.
Children with cystic fibrosis have a high incidence of paediatric chronic rhinosinusitis and nasal polyposis. All children with nasal polyps should be tested for cystic fibrosis.
Primary ciliary dyskinesia is a rare cause of paediatric chronic rhinosinusitis. This is an autosomal recessive disorder involving dysfunction of cilia. The diagnosis is considered in children with chronic rhinosinusitis who do not respond to medical and surgical treatment.
Controversy exists regarding the role of gastro-oesophageal reflux disease in paediatric chronic rhinosinusitis. At this stage, empirical treatment of gastro-oesophageal reflux disease is not indicated.
Diagnosis
Paediatric chronic rhinosinusitis is defined as the presence for 12 or more weeks of two or more of the symptoms of nasal congestion, coloured nasal discharge, facial pressure or pain or cough. In addition, purulent discharge and mucosal oedema should be evident on examination. Nasal endoscopy is useful in making the diagnosis, assessing for adenoid involvement and checking for polyps.
Plain x-rays have no role in the diagnosis of paediatric chronic rhinosinusitis and do not correlate with CT scan findings. A CT scan is the only available method to determine whether chronic rhinosinusitis is present in addition to chronic adenoiditis. CT is reserved for patients in whom surgery is being considered.
Management
The initial management of children with chronic rhinosinusitis is medical. Nasal saline irrigations twice a day are beneficial, although adherence can be poor. Intranasal corticosteroids (e.g. mometasone 50 µg in each nostril daily) are also recommended. Oral antibiotics are indicated, and oral corticosteroids should be considered. Oral antihistamines and decongestants are not indicated.
Antibiotic therapy is recommended for three to 12 weeks. Initial empirical treatment should transition to culture-directed antibiotic therapy. Doses should be weight appropriate. Amoxicillin–clavulanate or a second- or third-generation cephalosporin are first-line antibiotics. If the patient is allergic to penicillin and cephalosporins then using a macrolide or clindamycin is appropriate.5
If these medical measures fail then surgical intervention should be considered. In children aged up to 12 years, adenoidectomy alone can be very effective. The adenoids are believed to be obstructive or serve as a reservoir for bacterial growth. Research suggests that 70% of children with chronic rhinosinusitis will improve after an adenoidectomy.6 Maxillary sinus irrigation at the time of the adenoidectomy may be helpful. Persistence of symptoms despite an adenoidectomy may justify endoscopic sinus surgery.
Conclusion
Patients with chronic rhinosinusitis can be challenging to treat successfully. Even when symptoms are successfully treated, relapses are common. Many new treatments not mentioned in this summary are under investigation, but cannot be recommended before further evaluation for efficacy and safety. A strong partnership between the patient’s GP and specialist is often needed over a long period to successfully manage patients with this disease. MT
References
- Orlandi RR, Kingdom TT, Hwang PH, et al. International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 2016; 6 Suppl 1: S22-S209.
- Sethi DS, Winkelstein JA, Lederman H, Loury MC. Immunologic defects in patients with chronic recurrent sinusitis: diagnosis and management. Otolaryngol Head Neck Surg 1995; 112: 242-247.
- Costa Carvalho BT, Nagao AT, Arslanian C, et al. Immunological evaluation of allergic respiratory children with recurrent sinusitis. Pediatr Allergy Immunol 2005; 16: 534-538.
- Shapiro GG, Virant FS, Furukawa CT, et al. Immunologic defects in patients with refractory sinusitis. Pediatrics 1991; 87: 311-316.
- Antibiotic Expert Groups. Therapeutic guidelines: antibiotic. Version 15. Melbourne: Therapeutic Guidelines; 2014.
- Brietzke SE, Brigger MT. Adenoidectomyoutcomes in pediatric rhinosinusitis: a meta-analysis. Int J Pediatr Otorhinolaryngol 2008; 72: 1541-1545.