Klinefelter syndrome. A diagnosis not to forget
Klinefelter syndrome affects about one in 550 Australian men, but only half of those affected are ever diagnosed. It is an important cause of male infertility and hypogonadism, and diagnosis enables optimal treatment and outcomes for affected men.
Klinefelter syndrome (KS) is the most common chromosomal disorder in men. Almost 80 years after the clinical syndrome was described and 60 years since the genetic cause was identified,1 about 50% of men with KS remain undiagnosed throughout their lifetime.2
Morbidity and mortality are increased in men with KS,3 and clinical features include hypogonadism, infertility, altered fat distribution, cardiovascular disease, osteoporosis and learning difficulties. Microdissection testicular sperm extraction (microTESE) now offers an effective fertility treatment option in about 40% of men with KS.
Although all men with KS should be under specialist care, GPs have a vital role in detecting those who may be affected and in managing key aspects of chronic care, including prescribing and monitoring ongoing testosterone replacement therapy. This article focuses mainly on the investigation and management of KS in adult men.
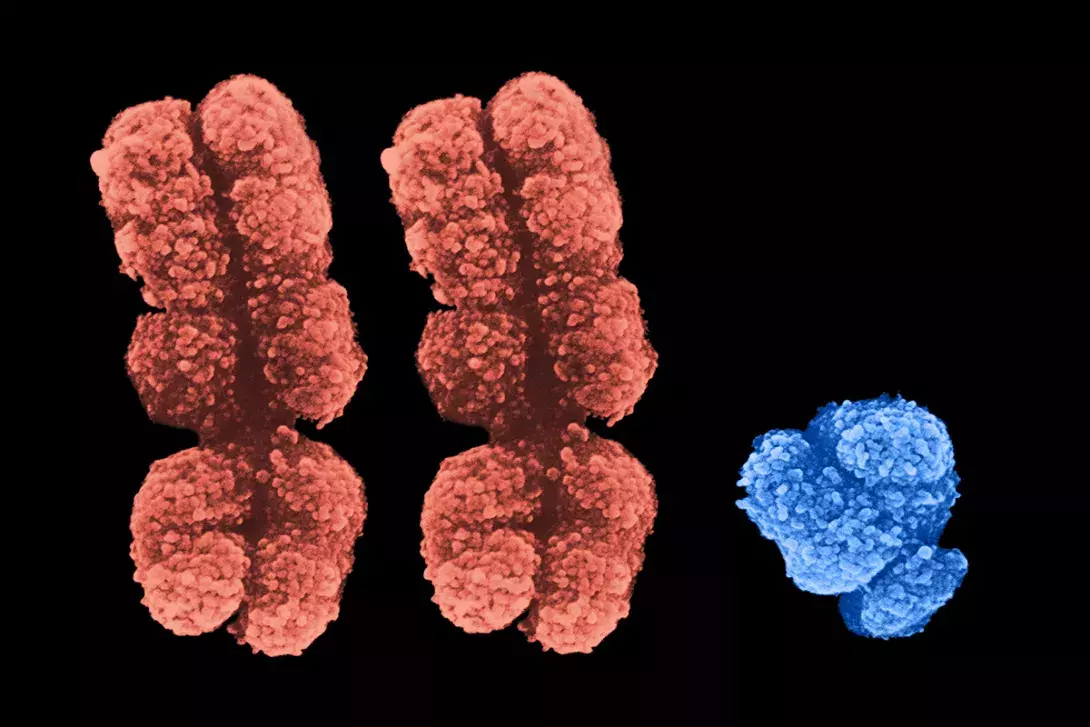
Cause of KS
KS is characterised by one or more additional X chromosome(s).3 About 85 to 90% of men with KS have a 47,XXY karyotype and 10 to 20% have a mosaic karyotype such as 46,XY/47,XXY, or other rarer but typically more severe forms such as 48,XXXY. KS occurs randomly and it is rare to have affected siblings or other family members. The only known risk factor is maternal age above 40 years,4 but the additional X chromosome has an equal chance of being maternal or paternal in origin. For those men with KS who father male offspring with their own sperm, their sons are not thought to have a higher risk of KS.
Clinical features
Patients with KS may present to GPs at any age. Men with KS have small testicles and primary hypogonadism. Infertility is a common presentation leading to the diagnosis. Other clinical features vary and are not always readily apparent. They can include tall stature, reduced facial and body hair, gynaecomastia, feminine fat distribution, varicose veins and learning difficulties. Men may present with low libido or other symptoms of hypogonadism, infertility or fracture.
Children and adolescents may have learning or behavioural difficulties. Puberty may be delayed and/or pubertal features may differ from normal – for example, testicles remain small, tall stature, gynaecomastia (seen in only about 50% cases) or a feminine fat distribution.
Examination should include measurement of height, weight and blood pressure and testicular examination, as well as looking for other clinical features of KS, as summarised in the Figure. The low diagnosis rates of KS may relate in part to the lack of routine examination of the testicles by doctors and, perhaps, a lack of awareness among many men about normal testicular size.
Testing for KS
There is no screening program for KS. Antenatal diagnosis is possible via some (nonfunded), noninvasive prenatal screening tests, typically performed at around 10 to 12 weeks’ gestation. KS can also be diagnosed at amniocentesis or chorionic villous sampling undertaken for other reasons.
Postnatal diagnosis of KS is by karyotype analysis (peripheral blood test). Some pathology providers have an out-of-pocket charge for this test, while others do not. Karyotype results are usually available one month after sample collection.
Other tests in men with suspected KS can include those listed below.
- Fasting, morning (about 8 to 9 am), serum testosterone level. Testosterone is expected to be low or low–normal in men with KS.
- Serum luteinising hormone (LH) and follicle-stimulating hormone (FSH) levels. In KS, both LH and FSH levels rise from mid-puberty and are markedly elevated in adulthood.
- Full blood examination. Haemoglobin and haematocrit may be mildly suppressed in men with hypogonadism and increase when they are taking testosterone therapy. Polycythaemia may occur, particularly in smokers on intramuscular testosterone therapy.
- Prostate specific antigen (PSA) test. Men with KS are not at elevated risk of developing prostate cancer, so routine discussion on PSA testing is appropriate. PSA is monitored in association with testosterone replacement therapy.
- Tests related to increased risk of cardiovascular disease and osteoporosis. Such tests include measurement of glucose and HbA1c levels, lipid profile, renal and liver function and vitamin D level. Thyroid function tests are recommended at the time of diagnosis of KS, and if normal they do not need to be repeated routinely.
- Semen analysis. Over 95% of men with KS will have azoospermia (no sperm seen in semen sample). KS is the most common cause of non-obstructive azoospermia.
- Dual energy x-ray absorptiometry (DXA) scan. KS is usually diagnosed in adulthood, by which time many years of hypogonadism may have led to osteopenia or osteoporosis, which is expected to improve with testosterone replacement therapy. If needed, repeat DXA scans for men with hypogonadism are rebateable under Medicare 12 months after their previous scan.
Treating KS
There is no cure for KS, but many features of the condition can be effectively treated.
Testosterone replacement therapy
Testosterone replacement therapy is the mainstay of treatment and improves many aspects of KS, but not fertility or gynaecomastia. If KS is diagnosed in childhood or adolescence, the timing of commencement of testosterone therapy is based on factors such as a rising LH level, as well as parameters of growth and virilisation through puberty and/or presence of gynaecomastia. Testosterone therapy is continued lifelong, with ongoing monitoring throughout.
If fertility treatment is desired, depending on the patient’s age at diagnosis and if azoospermia is confirmed, consideration should be given to surgical sperm retrieval via microTESE (see below) before testosterone therapy is started or after about six months’ withdrawal in men already on testosterone replacement therapy.
The Table summarises the commonly used testosterone preparations in Australia, and Box 1 provides some practical points on prescribing testosterone.5-7
Fertility treatment
Men with KS account for 1 to 2% of patients with male factor infertility, and 10% of those with azoospermia.8 For men with KS who desire to have children, there are two main options:
- donor sperm – use of sperm from a known or anonymous donor
- microTESE with intracytoplasmic sperm injection (ICSI).
MicroTESE combined with ICSI directly into an ovum provides the possibility of men with KS to have biological children. MicroTESE involves a general anaesthetic, externalisation of the testes from the scrotum, incision and opening of each testis. This is followed by careful microscopic examination, looking for sections of seminiferous tubule that may contain sperm – these generally appear more plump and a slightly richer colour than tubules not containing sperm. Excised sections are examined by an embryologist in theatre, and if sperm are found these can be taken back to the fertility laboratory to be injected into an ovum and/or frozen for future use.
Sperm retrieval and live birth rates from microTESE are about 40 to 45% in men with KS.9 There are no known parameters that predict the success of microTESE surgery. KS is a primary cause of infertility and gonadotrophin pretreatment before surgery with human chorionic gonadotrophin (hCG) and FSH does not increase the success rates of surgery.10 Interestingly, most of the sperm in men with KS isolated during microTESE have a normal chromosomal content and male offspring do not have KS.
One of the key issues for Australian men who wish to access this treatment option remains the limited number of trained surgeons and significant cost of the procedure and associated fertility treatments.
Psychological treatment
Patients with KS can face a number of challenges and psychosocial impacts are common.11 Psychologist input can have an important role in treatment for affected boys and men. Fertility-specific counselling is also available from all major fertility treatment providers.
Educational support and speech and language therapy
Learning difficulties and speech and language deficits are common in those with KS.12 Boys and young men presenting with these issues provide an important opportunity for GPs to consider the possibility of KS. Box 2 lists some websites providing information and support for men with KS.
Breast tissue removal
Half of all men with KS have gynaecomastia,13 which is not responsive to medical therapy. Treatment, if desired, is surgical removal of the breast tissue by a plastic surgeon. This procedure is not typically available through the public health system in Australia and cost can be prohibitive for many men.
Conclusion
KS affects one in 550 Australian men, yet half of those affected remain undiagnosed. Patients with KS have increased morbidity and mortality compared with men in the general population. Key clinical features include primary hypogonadism, small testicles and infertility and, in some, learning difficulties and increased cardiovascular risk. MicroTESE surgery provides many men with KS the chance to genetically father children, although access and cost remain significant barriers to this treatment.
All men with KS should be under specialist care; however, GPs have a vital role in detecting those who may be affected and in managing key aspects of chronic care, including ongoing prescribing and monitoring of testosterone replacement therapy. MT
