Eyelid lesions: a clinical approach for general practice
Eyelid lesions can range from benign lumps to malignant and potentially blinding and deadly disease, if missed. Initial presentations commonly take place in the primary healthcare setting, therefore early recognition of suspicious eyelid lesions is crucial.
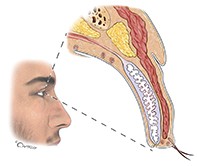
An understanding of eyelid margin structures is necessary for diagnosis of an eyelid lesion. Structures include the skin, subcutaneous tissue, orbicularis oculi muscle, tarsus, retroseptal fat pads and the conjunctiva. Adnexal structures include eyelashes, glands of Zeis and Moll, glands of Wolfring and Krause, meibomian glands and the associated vascular and lymphatic supply (Figure 1).
Clinical assessment
Clinical assessment begins with history. This should include symptoms (i.e. redness, pain and discharge), duration and progression of lesion, any visual disturbance (specifically reduced visual acuity, distortion or diplopia) and past medical history with a focus on history of skin cancer or other cancers, skin radiation and immunosuppression. Lesions can be described using the classic ‘ABCD’ method of evaluation – asymmetry, border irregularity, colour variation and diameter.1
Signs of malignancy include rapid growth, skin ulceration, inflammation, distortion of normal eyelid anatomy and eyelash loss, abnormal colour and texture, and bleeding. Other ominous signs of possible orbital invasion include double vision or globe displacement. Check for cervical lymphadenopathy and involvement of cranial nerves II-VII. In contrast, benign lesions are typically slow growing (i.e. they may be present for more than six months with no change in appearance), noninflammatory in appearance and do not usually cause disruption of lid margin contour. When in doubt, the patient should be referred to an ophthalmologist or oculoplastic surgeon for biopsy and further management as appropriate. It is crucial to obtain photographic documentation of the lesion (when possible) to record its progression.
For ease of clinical approach, eyelid lesions can be broadly classified into:
- inflammatory
- infectious
- neoplastic.
- Neoplastic eyelid lesions can be further divided into:
- benign
- premalignant
- malignant.
Inflammatory eyelid lesions
Hordeolum and chalazion
Acute inflammations of the glands of Zeis result in the formation of a stye (hordeolum externum). These behave like a small pimple at the base of the eyelash. Inflammation of the meibomian glands may be acute (hordeolum internum) or chronic (chalazion) (Figure 2). In the acute phase, a hordeolum internum appears as a red, swollen and tender eyelid lump in the region of the tarsus. These lesions can be very painful. More chronic inflammation of the meibomian gland (chalazion) typically presents as a slowly enlarging nontender eyelid nodule.
For small, localised disease without evidence of cellulitis, warm compresses, applied for 10 minutes four times per day with light massage over the lesion, should be tried before commencing oral antibiotics. If the lesion is painful and tender, is draining or if there is evidence of cellulitis, consider a short course of oral antibiotics targeting Gram-positive bacterial infections such as Staphylococcus aureus. If a chalazion worsens despite systemic antibiotics, and if well localised, referral to an ophthalmologist for incision and curettage may be required.
Infectious eyelid lesions
Molluscum contagiosum
These lesions, caused by DNA poxvirus, are characterised by multiple dome-shaped, painless, umbilicated shiny nodules on the skin including the eyelids, with or without conjunctivitis (Figure 3). The appearance of bumps is characteristic and therefore diagnosis is usually clinical. Molluscum contagiosum often affects children, and more pronounced cases may be seen in immunocompromised patients. In this setting, lesions can become large and affect sight.2
As the name suggests, molluscum contagiosum is contagious and can spread via direct contact. Lesions will resolve over time, but this can take several months to years. When associated with chronic conjunctivitis, molluscum contagiosum should be removed by simple excision, incision and curettage or cryosurgery. More recently, pulsed dye laser has been used to treat these lesions.3,4
Neoplastic eyelid lesions
Benign
Benign eyelid lesions can be categorised into cystic (sudoriferous cyst, sebaceous adenoma, epidermal inclusion cyst), solid (squamous cell papilloma, seborrhoeic keratosis), pigmented (naevi) and vascular lesions (haemangiomas).
Sudoriferous cyst
These lesions are adenomas of secretory cells of the glands of Moll (Figure 4). They appear as translucent, bluish, solitary smooth cysts located along the lid margin. Referral should be made to an ophthalmologist for marsupialisation if the cyst is superficial or for complete excision for deeper cysts.
Sebaceous adenoma
Adenoma of the sebaceous glands of the eyelid arises from glands of Zeis and sebaceous glands of the caruncle. These lesions typically present as yellowish papules on the face, scalp or trunk. They may resemble basal cell carcinoma (BCC) or seborrhoeic keratosis. Management includes complete excision, cryotherapy or ablation with carbon dioxide laser. Patients with multiple sebaceous adenomas could have an increased risk of visceral malignancy (Muir-Torre syndrome) and should undergo a thorough systemic evaluation.5
Epidermal inclusion cyst
These lesions are round or oval dome-shaped cysts filled with keratin, localised superficially under the eyelid skin (Figure 5). Because their natural tendency is to enlarge, complete surgical excision is recommended.
Squamous cell papilloma
These are soft, skin-coloured lesions that may be smooth, rounded or pedunculated (Figure 6). They may enlarge or multiply over time. They often spontaneously regress, although occasionally squamous cell carcinomas (SCCs) can appear papillomatous. Thus, excisional biopsy should be performed for suspicious lesions.
Seborrhoeic keratosis
These are characterised by brown-black, well circumscribed crust-like lesions, usually slightly elevated, with or without surrounding inflammation (Figure 7). They often affect middle-aged or elderly patients and may be removed by shave biopsy or, more readily, by cryotherapy applied in a dermatological fashion by liquid nitrogen sprayed onto the lesion, ensuring protection of the eye.
Melanocytic naevus
These lesions are composed of incompletely differentiated melanocytes that can clump at the epidermis. Most naevi appear in childhood and may enlarge during puberty. They present as well-circumscribed lesions, usually round or oval with uniform pigmentation (Figure 8). Melanomas may develop within pre-existing naevi, therefore suspicious lesions should be biopsied.
Capillary haemangioma
Cutaneous capillary haemangiomas typically present as red, raised lesions (Figure 9). The natural course of capillary haemangioma is initial enlargement followed by spontaneous regression. Therefore, treatment is only initiated for lesions that cause obstruction of the visual axis. Systemic beta blockers form first-line treatment. Other treatment options include the use of oral or injected corticosteroids.6
Premalignant
Actinic keratosis
These present as erythematous, scaly flat or raised lesions (Figure 10). They are typically found in middle-aged or elderly patients with fair complexions, often in sun-exposed areas. There is low risk of malignant transformation (less than 1%).7 Nonetheless, excisional biopsy is usually recommended to establish a diagnosis. Multiple lesions can be managed with cryotherapy or imiquimod 5% cream (because of the irritant effect of imiquimod on the eye, great care must be taken if the lesion is near the eye).
Keratoacanthoma
These lesions are regarded as low-grade SCCs. They often present as a flesh-coloured, raised lesion on the lower eyelid and rapidly grow into a dome-shaped nodule with a central crater filled with keratin. Although keratoacanthoma can spontaneously involute and regress over three to six months, the current recommendation is for histological diagnosis and complete surgical excision.8
Malignant
Basal cell carcinoma
BCC is the most common malignant neoplasm in the periocular region. It is usually found in the lower eyelid of middle-aged or elderly patients (Figure 11). Although it rarely metastasises, BCC can be locally invasive, especially when the lesion is located in the medial canthus.
There are two forms of BCC – the classic nodular type and the morpheaform type. The nodular type is usually found on the lower lid at the medial canthus as firm, raised pearly nodules with fine telangiectasias. The morpheaform type is more locally aggressive. These lesions lack ulceration and appear as firm, flat, indurated white-to-yellow plaques with indistinct margins. They are more difficult to excise and may result in a large eyelid defect.
Orbital invasion is rare (less than 5%) and often occurs for lesions located in the medial canthus (inner corner of the eyelids). Signs of orbital invasion may include a fixed orbital mass, restrictive eye movement and globe displacement. As well as assessing the presence or absence of local lymphatic spread of malignant eyelid lesions to regional nodes, assessment of a potentially malignant lid lesion should include exclusion of associated perineural spread. This is achieved clinically by assessing cranial nerves II, III-VI, V and VII. CT or MRI is indicated to determine the extent of disease. For noninvasive lesions, treatment is primarily with Mohs micrographic surgery followed by eyelid and facial reconstruction if required.
Squamous cell carcinoma
SCC is the second most common eyelid malignancy, often found in the lower lid or especially the upper lid, in contrast to BCCs (Figure 12).
Predisposing factors include ultraviolet light exposure, arsenic exposure, human papillomavirus and immunocompromised status.9 Similar to BCC, an SCC often presents as a painless nodular lesion with irregular rolled edges, pearly borders, telangiectasias and central ulceration.
For localised lesions, surgical excision with clear margin is the mainstay of treatment. Metastasis of SCC is commonly through the lymphatic system, invading along the trigeminal, oculomotor and facial nerves. Hence, initial examination should exclude signs of perineural spread in examining cranial nerves II, III-VI, V and VII. SCC with perineural involvement has a high recurrence rate of up to 50%, therefore postoperative radiotherapy has been suggested for all SCCs with perineural invasion.10
Sebaceous gland carcinoma
Sebaceous gland carcinoma is a rare, highly malignant and potentially lethal tumour originating either from the meibomian glands or glands of Zeis. It is often found in the upper lid of middle-aged or elderly patients. These lesions appear as yellow discolouration from lipid content, and can mimic blepharoconjunctivitis, chronic chalazia or particularly recurrent chalazia after repeated surgery, BCC and SCC. Eyelash loss and distortion of the eyelid margin are common (Figure 13). The presence of these signs in a lesion that initially resembles a chalazion or that presents with a unilateral chronic blepharoconjunctivitis should warrant biopsy.
Local invasion into surrounding conjunctiva is common, seen in 44 to 80% of patients.11 Patients are best referred to an ophthalmologist. Pentagonal full-thickness excision or multiple map punch biopsies of surrounding conjunctiva are required due to the potential for multifocal involvement with skin lesions.11 The presence of conjunctival invasion indicates a higher risk for orbital involvement; CT or MRI may be indicated to delineate the extent of the lesion. The mainstay of treatment is surgical excision, with wide local excision for localised lesions and exenteration for large, deeply invasive lesions or lesions with significant bulbar conjunctival involvement. Consider sentinel lymph node biopsies for Stage T2b or worse (i.e. tumour is more than 10mm or involves full eyelid thickness).
Melanoma
Melanoma of the eyelid is rare and accounts for less than 1% of all cutaneous malignant melanomas. It has peak prevalence in people between 50 and 80 years of age. It lacks pathognomonic features. Presentations may range from a flat tan lesion with irregular, indistinct borders to an elevated lesion with a combination of colours that includes tan, black, grey, pink, blue or white. It can also present as amelanotic lesions. Patients should be referred to an ophthalmologist or oculoplastic surgeon. A punch biopsy is often used to establish the diagnosis followed by a wide local excision or Mohs micrographic surgery for localised lesions. Sentinel lymph node biopsy should be considered for melanomas more than 1.0mm in thickness.
Merkel cell carcinoma
Merkel cell carcinoma is a rare and highly malignant neuroendocrine tumour, with rapid growth to more than 10 mm within two to three months. Two-thirds of patients present with lymph node metastasis at diagnosis, or within 18 months from initial therapy.12 The other third have local recurrences and satellite lesions. Merkel cell carcinoma occurs more commonly in women between 70 and 80 years of age, and has a predilection for the upper eyelid. It often appears as a painless, reddish or purplish vascularised solitary nodule without ulceration of the overlying skin.
Once a histological diagnosis is made, wide local excision with 5mm margins followed by frozen-section control of margins is considered the gold standard. Surgery in combination with local adjuvant irradiation has been to shown to lead to lower rates of local and regional recurrence in patients with positive lymph node disease. Research to establish targeted and immunological therapeutic options is ongoing for the treatment of advanced merkel cell carcinoma.12
Conclusion
Familiarity with common eyelid presentations in the primary healthcare setting is key to preventing morbidity and mortality from these lesions. A detailed history and examination with photographic documentation will assist in management and follow up. It is helpful to approach diagnosis of eyelid lesions in the broad categories of inflammatory, infectious and neoplastic (benign or malignant). When in doubt, prompt referral to an ophthalmologist will facilitate tissue diagnosis and management. See the Practice Points Box for helpful hints. MT