What’s the diagnosis?
Rapid onset of erythroderma in a 65-year-old man

Case presentation
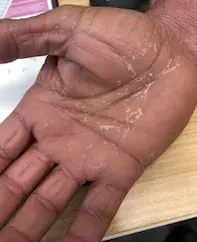
A 65-year-old man presents with mildly pruritic, erythematous plaques in a generalised distribution (Figure 1). He noticed the eruption on his distal arms, face and trunk three weeks ago, but it has recently started to involve his hands (Figure 2). He does not take any regular medications, and he denies any past history of eczema or psoriasis.
On examination, the patient has erythroderma but no rash on his extensor surfaces or gluteal cleft. There is thickening of the skin of his palms with overlying scale and some orange discolouration.
Differential diagnoses
Conditions to consider among the differential diagnoses include the following.
- Psoriasis. This common inflammatory skin condition presents with erythematous plaques overlying the extensor surfaces. Patients typically develop psoriasis before the age of 45 years, which makes it a less likely diagnosis in this case. In addition, the patient’s symptoms have progressed more rapidly than would be expected in psoriasis.
- Cutaneous T cell lymphoma. Cutaneous T cell lymphoma (CTCL) can present with widespread erythema, such as in Sézary syndrome, or with discrete scaly plaques, as in the plaque stage of mycosis fungoides. The hands are not a classic site for CTCL, making it a less likely diagnosis in this case.
- Drug hypersensitivity. Drug eruptions can be polymorphic in presentation, and clinicians should have a high index of suspicion for a drug trigger in patients who present with widespread erythema. Classic drug hypersensitivity reactions tend to present with maculopapular eruptions; the palmar surfaces are not usually affected. It can be difficult to elicit the triggering agent, and all medications started in the past three months (even if now ceased) should be considered. In this case, the palmar keratoderma and lack of any significant drug history made hypersensitivity less likely.
- Pityriasis rubra pilaris (PRP). This is the correct diagnosis. This scaly, reddish-orange eruption can be widespread or localised in distribution. The exact cause of PRP is unknown, although some cases may be inherited or have a drug precipitant. Patients with psoriasis can present with palmoplantar symptoms, making it difficult to differentiate between psoriasis and PRP. The erythema in PRP tends to have ‘islands of sparing’ (localised areas of unaffected skin), which can assist in making the diagnosis. Presentations of CTCL can be difficult to differentiate from PRP, and biopsy can be of assistance. Other features that may be present in CTCL include ulceration and poikiloderma, which are not present in PRP.
Investigations and diagnosis
Histological features can help to differentiate PRP from its clinical mimics. At least one skin sample should be obtained for haematoxylin and eosin staining; multiple samples can improve diagnostic yield. An alternating orthokeratosis and parakeratosis is usually seen, along with acanthosis and psoriasiform hyperplasia in the epidermis. The neutrophilic infiltrate and spongiform epidermal changes associated with psoriasis are not present; with PRP there is usually a sparse mixed infiltrate. The follicular plugging seen clinically is also observed in the sample, with parakeratosis at the edge of the follicular orifice.
Management
PRP is a rare condition, and there are limited high-quality trials assessing the effectiveness of treatment. Currently recommended therapies for PRP are similar to those used in psoriasis. For patients requiring systemic therapy, oral retinoids (acitretin/isotretinoin) are most effective, although methotrexate (off-label use) and ultraviolet B phototherapy can be used in some cases. Topical corticosteroids can be useful as an adjunct therapy or, in patients with limited disease, as monotherapy.
There are case reports describing successful off-label treatment of PRP with biological agents such as infliximab or adalimumab, but these agents are reserved for treatment-resistant disease.1,2 In patients with HIV-associated PRP, antiretroviral therapy should be started as well as treatment for PRP. Blood tests, including full blood count, liver and renal function tests and screening for hepatitis B and C, HIV and tuberculosis should be performed in severe cases, before starting immunosuppressive therapy.
Classic adult PRP, as described in this patient, is the most common subtype of PRP (about 55% of cases) and has an excellent prognosis, with up to 80% of patients experiencing spontaneous remission at three years.3 The prognosis for the classic juvenile subtype is similarly good. Other, less common subtypes of PRP have different prognoses. Atypical adult PRP has a poor prognosis, with less than 20% of patients experiencing remission at three years.4 HIV-associated PRP is also quite resistant to treatment.
Outcome
The patient was started on oral acitretin 50 mg once daily for one month, which was reduced to 37.5 mg daily for one month. He had an excellent response, with approximately 80% response at two months.
References
1. Adnot-Desanlis L, Antonicelli F, Tabary T, Bernard P, Reguiaï Z. Effectiveness of infliximab in pityriasis rubra pilaris is associated with pro-inflammatory cytokine inhibition. Dermatology 2013; 226: 41-46.
2. Walling HW, Swick BL. Pityriasis rubra pilaris responding rapidly to adalimumab. Arch Dermatol 2009; 145: 99-101.
3. Klein A, Landthaler M, Karrer S. Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol 2010; 11: 157-170.
4. Wang D, Cui-Lian Chong V, Chong W-S, Oon HH. A review of pityriasis rubra pilaris. Am J Clin Dermatol 2018; 19: 377-390.

