Percutaneous vertebroplasty
Vertebral compression fracture is a common manifestation of osteoporosis, leading to significant back pain and disability. About 16% of postmenopausal women will have such a fracture. Until recently, treatment has comprised bed rest, analgesics, bracing and rehabilitation. Now, the use of percutaneous vertebroplasty in osteoporotic vertebral compression fractures is becoming increasingly important. The procedure is available in most capital cities and usually provided by interventional radiologists with experience in neurospinal interventions.
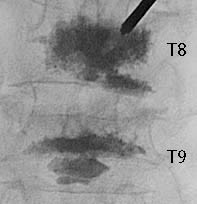
Percutaneous vertebroplasty involves the injection of polymethylmethacrylate (a bone cement) into a vertebral body. It was pioneered in France in the 1980s for the treatment of vertebral angioma. Subsequently, it was shown to be useful also in the treatment of other vertebral malignant tumours.
The aims of treatment with percutaneous vertebroplasty for osteoporotic compression fractures have been resolution in pain, improved mobility and bone strengthening.