Venous thromboembolism. Applying new guidelines in primary care
Venous thromboembolism (VTE) is a potentially life-threatening diagnosis commonly encountered in the primary care setting. New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of VTE provide physicians with evidence-based guidance on this challenging area of medicine.
- The Thrombosis and Haemostasis Society of Australia and New Zealand guidelines on management of venous thromboembolism (VTE) provide succinct, evidence-based guidance on diagnosing and managing deep vein thrombosis and pulmonary embolism.
- The diagnosis of VTE rests on radiological findings. Imaging is not required in patients with a low clinical likelihood and a negative d-dimer test result.
- Almost all patients with VTE require anticoagulation therapy.
- Apixaban and rivaroxaban are now the preferred anticoagulants in most patients with VTE, although low molecular weight heparin remains the agent of choice in pregnant and breastfeeding women.
- Duration of anticoagulation is determined by risk of progression and recurrence and must be weighed against bleeding risk.
- Inherited thrombophilia rarely influences management decisions, and routine testing is not indicated.
- Patients should be monitored to ensure ongoing benefit of anticoagulation and to identify chronic complications of VTE.
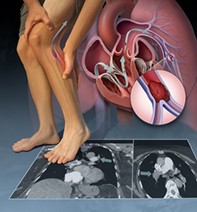
The term venous thromboembolism (VTE) encapsulates deep vein thrombosis (DVT) and pulmonary embolism (PE). These diagnoses may present in a disparate manner, from life-threatening episodes that require urgent hospitalisation and anticoagulation plus additional therapies, to asymptomatic episodes that may not require treatment at all. Presentation may be nonspecific, and a high index of suspicion is required when the diagnosis is considered. The cornerstone of management is anticoagulant medication. Nonvitamin K oral anticoagulants (NOACs) provide a safe, convenient option for patients and clinicians, and are now preferred to warfarin in most patient groups. Primary care physicians play an important role in timely diagnosis and evidence-based treatment decisions, which may reduce mortality and morbidity as well as the large economic costs associated with these challenging diagnoses.
The Thrombosis and Haemostasis Society of Australia and New Zealand (THANZ) are a group of clinicians and scientists whose mission statement includes the development of policies that improve health care. The THANZ guidelines on the diagnosis and management of VTE provide succinct, evidence-based guidance.1 The full guidelines are available online at www.thanz.org.au/resources/thanz-guidelines.
Diagnosis
Radiology: when to test
Symptoms of VTE are nonspecific, and only about 20% of patients suspected of having VTE ultimately have the diagnosis confirmed.2 Thus, objective diagnosis with radiological investigation is always required. Unfortunately, in the primary care setting immediate radiological investigation is not always feasible. In this setting, brief courses (less than 24 hours) of presumptive anticoagulation are appropriate until radiological investigation can be arranged.
Radiological studies are associated with significant cost and inconvenience to patients, especially those living in rural areas (Box). Imaging can be avoided in patients with a negative d-dimer test result and low risk scores as calculated by validated clinical prediction tools (Table 1). The tools with the most evidence to support their use are the Geneva and Wells scores.3 The pulmonary embolism rule out criteria (PERC) are useful in the exclusion of PE; however, they should only be used in young patients (less than 50 years of age), in whom the likely background rate of VTE is about 15% or less.4,5
Radiology: choice of test
The investigation of choice for suspected DVT is venous duplex ultrasound. In Australia, to investigate lower-limb DVT, the entire deep venous system of the leg from groin to ankle is imaged (Figure). A negative study result effectively excludes the diagnosis of lower-limb DVT.6 A two-point compression ultrasound may be helpful to exclude a proximal thrombosis but does not detect distal thromboses, and should always be followed up with serial ultrasound. A second ultrasound within one week from the original imaging is sufficient.
In most patients, CT pulmonary angiography (CTPA) is recommended as the investigation of choice for suspected PE.7 Its worth should be weighed against the significant radiation and nephrotoxic dye exposure. Ventilation-perfusion (VQ) scanning is preferred in pregnant patients and those with renal failure; however, this test is associated with a significant number of indeterminate results. In the setting of an indeterminate VQ finding, the next investigation is determined by the risk-benefit ratio of CTPA. If the risks of CTPA are too high, serial duplex ultrasound of the lower limbs is an effective alternative. The absence of DVT makes embolic events unlikely, and therefore anticoagulation can usually be safely withheld.7
Processes for diagnosing PE and DVT are outlined in Flowchart 1 and Flowchart 2, respectively.
Management
When to treat
Most patients with VTE require anticoagulation therapy. Apart from the rare patient with a contraindication due to bleeding, all proximal DVTs and PEs should be treated. Less clear is the management of isolated distal DVT – thromboses confined to the vessels below the popliteal vein, without associated PE. Symptomatic distal DVT should receive anticoagulation, but the duration may be limited to six to 12 weeks. Those with increased risk for bleeding may have anticoagulation deferred but should be monitored with two duplex ultrasounds over two weeks.8,9 Any thrombosis that progresses during this time should be treated.8,10 Subsegmental PE may be managed with a similar observational protocol in low-risk asymptomatic patients; the THANZ recommend serial bilateral ultrasound examination of the legs at diagnosis and after one week.11
At the other end of the scale, haemodynamic instability resulting from massive PE is associated with high rates of mortality. These patients should be urgently transferred via ambulance to a centre with thrombolysis capabilities.12,13
The benefit of treatment with anticoagulation must be weighed against the risk of major bleeding. The most significant risk for bleeding in patients on anticoagulation therapy is a previous history of bleeding. Anticoagulation should be avoided in most patients with active bleeding or unremedied blood loss over the preceding 30 days.14 Other predictors of bleeding include potential bleeding lesions, recent surgery (within 14 days), severe kidney disease and active cancer. It should be noted that the latter three criteria listed are also risk factors for thrombosis, making the decision to anticoagulate challenging, and often subjective, in these patients. Nevertheless, despite the high level of concern among patients and clinicians, rates of bleeding in patients without risk factors are reassuringly low, in the order of 0.8 to 1.6% per year. Bleeding rates in patients receiving low-dose NOACs were similar to age-matched controls.8,15
Which anticoagulant to use?
The THANZ recommend rivaroxaban or apixaban (both NOACs) in preference to warfarin for the treatment of VTE as there is no requirement for parenteral anticoagulation at initiation.1 Unlike warfarin, these agents require no dose adjustment (after the initial loading phase) or monitoring and are associated with fewer drug interactions and almost no food interactions. The direct antithrombin agent dabigatran requires an initial five-day period of heparin treatment and is not available on the PBS for treatment of VTE.
There are instances, however, in which rivaroxaban and apixaban should be avoided (Flowchart 3 and Table 2). NOACs are eliminated in part by the kidneys, and warfarin is preferred in advanced renal failure. There are limited high-quality data to support NOAC use in patients with weights of 120 kg or more, and these agents should be used with caution in this setting. Metabolism of NOACs is primarily hepatic and they should be avoided in patients receiving strong inhibitors of cytochrome P450 3A4, such as azole antimycotics and protease inhibitors for HIV. Women with childbearing potential should be made aware that NOACs have not been shown to be safe in pregnancy and breastfeeding. Contraceptive measures should be taken in sexually active women who are taking a NOAC, and before conception the NOAC should be replaced with a low molecular weight heparin (LMWH).8 An LMWH should be continued throughout the pregnancy and for the duration of breastfeeding.
There are limited data to guide the use of NOACs in antiphospholipid syndrome (APS), and warfarin is preferred in patients with this condition.16 APS is a rare condition; however, further laboratory testing should be considered before starting a NOAC in a patient with an otherwise unexplained prolonged activated partial thromboplastin time or a history of unprovoked thromboembolism or recurrent miscarriages. Data in patients with active malignancy are still evolving. Studies have suggested that rivaroxaban and apixaban are effective, but may be associated with increased rates of bleeding, especially in patients with mucosal disease.17,18 Nonetheless, due to their convenience, NOACs are increasingly employed in the treatment of cancer-associated VTE. Common anticoagulation regimens and their indications are outlined in Table 3.
Duration of anticoagulation
The optimal duration of anticoagulation for a patient with VTE is determined by the risk of clot progression or recurrence, which must be weighed against the risk of major bleeding (discussed above in ‘When to treat’) in patients who receive long-term anticoagulation (Table 2). Predicting which patients are at risk of further thrombotic events on withdrawal of anticoagulation remains challenging. Two questions are helpful:
- Does the patient have an indication for extended therapeutic anticoagulation?
- Does the patient have an indication for ongoing secondary prevention of VTE?
Patients who have experienced two or more unprovoked thromboses or have a diagnosis of antiphospholipid syndrome or active malignancy generally require indefinite anticoagulation. Secondary prevention of VTE should be considered in patients with a single unprovoked or nonsurgically provoked episode of VTE. There is equipoise in this group of patients, and personal preference should be considered. These patients can receive long-term prophylactic anticoagulation, with low-dose apixaban (2.5 mg twice daily) or rivaroxaban (10 mg daily) after an initial six to 12-month period of therapeutic anticoagulation.15,19 If NOACs are contraindicated, warfarin can be considered. Finally, cessation of anticoagulation after three to six months is appropriate if the patient is accepting of the 30% recurrence rate at five years.8
If the answers to the above questions are ‘no’, anticoagulation can usually be safely stopped after three to six months, or six to 12 weeks in the case of isolated distal DVT (Flowchart 4).8,10
Hereditary thrombophilia rarely influences the indicated duration of anticoagulation. Genetic mutations causing antithrombin, protein C and protein S deficiencies, when associated with a family history of thrombosis, result in increased risk of recurrence, and indefinite anticoagulation is usually indicated in patients with these deficiencies; however, these mutations are rare.20 More common abnormalities such as factor V Leiden and prothrombin gene mutations do not affect anticoagulation duration.21 Thus, hereditary thrombophilia testing in patients without significant family history should be limited to younger patients (less than 45 years of age) with significant unprovoked thrombosis and must be accompanied by suitable counselling. It should be noted that acute thrombosis and anticoagulant medication may interfere with the results of these tests.
Long-term follow up of VTE
On cessation of anticoagulation for DVT, a repeat ultrasound is recommended to assess residual venous obstruction as not all thrombi will completely resolve. Residual clot burden has minimal effect on decisions regarding duration of anticoagulation, although these results serve as a useful baseline. If the patient develops new symptoms, a negative d-dimer test result and unchanged ultrasound findings may be used to exclude recurrent DVT.
Women with a history of VTE should avoid oestrogen-containing contraceptives and oral menopausal hormone therapy (MHT) after discontinuing anticoagulation. Progestin-only contraceptives are generally safe. There is no evidence that using the levonorgestrel intrauterine device increases the risk of VTE. There is also no evidence that transdermal MHT increases VTE recurrence, and it can therefore be considered as a safe replacement for oral MHT.22
Patients receiving anticoagulation indefinitely should be reassessed on a regular basis to ensure they are still deriving benefit from their treatment. Finally, all patients should be monitored for the development of chronic complications of VTE. One in three patients suffers from post-thrombotic syndrome after a lower-limb DVT. The syndrome is characterised clinically by swelling, discomfort, hyperpigmentation and lipodermatosclerosis in the affected limb. Treatment options are, unfortunately, limited. An elastic compression stocking may reduce the swelling and pain but is not tolerated by all patients.23,24
If a patient who has suffered a PE complains of exertional dyspnoea in the ensuing two years, chronic thromboembolic pulmonary hypertension should be considered. A VQ scan to assess residual clot burden and an echocardiogram to assess right heart pressures should be carried out in these patients. If the results are abnormal, the patient should be referred for assessment by a specialist.25
Conclusion
VTEs are challenging diagnoses commonly encountered in the primary care setting. The THANZ guideline is a valuable resource for physicians looking for a pragmatic, evidence-based framework to inform their decision-making. Timely diagnosis and optimal management minimise both unnecessary therapy for minor events, and morbidity and mortality in more significant events. MT