What’s the diagnosis?
Alopecia with dull, broken hairs
Androgenetic alopecia may be very prominent over the vertex of the scalp, but the hair loss is symmetrical and associated with a much slower progressive history (often several years). The fine diameter, miniature hairs associated with androgenic alopecia differ from the broken, lustreless hair seen in this patient.
Alopecia areata is usually characterised by discrete round patches of complete hair loss. The broken hairs show a tapering tip at the surface of the scalp (exclamation mark hairs). Alopecia areata often develops suddenly over a few days. A scalp biopsy reveals lymphocytic inflammation targeting the hair bulbs.
Trichotillomania (the compulsive habit of hair pulling) results in irregular areas of alopecia, often with unevenly broken hairs and black dots at the scalp surface. The changes may be difficult to distinguish from tinea but the absence of pustules, scaling and erythema are clues for trichotillomania. Scalp biopsy in trichotillomania shows follicles with distorted, broken hairs and pigmented hair casts as well as numerous involuting (catagen phase) hair follicles without organisms or significant inflammation.
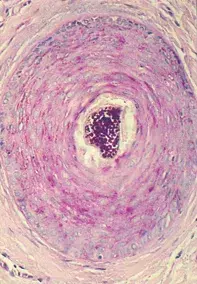
Tinea capitis is the correct diagnosis in this case. The broken hairs seen clinically reflect the presence of fungi within the hair shafts, which leads to easy breakdown. Tinea capitis may also be associated with severe inflammation and a boggy swelling (termed a kerion) if there is a marked immune response to the fungal elements. A biopsy of the scalp revealed numerous spores inside the hair shafts within the hair follicles (Figure 2). Apart from performing a biopsy, the diagnosis of tinea can be established by examining plucked hairs under the microscope as well as by sending hairs for fungal culture. Some fungal species causing tinea capitis fluoresce a yellow–green colour with Wood’s UV light, but this test may be falsely negative. Effective treatment for tinea capitis in adults includes the use of either griseofulvin 500 mg or 330 mg (10 to 20 mg/kg/day for children), ketoconazole 200 mg or itraconazole 100 mg daily for six weeks, or terbinafine 250 mg (5 to 8 mg/kg/day for children) for four weeks. The duration of treatment may vary from case to case.
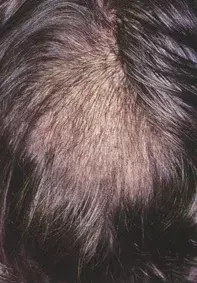
Over a three-month period a 33-year-old man developed a large area of alopecia affecting the left side of the vertex of his scalp (Figure 1). The hairs within the area of alopecia were less dense, broken and had lost their sheen.

