What’s the diagnosis?
A blistering eruption in pregnancy
Pruritic urticarial papules and plaques of pregnancy (also known as polymorphous eruption of pregnancy) often appears in the final trimester, particularly in primigravidas. It is characterised by itchy urticated lesions that may be associated with small vesicles, but not frank blisters. The lesions may commence on the sides of the abdomen within striae and usually spare the palms and soles. Skin biopsy shows superficial lymphocytic inflammation with eosinophils. The results of direct immunofluorescence are negative. The rash often continues to the end of pregnancy but then settles. Usually there is no recurrence in subsequent pregnancies.
Dermatitis may complicate pregnancy and may be due to underlying atopy or to contact reactions or nummular dermatitis. In addition to blisters vesicular eczematous patches are usually evident. Skin biopsy will show upper dermal lymphocytic inflammation with eosinophils, but results of immunofluorescence are negative. A dermatitis may develop at any time during pregnancy, and there may be a prior history of dermatitis.
Prurigo of pregnancy is a term that is used to describe a variety of itchy dermatoses characterised by firm papules that are often excoriated. Some papules are follicular based. The process may develop as an expression of atopy. Scabies may need to be excluded. Skin biopsy shows focal epidermal hyperplasia with lymphocytes and eosinophils. Immunofluorescence is negative.
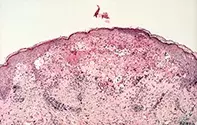
Pemphigoid gestationis is the correct diagnosis in this case. It may develop early in pregnancy, but may be delayed until the last trimester or early in the postpartum period. Skin biopsy revealed an intense subepidermal oedema with blister formation and a mixed inflammatory reaction consisting of lymphocytes and eosinophils (Figure 2). Immunofluorescence of the skin for the presence of antibodies revealed the presence of linear deposits of IgG and complement along the basement membrane zone. The blistering process is due to the development of autoimmune antibodies to the BP180 antigen found in the hemidesmosomal complex in basal keratinocytes. Circulating antibodies can be assayed using ELISA or immunoblotting to specific antigens. Subsequent pregnancies are often complicated by the same eruption. This can be severe and produce extensive blistering requiring systemic treatment. The antibodies may be transferred to the fetus, and short-lived blisters may develop in the newborn. Pemphigoid gestationis may flare but usually settles in the postpartum period. The term herpes gestationis is also used for this condition, but it is best avoided because it may cause confusion with herpes viral infection, which does not play a role. Treatment Mild disease may be controlled by topical corticosteroid creams and oral antihistamines, but if there are frank blisters oral corticosteroids should be used - 15 to 50 mg of prednisone daily may be required to bring the disease under control before the dose is reduced. Careful monitoring of the pregnancy for diabetes and hypertension are required.
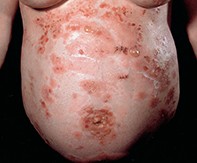
A 26-year-old pregnant woman developed a symmetrical intensely pruritic eruption that commenced around her umbilicus and became generalised in the third trimester. Grouped and annularly distributed blisters were present which broke to produce serous crusts (Figure 1).

