What’s the diagnosis?
Muscle weakness with knuckle erythema

Figure 1. Dorsum of the patient’s hand showing erythema over the knuckles and interphalangeal joints.
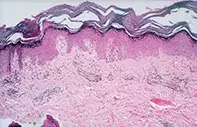
Figure 2. Skin biopsy demonstrating perivascular lymphocytic inflammation and lymphocytes interacting with basal keratinocytes at the epidermal junction.
Differential Diagnosis
Psoriasis of the hands may appear as erythematous and scaly patches on the joints. Careful examination of the nails for pitting and other signs of psoriatic nail dystrophy, arthritis or other lesions of psoriasis will usually establish the diagnosis. General symptoms are usually absent, except in very acute disease. Skin biopsy in psoriasis shows epidermal hyperplasia with neutrophil collections in the stratum corneum and lymphocytic dermal inflammation.
Dermatitis may present on the dorsum of the hands; however, it is often asymmetrical and associated with irritation or pruritus. Vesicles or fissures may be present. Skin biopsy shows epidermal hyperplasia with separation of keratinocytes (spongiosis) and lymphocytic inflammation with eosinophils.
Lupus erythematosus of the hands is usually a manifestation of photosensitivity and involves the dorsal aspect of the hands with relative sparing of the joints. The palms may also be involved. Systemic symptoms such as malaise may be present, but muscle weakness is absent except in mixed connective tissue disease. Biopsy findings may be the same as in this case. Skin immunofluorescence is helpful because it may be positive, with immunoglobulin and complement in a linear granular pattern along the basement membrane zone. Serological tests for lupus are also useful.
Dermatomyositis is the correct diagnosis here. Skin biopsy revealed perivascular lymphocytic inflammation and focal necrosis of basal keratinocytes with vacuolar changes at the epidermal junction (Figure 2). The violaceous erythematous lesions on the knuckles may become atrophic, producing Gottron’s papules. As well as periungual erythema, frayed cuticles with infarcts and haemorrhage may be seen.
Other skin signs, such as periorbital erythema with eyelid involvement and oedema (heliotrope rash), and muscle symptoms are major clues. Apart from skin biopsy, muscle enzyme levels, electromyography, muscle biopsy or muscle MRI are helpful in the diagnosis. In adults, careful review for symptoms and history of malignancy is required because dermatomyositis may be a paraneoplastic phenomenon. CT scan of the chest, abdomen and pelvis may be needed if initial laboratory testing is negative.
Treatment
For purely cutaneous disease, topical corticosteroids, sunscreens and oral hydroxychloroquine (Plaquenil) may be sufficient therapy. For full-blown dermatomyositis, oral corticosteroids, methotrexate or immunosuppressives such as azathioprine, methotrexate or mycophenolate mofetil are usually required to bring the process under control. The aim of treatment is to prevent permanent weakness, contractures and long term dystrophic calcification.
Over a three-month period, a 14-year-old boy developed a facial rash, pruritic erythematous patches on the back of his knuckles and interphalangeal joints, and periungual erythema with focal haemorrhage (Figure 1). This was accompanied by a general malaise and progressive weakness of his proximal limb muscles.

