What’s the diagnosis?
Recurrent dusky skin lesions

Psoriasiform drug reactions present with diffuse scaling and erythema that combine features of psoriasis and dermatitis. A lichenoid histopathology with eosinophils is often found and should prompt a search for a drug-related cause.
Lupus-like drug reactions may be difficult to clinically differentiate from subacute lupus erythematosus, and may present as annular scaling patches on the trunk and limbs. A lichenoid histopathology is found on skin biopsy.
Stevens–Johnson syndrome and drug-related erythema multiforme may present acutely with widespread targetoid lesions that may blister and are often associated with prominent mucous membrane involvement. Blindness and nail loss may develop as permanent sequelae due to scarring. The lichenoid reaction often targets sweat ducts when drugs are involved.
Toxic epidermal necrolysis presents with extensive painful burn-like blisters with loss of skin and mucous membrane. The skin biopsy shows extensive epidermal necrosis with scant lymphocytic inflammation. Intensive care management equivalent to that used for extensive burns is required for management.
Fixed drug reaction is the correct diagnosis in this case, and is characterised by recurrent tender erythematous lesions which may blister and recur at the same sites within hours of drug re-exposure. Common drugs inducing this reaction include the sulfonamides, tetracyclines, phenolphthalein, quinine and analgesics. The reaction is self-limited, and the main challenge is to identify the offending agent.
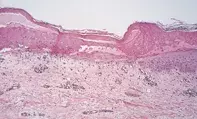
A 35-year-old woman developed a series of tender erythematous lesions with a dusky centre on her trunk (Figure 1) and upper limbs within hours of commencing sulfamethoxazole–trimethoprim for a recurrent urinary tract infection. Similar lesions had developed years previously at the same sites. Skin biopsy showed extensive epidermal necrosis with a superficial lymphocytic perivascular infiltrate and lymphocyte-associated keratinocyte necrosis (Figure 2).

