What’s the diagnosis?
Widespread tense blisters

Bullous insect bite reaction may present as tense blisters with an erythematous base. Insect bites tend to be asymmetrical, often grouped and concentrated on exposed sites. Individual lesions resolve spontaneously. Biopsy shows superficial and deep lymphocytic inflammation and eosinophils, and immunofluorescence is negative.
Bullous fixed drug reactions have a history of recurrent skin lesions localised to the same sites, including mucous membranes. The blisters usually occur in the centre of targetoid lesions and resolve spontaneously, leaving hyperpigmentation in their wake. Skin biopsy shows lymphocytic inflammation with epidermal necrosis, giving a lichenoid pattern. Immunofluorescence is negative.
Cicatricial pemphigoid presents primarily on mucous membranes such as the conjunctiva or oral cavity, but it may involve the skin, particularly on the head and neck. The lesions are often localised and heal with scars. Biopsy shows subepidermal blistering with a prominence of neutrophils. Immunofluorescence shows an identical pattern of linear deposits along the basement membrane zone.
Bullous pemphigoid is the correct diagnosis in this case. It is an autoimmune process in which circulating antibodies are directed to antigens BP1 (230 kDa) and BP2 (180 kDa), localised to the hemidesmosomes that bind basal keratinocytes to the basement membrane zone. The circulating antibodies can be detected or monitored by indirect immunofluorescence or now with ELISA method on blood. The blisters are often widespread (but usually spare the mucous membranes) and they may continue to appear over months to years. For widespread disease, oral prednisone (>0.75 mg/kg/day) is the treatment of choice and may require the addition of immunosuppressive agents such as azathioprine or mycophenolate mofetil. Some patients will respond to combinations of minomycin and nicotinamide. For some patients with generalised disease, potent topical corticosteroids (50 g/day) has been effective. Topical or intralesional steroids are useful for localised lesions.
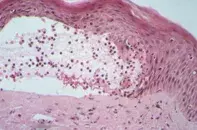
Over a three-month period, a 52-year-old woman developed widespread pruritic, tense blisters involving her trunk and limbs (Figure 1). In some areas the blisters were on an urticarial base. There were no mucous membrane lesions. Skin biopsy showed a subepidermal blister containing lymphocytes and numerous eosinophils (Figure 2). Immunofluorescence showed linear deposits of IgG and C3 along the basement membrane zone at the epidermal junction (Figure 3).

