Strategies to increase vaccination rates in the elderly

Coverage levels for recommended vaccines in older adults fall well below those in children. An important driver of vaccination is a recommendation from the person’s GP. Tips for talking about vaccines, addressing patient misconceptions and specific practice strategies may help GPs increase vaccination rates among their older patients.
Note
This is an online update of the original version of this article that was published in the Supplement of the February 2019 issue of Medicine Today. This update was prepared for World Immunization Week 2024.
- Vaccination rates for recommended vaccines in older adults fall well below rates seen in children.
- One of the most influential drivers of vaccination is a recommendation from the person’s GP.
- GPs can help increase vaccination rates by informing their older patients about the severity of vaccine-preventable diseases and the safety and effectiveness of vaccines.
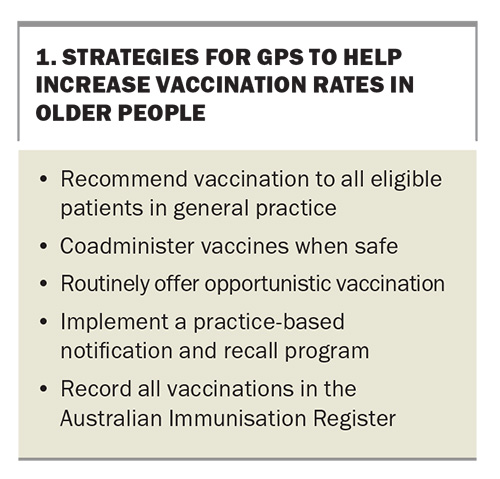
- Other strategies to help increase vaccination rates include:
– coadministration of vaccines
– opportunistic vaccination
– vaccination clinics
– patient notification and recall programs. - All vaccinations of older people must now be recorded in the Australian Immunisation Register.
Australia has not achieved acceptable vaccination rates in older people for vaccines listed on the National Immunisation Program (NIP). More can be done to achieve vaccine coverage comparable to that in children, of whom about 94% are fully vaccinated. Suggested strategies for GPs to help improve vaccination rates among older people are summarised in Box 1 and discussed in this article.
Recommend vaccination to all eligible patients
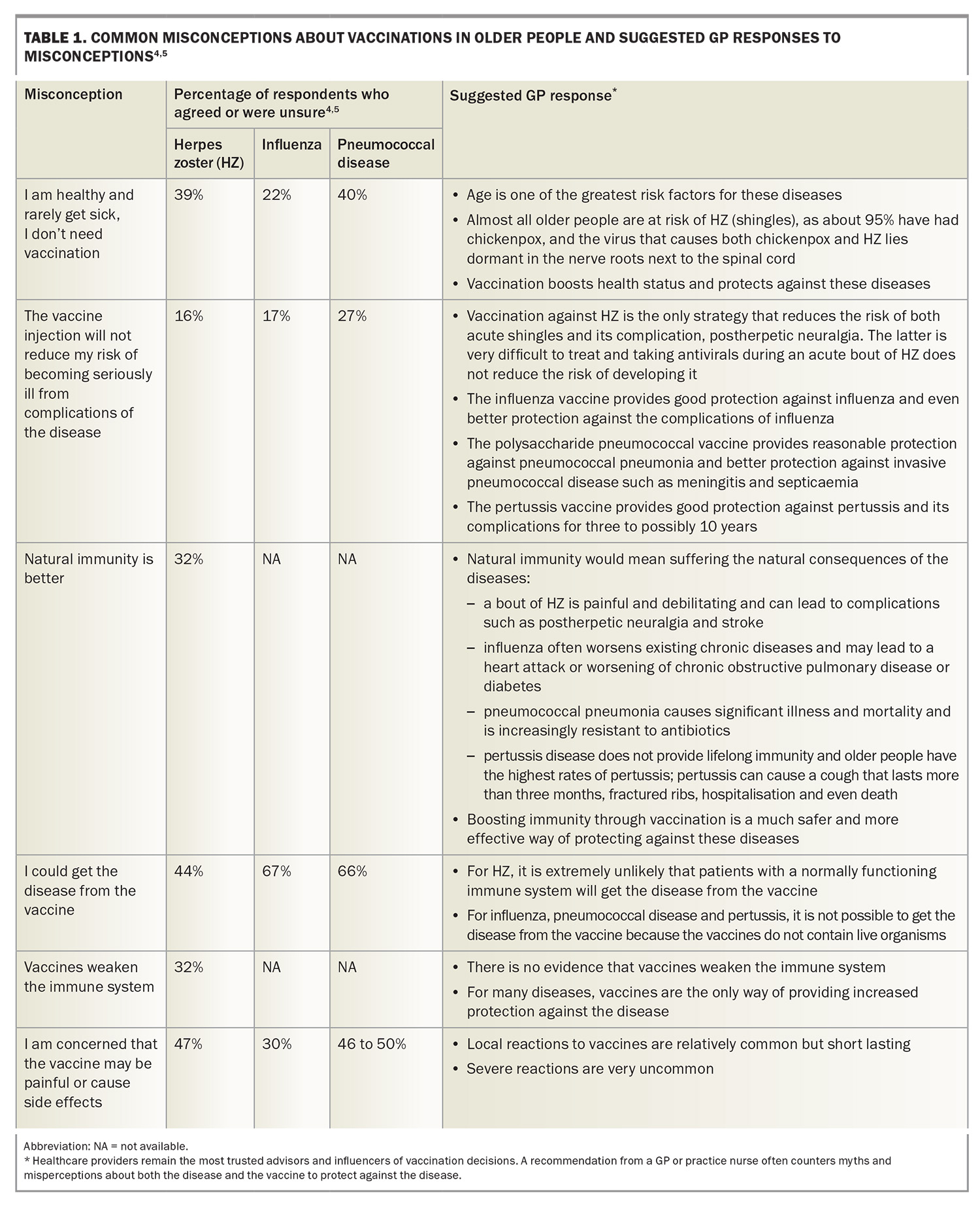
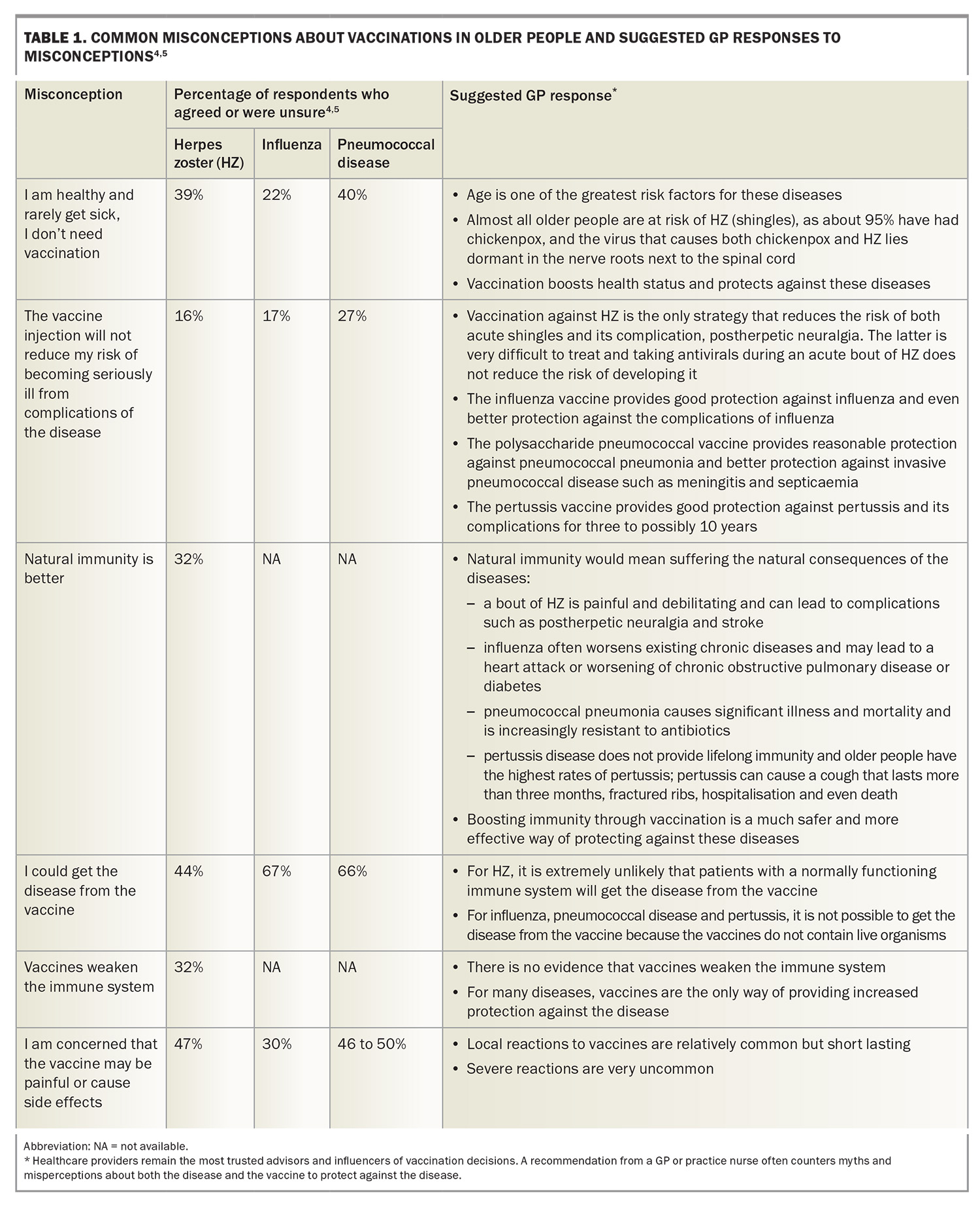
Studies show that the most influential driver of vaccination is a recommendation from the person’s healthcare provider. This can increase the likelihood of vaccination against influenza, pneumococcal disease and herpes zoster (HZ) 11-fold.1-5 However, patient surveys have found that myths and misconceptions about vaccines in older people are common (Table 1).4,5 These myths and misconceptions can act as barriers to vaccination and include the following beliefs:
- healthy people are not at risk of the disease targeted by the vaccine
- the disease is not serious
- the vaccine is ineffective or can itself cause the targeted disease
- natural immunity is better
- the risk of adverse effects is too high.
These misconceptions can be addressed by high-quality educational programs, ranging from one-on-one discussions through to societal-level campaigns.6 Both healthcare providers and patients need evidence-based information on the risks associated with the various vaccine-preventable diseases, the effectiveness and safety of the vaccines and ways of achieving high levels of vaccine coverage.
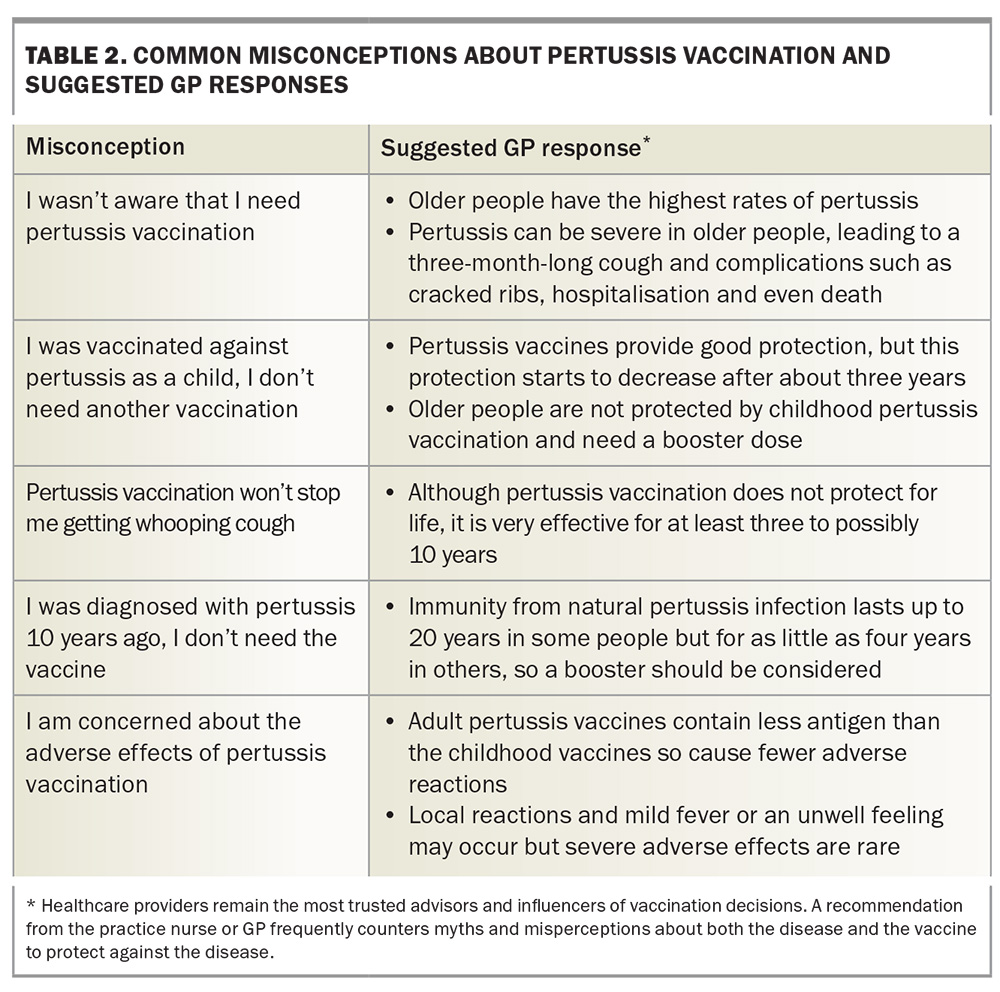
Some suggested GP responses to common patient misconceptions about vaccination are shown in Table 1 and Table 2. Tips for GPs on talking with patients about influenza, pneumococcal, HZ, pertussis, COVID-19 and RSV vaccination are shown in Box 2, Box 3, Box 4, Box 5, Box 6 and Box 7.
Other useful resources include the Australian Immunisation Handbook, National Centre for Immunisation Research and Surveillance fact sheets and the Australian and New Zealand Society for Geriatric Medicine position statement on Immunisation of Older People.7-9
Not on the National Immunisation Program does not mean ‘not needed’
All health professionals need to move beyond the mindset that the NIP is a comprehensive program to protect older people. It is based on other considerations, including economic, and while the GP should aim to administer all NIP-listed vaccines, there should be a discussion about the benefits of vaccines beyond the NIP.
A number of vaccines are recommended in the Australian Immunisation Handbook and by ATAGI but are not listed on the NIP. Several vaccines are registered on the TGA for age groups or indications beyond what is listed on the NIP. The shingles vaccine is registered from the age of 50 years, the inflection point beyond which the incidence of shingles greatly increases. RSV vaccines are registered from the age of 60 years, an inflection point beyond which the risks from hospitalisation with RSV greatly increase. Conjugate pneumococcal vaccines covering more or different serotypes are also now available. Meningococcus B and pertussis vaccinations are also not on the NIP for older people but can reduce the risk of these disabling and potentially fatal diseases in older people, particularly when local outbreaks occur.
Some vaccines, including COVID-19 vaccines, are funded but not on the NIP. Additionally, other funders, including the Department of Veterans Affairs, may fund vaccines that are not on the NIP for that patient.
The GP's role is to provide patients with expert health advice to allow the patient to decide which vaccines they wish to receive. Health practitioners often do not understand what drives patient preferences or the impact of the cost of an intervention; therefore, it should never be assumed that a vaccine is ‘too expensive’ for that patient or, conversely, that the patient can afford an unfunded vaccine.
Coadminister vaccines
A patient presenting for a particular vaccine, such as annual influenza vaccine, provides an opportunity to check current vaccination status and offer other vaccines. A pneumococcal vaccine can be given at the same time as the HZ vaccine (although they are best administered in different arms), and each of these can be given at the same time as an influenza vaccine. There is a rationale for coadministering influenza, COVID-19 and RSV vaccines each year; however, two adjuvanted vaccines (adjuvanted quadrivalent influenza and adjuvanted RSV vaccines) administered together may increase the risk of local and systemic adverse reactions. The safety and efficacy of administration of multiple vaccines given together has not been established for all combinations; however. this must be weighed against the risk of the patient not returning for a vaccine.
Support opportunistic vaccination
Other strategies that can help GPs increase vaccine coverage among older people in their practices include opportunistic vaccination and notification and reminder programs, which can act synergistically. Opportunistic vaccination captures the patient when they attend the practice; the vast majority of the older population visit a GP several times a year.4,10
A successful opportunistic vaccination program requires some planning. Suggested steps for GPs and practice staff to support opportunistic vaccination include the following.
- Display posters and leaflets about vaccinations for older people in the GP’s waiting and consulting rooms.
- Routinely inform eligible patients about each vaccine. A strategy is for the practice nurse to flag attending patients who are due for a vaccine in the appointment system after checking their vaccination status in the electronic record.
- Integrate vaccination into health assessments (e.g. ensure vaccination is part of the age 75 years health assessment).
- Administer the vaccine and document this in the patient’s electronic health record as well as the Australian Immunisation Register (AIR, see below).
- Give the patient information to take away that is relevant to their knowledge, interest and concerns or direct them to online patient information sites and personalise the information (e.g. www.ncirs.org.au/public, www.chop.edu/centers-programs/vaccine-education-center).
- Identify likely low-vaccination groups. Patients who attend the practice infrequently are less likely to receive recommended preventive care, such as vaccines. Reception staff can use the appointment system to generate a list of infrequent attenders (e.g. have not attended in the previous 12 to 18 months). This group could be sent an SMS or other electronic reminder suggesting they attend for vaccination.
- Implement standing orders to guide staff such as practice nurses to offer a range of vaccines after appropriate checks of eligibility and contraindications. Practice nurses could then administer the vaccine without the GP being present. Although this might mean patients are not billed, it will increase patient convenience and could be done in association with a GP appointment. For example, patients could see the practice nurse for vaccination while waiting to see the GP.
Occasionally, patients have strong views about vaccination and resist offers of vaccines. Although these views need to be respected, it is useful to understand the patient’s exact concerns and whether they might be amenable to further information. A strategy to help avoid giving offence when repeatedly offering a vaccine is to say ‘I understand your concerns about the […] vaccine and respect your decision. I find from time to time that patients change their mind, so raising the issue gives them an opportunity to discuss their wishes, address any concerns and possibly accept the vaccine if they wish’.
Implement notification and recall programs
Vaccination rates are likely to remain suboptimal, even with a planned opportunistic vaccination program, unless GPs also use a notification and recall strategy. This is particularly important for nonseasonal diseases, such as shingles. Suggested steps in a notification and recall/reminder program for GPs include the following.
- Appoint a co-ordinator. This increases the likelihood of teamwork, allocation of tasks and follow up of the impact.11,12
- Identify eligible patients. Practice software can be used to compile a list. GPs will need to determine whether they are the patient’s usual GP, for example by checking the patient’s electronic health record.
- Notify eligible patients about relevant vaccinations using one or more methods, ideally including an electronic strategy such as SMS messaging or an electronic reminder system. Examples of the latter include SmartVax (www.smartvax.com.au) and HotDoc (https:// hotdoc.com.au). A birthday card reminder is another way of prompting patients to attend for vaccination.
- Administer the vaccine and record the vaccination in the patient’s electronic record as well as the AIR. It can also be useful to give patients a small immunisation card that lists all the vaccines they have received. These cards are available from most state health departments and have the advantage of providing a portable summary of the individual’s vaccine history.
- Send ongoing recalls and reminders to any missed or new eligible patients at appropriate intervals. A tailored phone call or SMS from the practice nurse coupled with a strong GP recommendation will further increase coverage rates and potentially save the practice the time and cost of sending repeated letters.11 It is important to document reminders in the patient’s electronic health record. Sending reminders is made easier for some patient target groups if they are captured in the electronic practice register; it is worthwhile setting up disease and high-risk practice registers for some conditions.11
Australian Immunisation Register
The AIR was extended to all age groups from November 2016, replacing the Australian Childhood Immunisation Register.13 The AIR records vaccinations given through general practice and community clinics, including vaccines funded under the NIP and privately funded vaccinations. It provides a record of vaccinations of older people and makes this information available to other GPs and healthcare practitioners, for example if the patient moves to a new general practice.
The data could also be used, when sufficiently complete and reliable, to identify and target regions achieving lower vaccination rates, and to identify high vaccination regions that can be further interrogated to demonstrate best practices.
Conclusion
Despite official recommendations on vaccination in older people and inclusion of many vaccines on the NIP, coverage levels in older adults are well below those in children. Strategies that might increase uptake of recommended vaccines among older people include government actions, such as listing all recommended vaccines on the NIP and improving national surveillance of vaccination coverage levels and disease rates in the older population to inform funding discussions. However, GPs also have the opportunity to help increase vaccination rates among their older patients. Suggested strategies include educating their older patients about the risks and potential severity of vaccine-preventable diseases and the safety and effectiveness of vaccines, coadministration of vaccines where this is safe, and adopting systematic practice strategies to support opportunistic vaccination and patient notification and recall systems. MT
COMPETING INTERESTS: Professor Woodward has received funds for sitting on advisory boards and participating in educational events, for Seqirus, Sanofi, MSD, Pfizer, Moderna and GlaxoSmithKline. Associate Professor Litt has received funds for sitting on advisory boards for Seqirus and GlaxoSmithKline and speaker’s fees from Seqirus when providing educational updates on zoster vaccination for a range of healthcare providers. Professor Van Buynder has conducted clinical research on vaccine effectiveness of adjuvanted vaccines via an unrestricted grant from Novartis. He has also received support for research, education and marketing, travel and/or advisory board activities from Seqirus, Sanofi, GlaxoSmithKline, Roche, Pfizer and Novartis.
References
1. Damm O, Witte J, Greiner W. A systematic review of herpes zoster vaccine acceptance. Value Health 2015; 18: A592.
2. Task Force on Community Preventive Services. Recommendations to improve targeted vaccination coverage among high-risk adults. Am J Prev Med 2005; 28(5 Suppl): 231-237.
3. Mieczkowski T, Wilson S. Adult pneumococcal vaccination: a review of physician and patient barriers. Vaccine 2002; 20: 1383-1392.
4. Litt J, Rigby K, Duffy J. Australian National Influenza and Pneumococcal Survey in the elderly. Report No. 1. 12/2003 to Commonwealth Department of Health and Ageing. Adelaide: Discipline of General Practice, Flinders University; 2003. p. 199.
5. Litt J, Kim S, Woodman R, MacIntyre R, Cunningham A. Australian zoster study: GP and patient views about herpes zoster (shingles), its complications, and the likely acceptance of azoster vaccine (Zostavax). Int J Infect Dis 2014; 21(Suppl): 436-437.
6. Eiden AL, Barratt J, Nyaku MK. Drivers of and barriers to routine adult vaccination: a systematic literature review. Hum Vaccin Immunother 2022; 18: 2127290.
7. Australian Technical Advisory Group on Immunisation (ATAGI). Australian immunisation handbook. Canberra: Australian Government Department of Health; 2018. Available online at: https://immunisationhandbook.health.gov.au (accessed April 2024).
8. National Centre for Immunisation Research and Surveillance (NCIRS). NCIRS fact sheets, FAQs and other resources Sydney: NCIRS; 2024. Available online at: https://ncirs.org.au/resources (accessed April 2024).
9. Australian and New Zealand Society for Geriatric Medicine (ANZSGM). Position statement no. 7. Immunisation of older people - revision number 3, 2018. Sydney: ANZSGM; 2018. Available online at: www.anzsgm.org/posstate.asp (accessed February 2019).
10. Britt H, Miller GC, Charles J, et al. General practice activity in Australia 1990-00 to 2008-09: 10 year data tables. Canberra: Australian Institute of Health and Welfare; 2009.
11. Royal Australian College of General Practitioners. Putting prevention into practice. Guidelines for the implementation of prevention in the general practice setting. Melbourne: RACGP; 2018.
12. Thomas RE, Lorenzetti DL. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst Rev 2018; (5): CD005188.
13. Australian Government Department of Human Services. Australian Immunisation Register. Available online at: www.humanservices.gov.au/individuals/services/medicare/australian-immunisation-register (accessed February 2019).