High rate of antimicrobial resistance reported in paediatric bloodstream infections
By Melanie Hinze
Almost one in 10 children with a bloodstream infection are infected with a multidrug resistant (MDR) organism, new Australian research reveals. The research also highlighted key differences in the geographic distributions of bacteraemic pathogens across the country.
Key findings of the Australian Group on Antimicrobial Resistance (AGAR) Kids Report were published recently in Communicable Diseases Intelligence. The report evaluated 1679 isolates from 1611 patients aged younger than 18 years submitted by 38 institutions across Australia throughout 2020 and 2021. It found that overall 9.4% of the bacteria causing bloodstream infections were caused by MDR organisms.
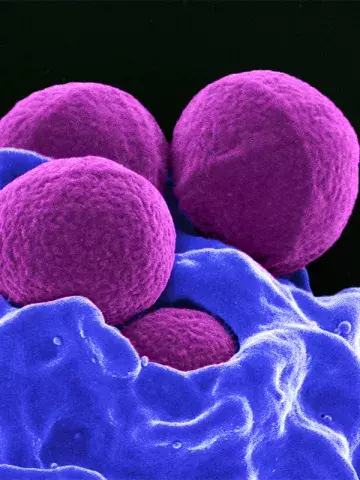
A total of 902 Gram-negative isolates were reported. These included 800 Enterobacterales isolates, 61 Pseudomonas aeruginosa and 41 Acinetobacter spp. Of the 777 Gram-positive isolates reported, 607 were Staphylococcus aureus and 170 were enterococci.
Nationwide, the Gram-negative Enterobacterales Escherichia coli was the most frequently reported bacteria in patients under 1 year of age, with the highest proportion of antibiotic resistance found in Victoria.
Staphylococcus aureus was the most common bacteria found in children over the age of 1 year. The Northern Territory recorded the highest rate of methicillin-resistance S. aureus (MRSA) at 45%, followed by Western Australia at 19%. Overall, 12.9% of S. aureus isolates were methicillin resistant, and 5.6% of isolates were MDR.
Ms Anita Williams, lead author of the article and Research Officer, Infectious Diseases Epidemiology at The Kids Research Institute Australia, Perth, said the data were reported from all eight paediatric tertiary hospitals in the country, and 25 of the 29 principal referral hospitals. This included 20 of the 26 accredited level III neonatal intensive care units, all accredited paediatric intensive care units, and all haematology, oncology and transplant centres.
‘This means that the results of this study are generally representative of antimicrobial resistance in children nationwide,’ she said.
Additionally, seven out of 10 infections were community onset, meaning patients presenting to GPs were exposed to the same bacteria with the same resistance profiles as those studied.
Tasmania had the highest rate of community onset episodes (85% of all episodes), whereas Victoria had the lowest rate (58% of episodes).
‘This paper demonstrates that all children in Australia are at risk of antimicrobial resistant infections,’ Ms Williams said.
Ms Williams told Medicine Today that AGAR reports would be published regularly to track antimicrobial resistance in Australian children, to investigate the differences in proportions of antimicrobial resistance between adults and children, and to assess the geographic distribution of antimicrobial resistance in children across Australia at a more localised level.
‘These reports will provide crucial evidence for all clinicians, including those managing neonates and children, to tackle the challenge of antimicrobial resistance in Australia,’ she added.
Commun Dis Intell 2024; 48: https://doi.org/10.33321/ cdi.2024.48.32.