Buruli ulcer: consensus statement highlights need for increased awareness
By Melanie Hinze
A new consensus statement, endorsed by the Australasian Society for Infectious Diseases and published in the Medical Journal of Australia, highlights the increasing incidence of Buruli ulcer in Australia, and provides updates for diagnostic and treatment recommendation for clinicians.
With the incidence of Buruli ulcer increasing across Australia, and its presence in previously nonendemic areas, the statement authors have called for this disease to be made nationally notifiable.
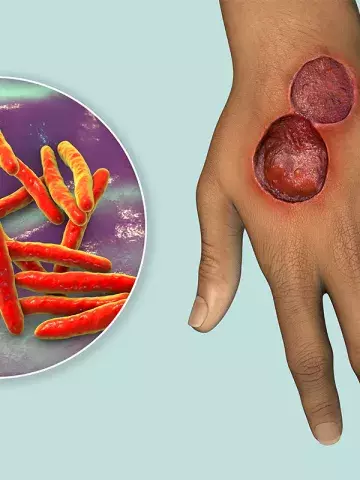
Previously, outbreaks of Buruli ulcer, which is caused by Mycobacterium ulcerans, have largely been localised to coastal regions in Victoria and north Queensland, but transmission has now been reported in suburbs of Melbourne and in Bateman’s Bay in New South Wales. In 2023, Victoria reported 362 cases, the highest annual count recorded to date, the statement notes.
Senior author, Dr Stephen Muhi, Infectious Diseases Specialist at the Royal Melbourne Hospital and Senior Research Fellow at the Peter Doherty Institute for Infection and Immunity, Melbourne, told Medicine Today that diagnostic best practice incorporated early identification of the ulcer, which usually started as a painless nodule or plaque that progressed to ulcers with undermined edges. A swab of the ulcer’s undermined edge or a biopsy of a nonulcerated lesion sent for PCR testing remained the gold standard, he said.
The statement authors noted that incorrectly performed swabs or swabs of nonulcerated skin can give a false-negative result.
Eight weeks’ treatment with rifampicin-based dual antibiotic therapy, in combination with clarithromycin or a fluoro-quinolone, remained the preferred treatment, or six weeks for small uncomplicated lesions, or four weeks post-surgery, they said.
The authors stressed the importance of patient education, as lesions could enlarge with treatment and took an average of four to five months to heal, well after the antibiotic course had been completed.
They also noted that children comprised about 10% of cases and had higher rates of severe or nonulcerative disease and an increased risk of paradoxical reactions.
In addition, First Nations Australians may face diagnostic delays and limited access to specialist care, particularly in remote regions, the authors wrote.
Dr Muhi said the emergence of Buruli ulcer in new areas highlighted the importance of raising awareness of this disease.
‘We hope this [consensus statement] offers frontline clinicians an overview of the management of Buruli ulcer,’ he said. ‘We also hope it offers useful guidance, drawn from contemporary evidence and the experience of the authors.’
Med J Aust 2025; doi: 10.5694/ mja2.52591 (https://www.mja.com.au/journal/2025/222/11/management-mycobacterium-ulcerans-infection-buruli-ulcer-australia-consensus).