Omg, Omicron! Why it's too soon to panic about COVID vaccines and the new variant
Researchers around the world are trying to work out whether existing COVID vaccines protect us from the latest variant, Omicron.
The worst-case scenario is the virus has mutated so much in the crucial parts of its genome that it can escape COVID vaccines designed to protect us from earlier versions of the virus – with devastating consequences globally.
.@WHO Technical Lead on Covid-19 @mvankerkhove lays out what you need to know about Omicron: “We’ll get some information on transmissibility and severity in the coming days,” she says, though it’ll take 2-4 weeks for preliminary information on the impact of vaccines on Omicron. pic.twitter.com/H48JLsOEkI
— Christiane Amanpour (@amanpour) November 29, 2021
But it’s too soon to panic. And vaccines may end up protecting us against Omicron after all, as they have done with earlier variants.
The World Health Organization (WHO) says it will take us another two to four weeks to figure out what’s going on. Here’s what scientists around the world are racing to find out.
Read more: Not again ... how to protect your mental health in the face of uncertainty and another COVID variant
Why the concern?
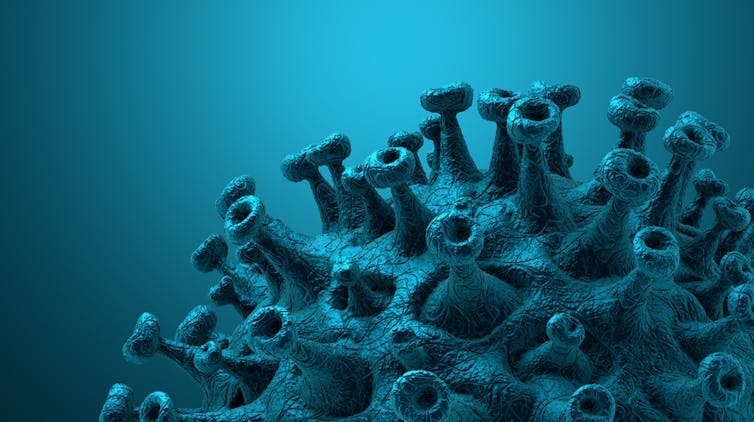
The reason Omicron has caused global alarm is due to the number of new mutations throughout the genome of SARS-CoV-2, the virus that causes COVID.
This data, coupled with real world data on the rapid rise in Omicron cases in South Africa, prompted the WHO to designate Omicron a 'variant of concern' on November 26.
Omicron has now been detected in several other countries around the world.
The Omicron COVID-19 variant is now classified as a ’variant of concern’ (VOC). While data on the Omicron is limited, here’s what we know about this variant so far. https://t.co/UpwcQH58Kj
— Healthline (@Healthline) December 1, 2021
We’ve already seen some Omicron mutations in other variants.
Individually, some of these mutations have been associated with resistance to neutralising antibodies. In other words, these mutations help the virus evade recognition by an immune system primed with a COVID-19 vaccine.
Some of these individual mutations have also been linked with increased transmissibility of the virus from one person to another.
However, Omicron has many unique mutations. For instance, on the spike protein, the protein used in many current vaccines, Omicron has about 30 mutations compared with the virus that came out of Wuhan. Delta has only ten mutations in its spike protein. So you get an idea of the scale of change.
Read more: Omicron: why the WHO designated it a variant of concern
Investigating the way these multiple mutations interact with one another, rather than individually, will be key to understanding how Omicron behaves compared with other variants.
Looking at these interactions will tell us more about Omicron’s ability to infect cells, cause disease and escape vaccines. And experiments are under way to investigate these mutations and their impacts.
While we wait for the results, we heard this week from some of the vaccine manufacturers. Moderna said its vaccine would be less effective against Omicron than against Delta. Meanwhile, Pfizer/BioNTech said its vaccine would still protect against severe disease. Both companies said they could produce tweaked booster vaccines, if needed.
European stock markets have fallen after the boss of Moderna cast doubts on the effectiveness of vaccines against the new Omicron Covid variant.
— Capital Moments (@CapitalMoments) November 30, 2021
Stephane Bancel told the Financial Times he thought there would be a "material drop" in vaccine efficacy. pic.twitter.com/40rbnKb8ms
Why will it take weeks to get answers?
Here’s what researchers around the world are working on and why we won’t have answers for a few weeks.
Growing the virus
Researchers are taking samples of Omicron from infected people and growing the virus in laboratories. This gives them working stocks of the virus to conduct experiments. This can take time as you’re often starting with tiny amounts of virus from a swab.
This process also relies on access to the right types of cells to grow the virus in.
Finally, this needs to be done in laboratories that offer a high level of biosafety, to contain the virus. Not all researchers have access to these facilities.
Make your own ‘virus’
Researchers can also use genetic tools to produce the virus in the laboratory, requiring only the genome sequence of SARS-CoV-2 to begin production. This removes the reliance on patient samples.
They can also produce genetically engineered viruses, called pseudotyped viruses, in the laboratory. These carry only the spike protein of SARS-CoV-2.
Researchers can also express small portions of the spike protein on the surface of other organisms, such as yeast.
All of these options take time to set up, optimise and be used in the types of studies outlined below.
Both methods are useful
Initial studies will look at how Omicron’s mutations impact the fitness of the variant – its transmissibility and ability to evade vaccine-induced immunity.
For instance, initial experiments will look at Omicron’s ability to infect cells. These studies will tell us how well Omicron’s spike protein interacts with the ACE2 receptor, the gateway to infecting our cells. Further studies will investigate how well Omicron can replicate in cells after gaining entry.
Neutralisation studies will investigate how well antibodies – induced by current SARS-CoV-2 vaccines – can neutralise Omicron, or prevent it from infecting cells. Such studies rely on access to serum from vaccinated people and are likely to compare the neutralising capacity of Omicron against other SARS-CoV-2 variants.
More of the same. but central message; patience. Data is not as bad as could have been, in a few weeks there will be enough to know:
— Marc Veldhoen (@Marc_Veld) November 27, 2021
- infectiousness
- pathogenicity
- evasion of neutralising antibodies.https://t.co/YPqYLMLCxm
Studies are also likely to investigate the effect of vaccine booster regimes and earlier SARS-CoV-2 infection on how well antibodies neutralise Omicron.
So what can we expect? Until we get the results of these experiments, it’s difficult to say for certain.
Studies of how effective COVID-19 vaccines are against other variants show they are generally less able to induce the type of antibody response we’d like to see (neutralising antibodies). However, when previous variants have emerged, vaccines have continued to protect against severe disease.
Vaccine protection is not all or nothing. We are unlikely to get a perfect neutralising antibody response against Omicron, or no response, rather something in between.
Read more: How well do COVID vaccines work in the real world?
We'll also know more as we see more cases
Continued monitoring of real-world data will also be essential to determine how Omicron impacts the broader pandemic.
Whether Omicron is able to spread from seeding events around the world or compete with Delta are questions to be answered in the coming weeks.
Whether infection with Omicron causes less or more serious disease also remains unclear. Monitoring hospitalisation rates will be key here.
We still need to tackle Delta
Currently fewer than 200 genetic sequences of Omicron have been compiled compared with more than 2.8 million Delta sequences. Delta remains the most dominant variant. So we should continue to use vaccines and therapies we know work against Delta.
It’s also essential we continue with public health measures, such as wearing masks and social distancing, alongside continued vaccination, to combat the spread of SARS-CoV-2 and the emergence of further variants.
Read more: Wealthy nations starved the developing world of vaccines. Omicron shows the cost of this greed
This article is republished from The Conversation under a Creative Commons license. Read the original article, published on December 2, 2021.
Disclosure statement
Adam Taylor receives funding from the Australian National Health and Medical Research Council.
![]()

