Cerebral aneurysms and subarachnoid haemorrhage: avoiding the diagnostic pitfalls
Patients with atypical or mild symptoms of subarachnoid haemorrhage due to a ruptured cerebral aneurysm are more difficult to diagnose than patients who present with typical symptoms of sudden severe headache and associated symptoms. Patients without typical symptoms are more likely to have low volume haemorrhages that may not be seen on a CT scan.
- Subarachnoid haemorrhage (SAH) due to a ruptured cerebral aneurysm is a potentially fatal condition that often presents as headache.
- A raised index of suspicion must exist for all patients with sudden, severe headache with or without associated symptoms.
- Initial investigation of suspected SAH should be a noncontrast CT scan; most haemorrhages will be apparent on this test.
- Management of SAH is increasingly becoming endovascular.
- The outcome for patients with no or only a mild global or focal neurological deficit on presentation has improved, but prehospital mortality and disability from the initial haemorrhage remains a significant problem.
- Unruptured asymptomatic aneurysms are not an urgent scenario and can be dealt with in consultative outpatient fashion.
Picture credit: © KO Studios
Headache, a common presentation to primary care physicians, usually has a benign cause and course but can occasionally be a symptom of a neurological condition requiring urgent neurosurgical treatment. Secondary headache (headache due to an underlying pathological cause, including structural, vascular, infective, inflammatory or drug-induced) therefore always needs to be considered in patients with new, severe or persistent headache or atypical presentations of headache.1,2
Patients presenting with sudden severe ‘thunderclap’ headache, with or without associated symptoms (which may include nausea and vomiting, loss of consciousness and a focal or global neurological deficit) clearly need immediate investigation with brain CT for probable subarachnoid haemorrhage (SAH) due to a ruptured cerebral aneurysm. However, patients with atypical or mild symptoms of SAH are more difficult to diagnose; these are often the patients with low volume haemorrhages that may not be seen on a CT scan. Further investigations are required in these patients to exclude SAH as the aetiology. As some of these investigations are invasive and involve risk (e.g. lumbar puncture and digital subtraction angiography), significant decisions and recommendations have to be made in patients who often have the mildest headache.2-5
Ruptured cerebral aneurysms have a significantly different natural history to unruptured aneurysms. The re-rupture rate in the first two weeks after haemorrhage is 20% (with mortality of 10%), and in the first six months is 50%.6,7 The annual rupture rate of a small (less than 10 mm) unruptured aneurysm is in the order of 1% per year or less.8
There are, of course, structural causes of headache and nontraumatic SAH other than a ruptured cerebral aneurysm, and these are generally discovered on further investigation.9,10 The critical issue is the diagnosis of the haemorrhage itself as a missed haemorrhage can have devastating effects for the patient.11
The investigation and management options for patients with SAH due to a ruptured cerebral aneurysm are discussed in this article, and a case study of a low volume haemorrhage is presented to demonstrate some of the difficulties and complexities surrounding diagnosis (Box and Figures 1a and b). The presentation and management of unruptured cerebral aneurysms is also discussed.
Investigations for SAH
CT scan
A noncontrast CT scan of the brain is the best and most widely available test for the investigation of severe headache.2 It is the most sensitive imaging modality for detecting blood, and will reveal blood in over 95% of patients with SAH, although the sensitivity decreases over time (sensitivity is 98 to 100% in the first 12 hours after SAH, reducing to 93% at 24 hours and to between 57 and 85% six days after SAH).2,12,13
Lumbar puncture
Lumbar puncture is the test required to exclude SAH when CT imaging is unhelpful.2,14 It is best performed more than 12 hours after SAH.15
The results of lumbar puncture can be confounded by ‘traumatic taps’, where the cerebrospinal fluid (CSF) is stained by blood contamination during puncture.16,17 Traditionally there should be clearing of the blood staining if it is traumatic, and consistency over tube collection if SAH is present.16,17 Other methods to differentiate SAH and contaminated collection are examination on spectrophotometry of the supernatant from centrifuged CSF samples (presence of xanthocromia indicating SAH) and laboratory assessment of CSF samples for extracellular blood products such as bilirubin (detection of bilirubin indicating SAH).15,16
The majority of patients with suspected SAH appear to have ‘traumatic taps’.17 Needless to say a clear result is comforting and as definitive as possible in the acute period after possible haemorrhage.16 CSF samples that are heavily contaminated with blood will often be problematic despite the above considerations.
CT angiography
CT angiography (CTA) is often used as an adjunct to CT and lumbar puncture, and can be a powerful tool for the noninvasive assessment of anomalies in the larger vessels of the circle of Willis.18,19 However, this assessment of vascular anatomy does not exclude that there has been haemorrhage.
The sensitivity of CTA is less than that of digital subtraction angiography.18,19
MRI and magnetic resonance angiography
MRI is less sensitive than CT at finding acute haemorrhage and therefore is not recommended as a primary screening modality patients with suspected SAH.20,21 Magnetic resonance angiography (MRA) also, in general, has somewhat less anatomical resolution than CTA, although new techniques for optimising images and defining pathology are promising.22
Digital subtraction angiography
Digital subtraction angiography (DSA) is the gold standard to assess vascular anatomy but has restricted availability and an attendant risk as it is an invasive test.2 It is uncommonly used to investigate patients with SAH, unless haemorrhage or vessel anomaly is seen on noninvasive tests.
Nonhaemorrhagic presentation of cerebral aneurysms
Incidental finding
Most aneurysms are discovered incidentally in an outpatient setting. Increased access to noninvasive, relatively accurate imaging such as CTA and MRA has meant that the volume of incidental findings of cerebral aneurysm, which has a community prevalence of about 2%, is significant.23,24
Several multicentre and prospective trials have attempted to determine the natural history of cerebral aneurysms and the morbidity of therapy.8,25-29 Unfortunately, the heterogeneity of aneurysms in terms of size, morphology and site, along with the moving target of microsurgical and endovascular morbidity, conspires to cloud risk–benefit analysis for repair.30
In general terms, the larger the aneurysm, the greater the risk of haemorrhage.8,27 Certain sites, such as the posterior circulation and the posterior communicating artery (which is part of the circle of Willis), appear to have increased haemorrhage risk independent of the size of the aneurysm.8,27 Aneurysms with unfavourable morphology, such as daughter sacs, are also thought to be higher risk.27 It is generally agreed that the haemorrhage rate for small (less than 7 mm) aneurysms with no unfavourable features is less than 1% annually.8,27 Giant aneurysms (greater than 25 mm) have an adverse event rate of more than 2% annually.8,27,31
Mass effect
Mass effect generally relates to large aneurysms or those in specific sites.32 Large or giant aneurysms may have a mass effect on neural structures, causing focal or global neurological deficits or seizures.32,33 Standard imaging will usually make this diagnosis, although other lesions may be mimicked – for example, thrombosis of an aneurysm can lead to acute swelling and embolus that may mimic a brain tumour on imaging.34
Sites notorious for nerve deficit even with small or medium aneurysms are the posterior communicating artery, affecting the third cranial nerve (oculomotor nerve), and the anterior communicating artery, affecting the second cranial nerve (optic nerve) or chiasm.35 Compression of these or other nerves can cause acute or chronic deficit.
Acute cranial neuropathies related to aneurysms are an emergency in that they indicate a change in the aneurysm, which signals an increase in risk of haemorrhage.36 Differentiation of aneurysmal compression and diabetic mononeuropathy can be problematic (e.g. pupil involvement in aneurysmal compression), and is a classic pitfall.37
Therapy and outcome
Outcome following SAH due to a ruptured cerebral aneurysm remains concerning despite advances in therapy.2 A rough guide is that after SAH, one-third of patients will be treated and recover ‘back to normal’, one-third will survive and be disabled, and one-third will not survive.2 Prehospital mortality is up to 15%, which is probably an underestimation as many causes of sudden death in the elderly may go uninvestigated.38
The immediate treatment of patients presenting with haemorrhage involves basic resuscitation in poor grade patients (i.e. patients with a global or focal neurological deficit).39 A significant cause of ongoing coma following a SAH is hydrocephalus relating to the blood in the subarachnoid space. A patient with a decreased level of consciousness following a haemorrhage is not considered optimised until this pressure is relieved with external ventricular drainage. As an extension of this, no patient should be considered unsalvageable on the grounds of clinical condition without CSF diversion.40,41 Careful control of the patient’s blood pressure (by medication) is vital initially to decrease the risk of rebleeding.39
Securing of the aneurysm by the most appropriate means should be achieved at the earliest opportunity, when the multidisciplinary team required can be assembled.42 The patient’s current use of anticoagulant and antiplatelet medication has to be dealt with as effectively as possible with the administration of procoagulants, blood products and platelets as appropriate. The presence of irreversible or significant bleeding diathesis may be a relative indication for endovascular treatment (i.e. coiling) rather than microvascular treatment (i.e. clipping).
Vasospasm is a significant complication of SAH and typically has onset five to 10 days after the bleeding event.43 Treatment of vasospasm includes pharmacotherapy with nimodipine and induction of hypertension and hypervolaemia, to increase cerebral blood flow.44,45 Endovascular angioplasty (chemical and balloon) is being used increasingly to manage this problem, with great benefit.45,46 A typical stay in an intensive care or high dependency unit of a patient with vasospasm can be more than two weeks due to the intensity of this therapy.
Patients with unruptured aneurysms that are being repaired microsurgically require the same presurgical assessment and management of antiplatelet or anticoagulant therapy as those undergoing any other major craniotomy. In those undergoing elective coiling, there is often no need to stop antiplatelet medication, and in those requiring complex repairs and/or stents, preloading with significant antiplatelet medication prior to the procedure is often appropriate.47
Endovascular therapy
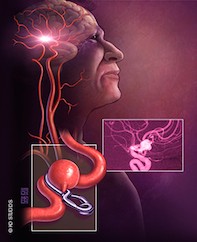
The greatest change in the care of patients with this condition in recent times is the emergence of endovascular therapy as the dominant modality for treating ruptured cerebral aneurysms (Figure 2).29 The use of different embolic material and coils, along with stents and technical tricks of repair such as balloon-assisted coiling, have rapidly changed the deployment of endovascular therapy.48
Dedicated neurointerventional radiologists are now working in large centres and repairing the majority of ruptured aneurysms.48
Microvascular repair
Microvascular repair (surgical aneurysm clipping) remains an important modality for lesions unfavourable for endovascular intervention.29,49 Unsuitability for coil repair often relates to the ratio of the fundus to the neck of the lesion in locations where the use of stent or balloon assistance for the coiling may be inappropriate or unsafe.49 The most common location where coiling is not favoured is the middle cerebral artery bifurcation.94
Repair of a ruptured carotid bifurcation aneurysm is discussed in the case study (Box and Figures 1a and b).
Open surgery
Open surgery may also be used where there are associated surgical benefits, such as removal of intracerebral clot.2
Treatments compared
In general, endovascular therapy has lower upfront risk than other treatments, and is without the associated morbidity of craniotomy (brain retraction, wound, access risk).29 It does, however, have less durability overall, and also a greater possibility of persistent/recurrent aneurysm necks (filling of the aneurysm where it pouches out from the vessel wall), which present an ongoing risk of haemorrhage, although the magnitude of that risk overall and in the previously ruptured versus the unruptured cohort is not well known.28,50 Securely coiled aneurysms that are stable after two years rarely re-rupture.50
A relevant factor in stent-assisted repair of aneurysm is that the patient usually requires indefinite antiplatelet therapy.51 This and issues of durability will become more clear as our longitudinal experience with this therapy improves with time.
The ideal therapeutic scenario is where a balance and good working relationship exists between neuroradiologists and neurosurgeons. Care decisions should not be based on treatment availability in a condition such as this, and collaboration is vital; however, access limitations to endovascular care can influence intervention decisions.49 There are frequent occasions where both coiling and clipping may be applied, either as planned adjuvants or in cases of failure of one or other.
In the presented case study, the anatomy of the aneurysm was such that simple coiling was not possible and stenting/coiling was thought to be higher risk than microsurgical repair.
Conclusion
Cerebral aneurysms remain a diagnostic and therapeutic challenge. Although SAH can be excluded in most patients with headache by simple history taking, in those where doubt remains (e.g. when the haemorrhage is low volume and does not show on CT imaging) the consequences of failure to diagnose need to be weighed against the inconvenience and possible morbidity of further investigation.
When an aneurysm has been diagnosed, the decision to treat and the mode of treatment to use has become multidisciplinary in a way analogous to that in many other medical conditions. This has led to better outcomes and the emergence of specialised neurovascular centres. MT
References
- Edlow JA, Caplan LR. Avoiding pitfalls in the diagnosis of subarachnoid hemorrhage. N Engl J Med 2000; 342: 29-36.
- Bederson JB, Connolly ES Jr, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 2009; 40: 994-1025.
- Eggers C, Liu W, Brinker G, Fink GR, Burghaus L. Do negative CCT and CSF findings exclude a subarachnoid haemorrhage? A retrospective analysis of 220 patients with subarachnoid haemorrhage. Eur J Neurol 2011; 18: 300-305.
- Ditta M, Galea J, Holland J, Patel HC. Lumbar puncture and the diagnosis of CT negative subarachnoid haemorrhage: time for a new approach? Br J Neurosurg 2013; 27: 599-602.
- Edlow JA, Panagos PD, Godwin SA, Thomas TL, Decker WW; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2008; 52: 407-436.
- Tang C, Zhang TS, Zhou LF. Risk factors for rebleeding of aneurysmal subarachnoid hemorrhage: a meta-analysis. PLoS One 2014; 9: e99536.
- Jane JA, Winn HR, Richardson AE. The natural history of intracranial aneurysms: rebleeding rates during the acute and long term period and implication for surgical management. Clin Neurosurg 1977; 24: 176-184.
- Wiebers DO, Whisnant JP, Huston J 3rd, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003; 362: 103-110.
- Torelli P, Campana V, Cervellin G, Manzoni GC. Management of primary headaches in adult emergency departments: a literature review, the Parma ED experience and a therapy flow chart proposal. Neurol Sci 2010; 31: 545-553.
- Landtblom AM, Fridriksson S, Boivie J, Hillman J, Johansson G, Johansson I. Sudden onset headache: a prospective study of features, incidence and causes. Cephalalgia 2002; 22: 354-360.
- Neil-Dwyer G, Lang D. ‘Brain attack’ – aneurysmal subarachnoid haemorrhage: death due to delayed diagnosis. J R Coll Physicians Lond 1997; 31: 49-52.
- Byyny RL, Mower WR, Shum N, Gabayan GZ, Fang S, Baraff LJ. Sensitivity of noncontrast cranial computed tomography for the emergency department diagnosis of subarachnoid hemorrhage. Ann Emerg Med 2008; 51: 697-703.
- Perry JJ, Stiell IG, Sivilotti ML, et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ 2011; 343: d4277.
- Stewart H, Reuben A, McDonald J. LP or not LP, that is the question: gold standard or unnecessary procedure in subarachnoid haemorrhage? Emerg Med J 2014; 31: 720-723.
- Cruickshank A, Auld P, Beetham R, et al. Revised national guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage. Ann Clin Biochem 2008; 45: 238-244.
- Gorchynski J, Oman J, Newton T. Interpretation of traumatic lumbar punctures in the setting of possible subarachnoid hemorrhage: who can be safely discharged? Cal J Emerg Med 2007; 8: 3-7.
- Shah KH, Edlow JA. Distinguishing traumatic lumbar puncture from true subarachnoid hemorrhage. J Emerg Med 2002; 23: 67-74.
- Velthuis BK, Van Leeuwen MS, Witkamp TD, Ramos LM, Berkelbach van Der Sprenkel JW, Rinkel GJ. Computerized tomography angiography in patients with subarachnoid hemorrhage: from aneurysm detection to treatment without conventional angiography. J Neurosurg 1999; 91: 761-767.
- Wintermark M, Uske A, Chalaron M, et al. Multislice computerized tomography angiography in the evaluation of intracranial aneurysms: a comparison with intraarterial digital subtraction angiography. J Neurosurg 2003; 98: 828-836.
- Mitchell P, Wilkinson ID, Hoggard N, et al. Detection of subarachnoid haemorrhage with magnetic resonance imaging. J Neurol Neurosurg Psychiatry 2001; 70: 205-211.
- Schellinger PD, Fiebach J, Mohr A, et al. [Value of MRI in intracerebral and subarachnoid hemorrhage]. Der Nervenarzt 2001; 72: 907-917.
- Chang W, Huang M, Chien A. Emerging techniques for evaluation of the hemodynamics of intracranial vascular pathology. Neuroradiol J 2015; 28: 19-27.
- Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 2011; 10: 626-636.
- Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke 1998; 29: 251-256.
- White PM, Wardlaw JM. Unruptured intracranial aneurysms. J Neuroradiol 2003; 30: 336-350.
- Rinkel GJ. Natural history, epidemiology and screening of unruptured intracranial aneurysms. J Neuroradiol 2008; 35: 99-103.
- Morita A, Kirino T, Hashi K, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 2012; 366: 2474-2482.
- Spetzler RF, McDougall CG, Zabramski JM, et al. The Barrow Ruptured Aneurysm Trial: 6-year results. J Neurosurg 2015; 123: 609-617.
- Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet 2015; 385: 691-697.
- Ajiboye N, Chalouhi N, Starke RM, Zanaty M, Bell R. Unruptured cerebral aneurysms: evaluation and management. ScientificWorldJournal 2015; 2015: 954954.
- International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms – risk of rupture and risks of surgical intervention. N Engl J Med 1998; 339: 1725-1733.
- Deruty R, Pelissou-Guyotat I, Mottolese C, Amat D. Management of unruptured cerebral aneurysms. Neurol Res 1996; 18: 39-44.
- Patil A, Menon GR, Nair S. Unruptured anterior communicating artery aneurysms presenting with seizure: report of three cases and review of literature. Asian J Neurosurg 2013; 8: 164.
- Kim YJ, Jeun SS, Park JH. Thrombosed large middle cerebral artery aneurysm mimicking an intra-axial brain tumor: case report and review of literature. Brain Tumor Res Treat 2015; 3: 39-43.
- de Oliveira JG, Borba LA, Rassi-Neto A, et al. Intracranial aneurysms presenting with mass effect over the anterior optic pathways: neurosurgical management and outcomes. Neurosurg Focus 2009; 26: E3.
- Keedy A. An overview of intracranial aneurysms. Mcgill J Med 2006;
- 9: 141-146.
- Jacobson DM. Pupil involvement in patients with diabetes-associated oculomotor nerve palsy. Arch Ophthalmol 1998; 116: 723-727.
- Schievink WI, Wijdicks EF, Parisi JE, Piepgras DG, Whisnant JP. Sudden
- death from aneurysmal subarachnoid hemorrhage. Neurology 1995; 45:
- 871-874.
- Bederson JB, Connolly ES Jr, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 2009; 40: 994-1025.
- Germanwala AV, Huang J, Tamargo RJ. Hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am 2010; 21: 263-270.
- Rajshekhar V, Harbaugh RE. Results of routine ventriculostomy with external ventricular drainage for acute hydrocephalus following subarachnoid haemorrhage. Acta Neurochir 1992; 115: 8-14.
- Laidlaw JD, Siu KH. Ultra-early surgery for aneurysmal subarachnoid hemorrhage: outcomes for a consecutive series of 391 patients not selected by grade or age. J Neurosurg 2002; 9: 250-258; discussion 47-49.
- Mills JN, Mehta V, Russin J, Amar AP, Rajamohan A, Mack WJ. Advanced imaging modalities in the detection of cerebral vasospasm. Neurol Res Intern 2013; 2013: 415960.
- Pickard JD, Murray GD, Illingworth R, et al. Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. BMJ 1989; 298: 636-642.
- Velat GJ, Kimball MM, Mocco JD, Hoh BL. Vasospasm after aneurysmal subarachnoid hemorrhage: review of randomized controlled trials and meta-analyses in the literature. World Neurosurg 2011; 76: 446-454.
- Hoh BL, Ogilvy CS. Endovascular treatment of cerebral vasospasm: transluminal balloon angioplasty, intra-arterial papaverine, and intra-arterial nicardipine. Neurosurg Clin N Am 2005; 16: 501-516.
- Rahme RJ, Zammar SG, El Ahmadieh TY, El Tecle NE, Ansari SA, Bendok BR. The role of antiplatelet therapy in aneurysm coiling. Neurol Res 2014; 36: 383-388.
- Joseph S, Kamble R. Current trends in endovascular management of intracranial aneurysms (including posterior fossa aneurysms and multiple aneurysms). Indian J Radiol Imaging 2008; 18: 256-263.
- Darsaut TE, Kotowski M, Raymond J. How to choose clipping versus coiling in treating intracranial aneurysms. Neurochirurgie 2012; 58: 61-75.
- Pyysalo LM, Keski-Nisula LH, Niskakangas TT, Kahara VJ, Ohman JE. Long-term follow-up study of endovascularly treated intracranial aneurysms. Interv Neuroradiol 2010; 16: 361-368.
- Geyik S, Yavuz K, Yurttutan N, Saatci I, Cekirge HS. Stent-assisted coiling in endovascular treatment of 500 consecutive cerebral aneurysms with long-term follow-up. AJNR Am J Neuroradiol 2013; 34: 2157-2162.