Headache: investigating the cause

Headaches are a frequent presenting complaint in primary care settings. Diagnoses are primarily clinical, with some specific indications for further investigation. This article provides specialist advice and allows GPs to review their existing knowledge and expertise on this common presentation.
- Most patients presenting with chronic or recurrent headache will have one of the primary headache disorders; therefore, investigations are unlikely to be abnormal.
- GPs will be familiar with the usual presentation of the common primary headaches. These headaches can often be diagnosed without further investigation.
- Headaches occurring with new, abrupt onset or with relentless progression are likely to be caused by specific pathology and patients should be referred for appropriate testing and treatment.
- In most cases requiring brain imaging, MRI is preferable over CT. GPs should consider the practical difficulties for patients with regards to cost, access and availability.
- The mnemonic ‘SNOOP-4’ (systemic, neurological, onset [sudden or after 50 years of age], pattern change, precipitated by valsalva manoeuvre, postural aggravation, papilloedema) is a useful checklist of ‘red flag’ conditions in patients presenting with headache.
Most patients with headache have one of the primary headache disorders, such as migraine, but sometimes headache can be the presenting feature of serious neurological disease. Thoughtful and judicious use of investigations is required to diagnose patients with secondary headache, without submitting those with primary headache to unnecessary tests. It is vital to have a strategy in mind when seeing patients with headache as indiscriminate investigation is likely to be unproductive and wasteful.
Useful strategies when diagnosing patients with headache are to:
- classify headaches according to tempo (i.e. the time course of the evolution of symptoms) to help clarify the likely causes and thus determine which investigations, if any, should be pursued
- have in mind a list of ‘red flags’ that would trigger specific investigative paths.
Some of the investigations referred to in this article may be impractical for a GP to undertake. In these situations, referral of patients to an emergency department or for specialist care is appropriate.
A sound understanding of the usual presentation of the common primary headaches is vital (Box 1). Often, these headaches can be diagnosed without the need for special tests. However, sometimes limited investigation is required, if only to fully reassure both the patient and clinician in the case of atypical presentations.
Fortunately, the time course of most primary headaches is characteristic and distinguishes them from other possibilities.
The pattern of headaches can be regarded as:
- acute headache of instantaneous onset (likened to the snap of one’s fingers)
- acute headache developing over minutes to days
- subacute headaches developing over days to weeks
- recurrent headaches
- recurrent facial pain
- chronic headaches (more than 15 days per month for more than three months).
Each of these patterns raises a distinct range of diagnostic possibilities and, hence, a particular approach to investigation.
Instantaneous headache
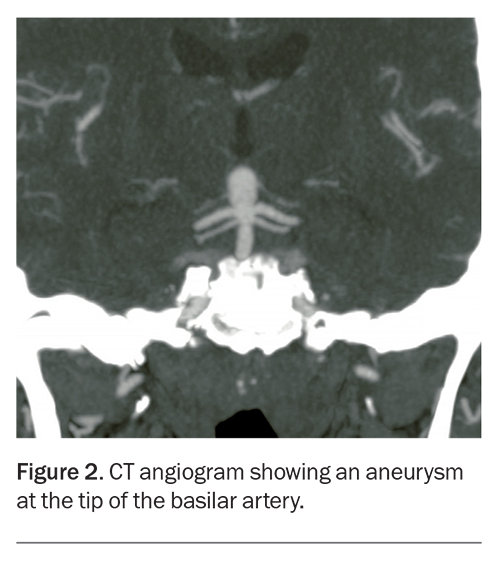
Headache developing instantaneously, likened to the snap of one’s fingers, requires urgent action, mainly to avoid missing the diagnosis of subarachnoid haemorrhage. Although some causes are benign, these can only be diagnosed after serious pathology has been excluded (Box 2).
Subarachnoid haemorrhage
Instantaneous (‘thunderclap’) headache must be regarded as a subarachnoid haemorrhage until proven otherwise. In practice, this will often mean referral of any patient with an acute presentation to an emergency department.
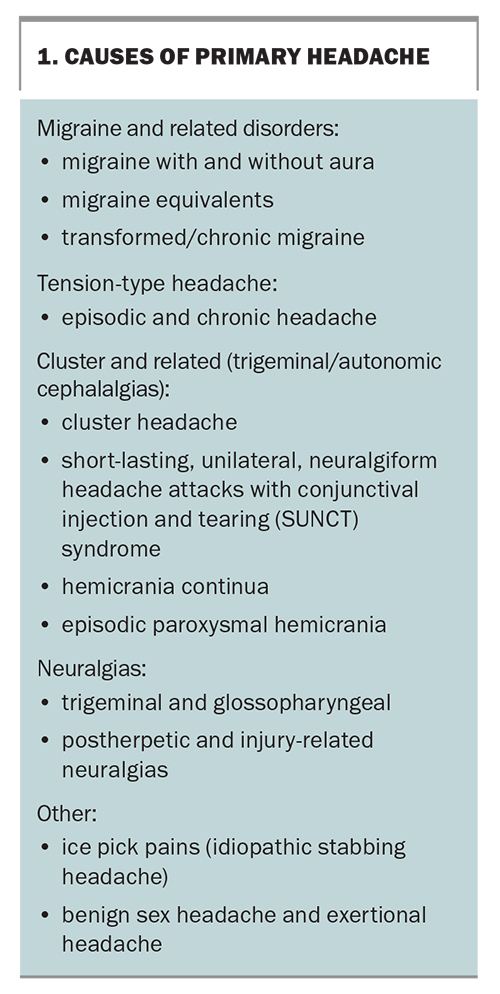
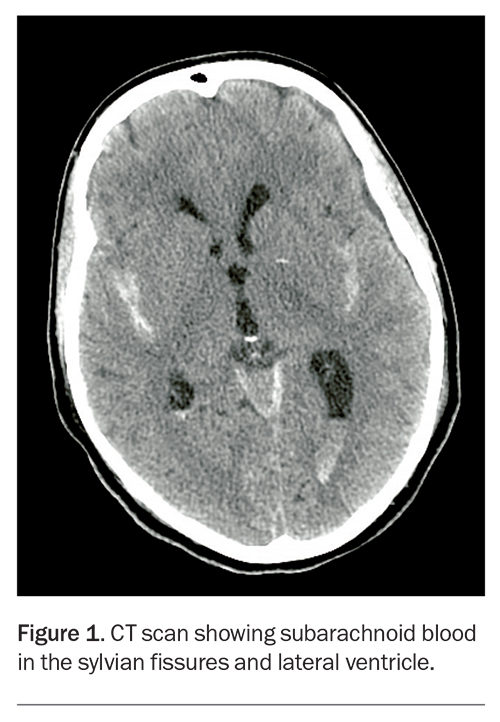
Modern imaging (CT or MRI scans of the brain) is usually sensitive at detecting subarachnoid blood if performed within a few days of a subarachnoid haemorrhage (Figure 1). Lumbar puncture may occasionally show a subarachnoid haemorrhage (by revealing blood or chemically confirmed xanthochromia) when the diagnosis is unclear on imaging, but a traumatic tap may confound interpretation. If the patient presents later than a week after the abrupt headache, subarachnoid blood may no longer be apparent and investigation should then focus on a possible source of the haemorrhage.
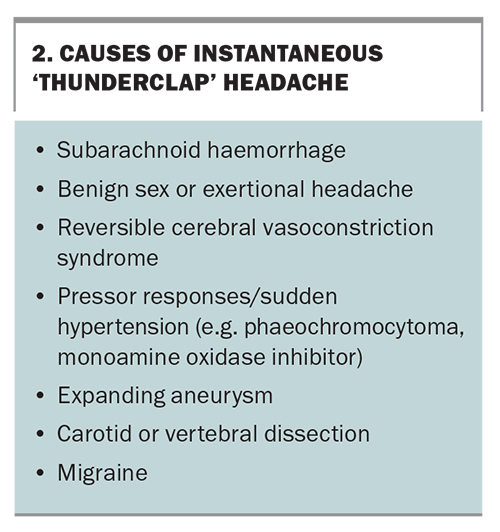
Modern CT angiography (CTA) or magnetic resonance angiography (MRA) is reasonably sensitive at demonstrating aneurysms (Figure 2) and arteriovenous malformations. If a subarachnoid haemorrhage is confirmed, or is strongly suspected despite negative CTA or MRA, a catheter angiography should be performed.
Reversible cerebral vasoconstriction syndrome
Reversible cerebral vasoconstriction syndrome (RCVS) may cause single or recurrent episodes of instantaneous headache. CTA or MRA may show vasospasm, but this may not be apparent immediately; the radiological changes may appear a few days after the initial presentation with headache. Localised ischaemic changes or very focal subarachnoid haemorrhage may be seen in patients with this condition. Some cases of benign orgasmic headache may fit into this category, but usually investigation is normal with this condition. Expanding aneurysms or arterial dissection should be apparent on CTA or MRA.
Phaeochromocytoma
Abrupt onset of headache associated with labile or recent elevation of blood pressure would trigger consideration of a phaeochromocytoma. Appropriate biochemical testing should then be undertaken.
Arterial dissection
Sudden onset of focal pain in the posterior neck (vertebral artery), front of the neck or behind the eye (carotid artery) might suggest possible arterial dissection, especially if associated with trauma to the region. The trauma may be severe (such as from major motor accidents) or minor (such as sharp head turning or chiropractic manipulation). MRA is often very helpful in clarifying this diagnosis, but it must include the vessels in the neck (such views are often not included if they are not specifically requested). CTA and catheter angiography may also show such lesions.
Noninstantaneous acute headache
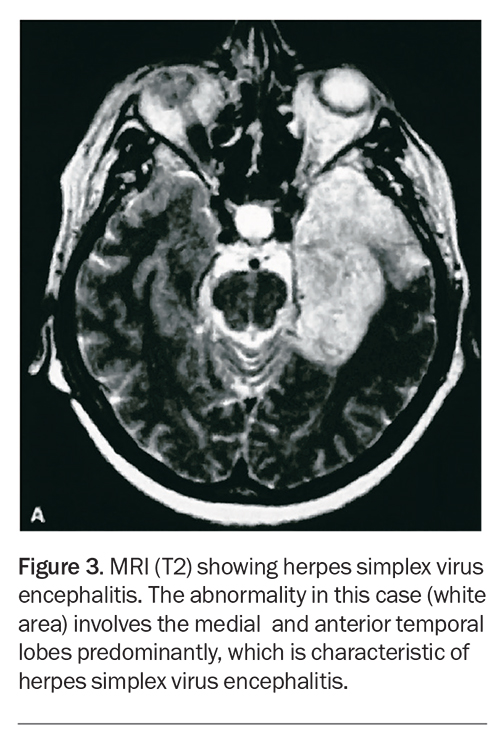
Headaches developing over hours or a day or two should also raise concerns about serious conditions (Box 3). If fever or other indicators of infection are present, meningitis and encephalitis must be excluded.
Meningitis and encephalitis
If bacterial meningitis is a genuine consideration, blood cultures should be taken. Urgent treatment with antibiotics should begin at once, preceding specific investigation that would usually involve brain imaging first and then a lumbar puncture (unless this was contraindicated by the imaging findings).
For possible encephalitis, investigation should include an early MRI scan (Figure 3), a lumbar puncture with a specimen sent for detection of herpes simplex virus by polymerase chain reaction, as well as a routine cell count, culture, biochemistry, and appropriate investigation for less common infectious agents. Treatment with antiviral agents to cover herpes simplex virus infection will usually be started if herpes encephalitis is considered a possibility, pending results of investigations.
Systemic infections
GPs will be familiar with acute viral illnesses such as influenza or infectious mononucleosis presenting with headache as a prominent early symptom. Appropriate investigations should be undertaken if these conditions are suspected.
Headache from raised pressure
Urgent brain imaging should always be undertaken in patients with acutely developing headaches, unless the diagnosis is obvious on clinical grounds. Imaging will show a structural mass lesion large enough to cause headache from raised pressure, including hydrocephalus. Venous sinus thrombosis may be missed if the appearances of the venous sinuses are not examined specifically. Therefore, MR or CT venography should be included in the investigation if this condition is suspected.
Low-pressure headache
Headaches developing or changing in nature after a lumbar puncture or epidural injection raise the possibility of low intracranial pressure, especially if aggravated by the upright posture. Occasionally, similar headaches develop spontaneously (e.g. from leakage of cerebrospinal fluid from a nerve root sleeve).
Postlumbar puncture headaches are often treated with lumbar epidural blood patch, without further investigation, if the clinical presentation is typical. If the diagnosis is in doubt, an MRI scan of the brain (with contrast) may show a very characteristic appearance.
Subacute headache
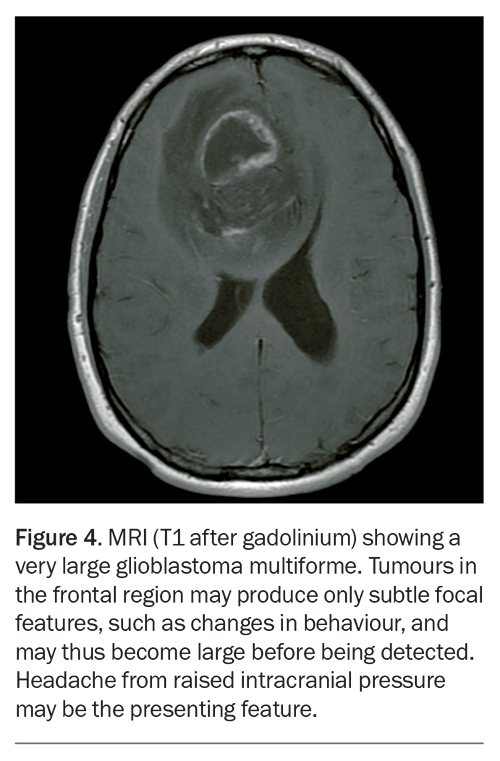
Relentlessly progressing headache over days to weeks is suggestive of serious pathology (Box 4). Once again, brain imaging, preferably MRI, is vital to exclude an intracranial space-occupying lesion (Figure 4) or progressive hydrocephalus. If the symptoms or signs are suggestive of raised intracranial pressure (e.g. a history of visual obscurations on rising to standing or papilloedema on examination) but imaging is unremarkable, benign intracranial hypertension (now usually termed ‘idiopathic intracranial hypertension’) should be considered. This possibility would lead to a lumbar puncture with recording of the cerebrospinal fluid pressure. A lumbar puncture would also be diagnostic in cases of chronic meningitis.
In a patient over 55 years of age with progressive headache, temporal arteritis must be considered and erythrocyte sedimentation rate and C-reactive protein level measured. Temporal artery tenderness should be looked for and temporal artery biopsy should be pursued if the diagnosis seems possible after these preliminary tests.
Headaches may arise from the sinuses, neck, eyes, or temporomandibular joint and dental disorders, but these causes are usually suggested by the history and examination. These possibilities should be pursued with appropriate investigation or referral.
Recurrent headache or facial pain
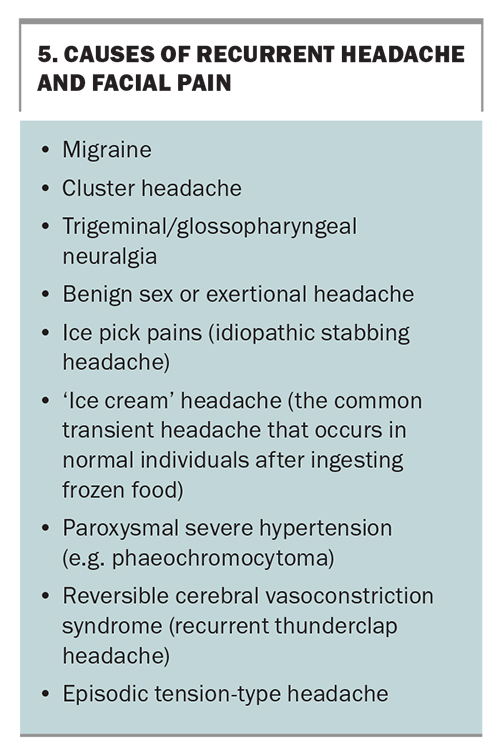
Most patients with recurrent headache have one of the primary headache disorders (Box 5).
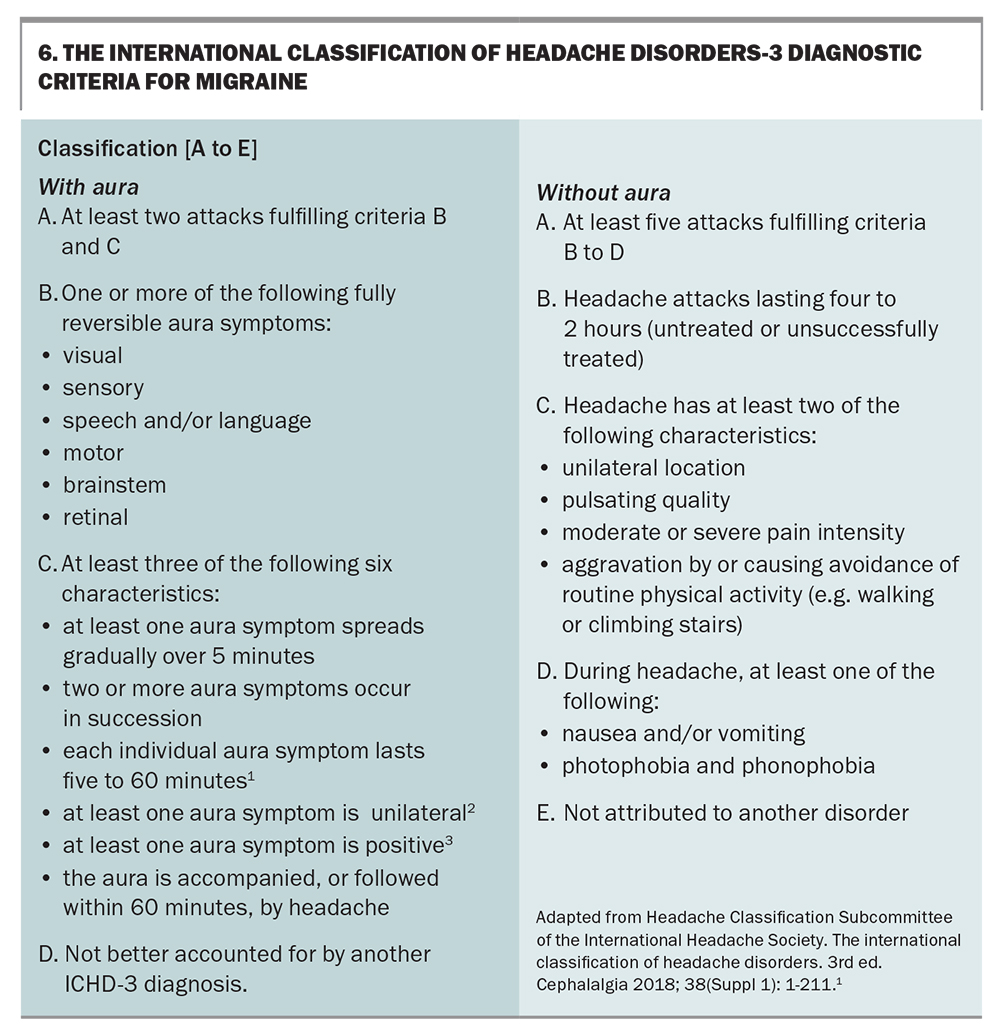
Migraine
Migraine is a diagnosis based on typical clinical features. Criteria have been set out in the International Classification of Headache Disorders (ICHD, 3rd edition; Box 6).1 Migraine is very common and all doctors will have a sound appreciation of the usual features and be attuned to recognising what is atypical. If the history is typical, investigation is usually not required.
Migraine without aura is characterised as a recurrent headache disorder manifesting in attacks lasting four to 72 hours. Typical characteristics of the headache are unilateral location, pulsating quality, moderate or severe pain intensity, aggravation by routine physical activity and association with nausea, photophobia or phonophobia.1
Migraine with aura is a recurrent disorder manifesting in attacks of reversible focal neurological symptoms that usually develop gradually over five to 20 minutes and last for less than 60 minutes. Headache with the features of migraine without aura usually follows the aura symptoms. Less commonly, headache lacks migrainous features or is completely absent. Typical aura consists of visual, sensory or speech symptoms. Gradual development, duration no longer than one hour, a mix of positive and negative features and complete reversibility are characteristic.1
Generally, focal neurological symptoms would be an indication for imaging the brain, unless typical of migraine aura. The usual visual aura symptoms of scintillating scotoma or fortification spectra are well known, but an understanding of the typical evolution of symptoms of migraine with aura over five to 60 minutes is equally important. A more rapid evolution over seconds to a few minutes would raise suspicion of a focal seizure (and thus a likely structural lesion), whereas an abrupt, almost instantaneous onset might suggest stroke or transient ischaemic attack.
Migraine is typically underdiagnosed in the community. The formal ICHD 2nd edition criteria are difficult to remember for day-to-day diagnostic use and simpler user-friendly diagnostic methods have proved to be almost as reliable as the formal criteria. One such approach is the three question method suggested by Lipton and colleagues.2 These three questions are:
- in the past three months, has a headache interfered with your activities on at least one day?
- when you have a headache, do you feel nauseated (sick)?
- when you have a headache, does light bother you?
If the answer is yes to two or three of these questions, the diagnosis is highly likely to be migraine.
Cluster headache
Cluster headache has such a characteristic time course that, in most cases, a firm diagnosis can be made with great confidence from the patient’s history. The attacks are of severe, strictly unilateral pain that is orbital, supraorbital or temporal, or in any combination of these sites, lasting 15 to 180 minutes and occurring from once every other day to eight times a day. The attacks are associated with one or more of the following, all of which are ipsilateral: conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis and eyelid oedema. Most patients are restless or agitated during an attack.1
As lesions in the region of the cavernous sinus can sometimes produce a similar clinical picture to cluster headache, most neurologists would now obtain an MRI scan and MRA of the brain in such cases. However, the results are rarely abnormal.
Trigeminal neuralgia
Trigeminal neuralgia is a unilateral disorder characterised by brief electric shock-like pains. They are abrupt in onset and termination, and limited to the distribution of one or more divisions of the trigeminal nerve. Pain is often evoked by trivial stimuli, including washing, shaving, smoking, talking or brushing the teeth (trigger factors), and frequently occurs spontaneously. Small areas in the nasolabial fold and chin may be particularly susceptible to the precipitation of pain (trigger areas). The pain usually remits for variable periods.1
Trigeminal neuralgia is often due to compression of the root entry zone of the nerve by a vascular loop. This may be apparent with carefully directed MRI or MRA, which should also detect other less usual causes, such as other lesions compressing the nerve or a plaque of multiple sclerosis in the pons.
Ice pick pains (idiopathic stabbing headache)
Idiopathic stabbing headache is transient and consists of localised stabs of pain in the head. These pains occur spontaneously in the absence of organic disease of underlying structures or of the cranial nerves. This is a relatively common and benign disorder.
Benign sex headache and exertional headache
As subarachnoid haemorrhage may occur during exertion or sexual activity, headache occurring in these contexts must always be taken seriously. Naturally, if many similar events have occurred with no disastrous consequences, subarachnoid haemorrhage is much less likely. However, RCVS is still a concern and appropriate imaging is required.
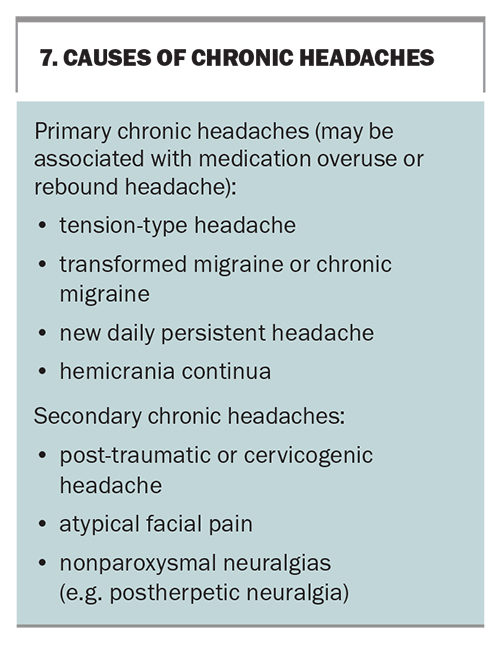
Chronic headache
There has been much interest in recent years in the concept of chronic daily headache. This is a pattern of headache occurring more than four hours per day for 15 or more days per month and for more than three months. Headaches arising from cervical spine pathology or persistent neuralgic pain after herpes zoster virus infection would fall into this category and are usually easy to recognise. The term ‘chronic daily headache’ is usually reserved for the primary headaches presenting with this time course (Box 7).
Mild cases often fall into the category of tension-type headache (defined in essence as primary headache without migrainous or other diagnostic features), but most disabling cases have chronic migraine. Chronic migraine is diagnosed when a patient has 15 or more days of headache per month with migraine features on at least eight days. Many patients evolve from a pattern of episodic typical migraine to a more frequent headache pattern with fewer typical migrainous features. Excessive (e.g. more than 10 days per month) use of acute medications, such as ergotamines, triptans or codeine, may contribute to this transformation.
New daily persistent headache begins over one to three days and then persists, with the patient usually being able to give the precise date of onset. This rare type of headache is notoriously difficult to treat. Hemicrania continua is a rare, strictly unilateral headache that is specifically responsive to indomethacin.
In general, the group of patients with chronic headache is challenging to manage and taking a detailed history is vital. Investigation is usually normal but imaging is undertaken at some stage in most of these patients.
Recognising the ‘red flags’
One mnemonic for red flag signs in patients with headache is ‘SNOOP-4’, which is outlined below:3
- systemic symptoms and signs, such as fever, myalgias and weight loss, could point to giant cell arteritis or an infection; systemic disease, such as malignancy and AIDS, suggests metastatic disease or an opportunistic central nervous system (CNS) infection
- neurological symptoms or signs raise suspicion for structural, neoplastic, inflammatory or infectious CNS disease
- onset, as in sudden-onset conditions (e.g. thunderclap headache), could indicate an underlying stroke, subarachnoid haemorrhage, cerebral venous sinus thrombosis, RCVS or arterial dissection
- onset after 50 years of age suggests structural, neoplastic, inflammatory or infectious CNS disease, or giant cell arteritis
- pattern change (if there is a previous history) could point to progressive headache with loss of headache-free periods
- precipitated by valsalva manoeuvre, which suggests Chiari malformations, structural lesions that obstruct cerebrospinal fluid flow or a cerebrospinal fluid leak
- postural aggravation, which is headache worsened by either standing or lying down, suggests intracranial hypotension from a cerebrospinal fluid leak or intracranial hypertension, respectively. Aggravation by certain neck movements and positioning might indicate cervicogenic headache
- papilloedema, when present, raises the suspicion of intracranial hypertension.
Investigations to reassure the patient
Most patients with recurrent or chronic headaches have ‘primary’ headaches, therefore, investigations are likely to be normal. The patient often finds it difficult to believe that severe headache is not associated with structural brain pathology and sometimes imaging is needed to quell such fears. This often leaves the doctor feeling uncomfortable, either for ordering what seems to be an unnecessary test or for failing to allay the patient’s concerns. In these cases, it is inadvisable to arrange an inadequate investigation that fails to definitively exclude the disorders causing concern.
If any imaging is contemplated, it is better to initially perform an MRI scan, rather than a CT scan, as CT findings often necessitate the patient subsequently undertake an MRI. MRI is clearly superior in excluding structural lesions that are likely to cause headache, and the radiation dose, which is an issue with CT, is not an issue with MRI. The practical difficulty is the policy of differential Medicare reimbursement for CT versus MRI when requested by a GP.
Patients with migraine or tension type headache are not immune to other disorders. A secure knowledge of the usual features of these disorders allows for recognition of a significant change that might imply alternative pathology.
Conclusion
Although there is no simple or global rule to guide the investigation of a patient with headache, a careful and focused clinical assessment, with particular emphasis on the tempo of the headache’s evolution, can help establish a cause. The approach to investigation for recently developed headaches is greatly different from that of longstanding chronic or recurrent headaches. MT
COMPETING INTERESTS: Dr Stark has received lecture fees from Allergan, Janssen-Cilag, MSD and Pfizer, and consultancy fees from Allergan, Janssen-Cilag and Pfizer.
References
1. Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders. 3rd ed. Cephalagia 2018; 38(Suppl 1): 1-211.
2. Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: The ID Migraine(TM) validation study. Neurology 2003; 61: 375-382.
3. Silberstein SD, Lipton RB. In: Silberstein SD, Lipton RB, Dodick DW, eds. Wolff’s headache and other head pain. 8th ed. New York: Oxford University Press; 2008: 315-377.