Acute coronary syndromes – improving outcomes in women
Cardiovascular disease is a leading cause of death around the world and represents a major threat to the health of Australian women, in whom it is under-recognised. Acute coronary syndromes often present differently in women than in men, and women may be undertreated, receiving less risk factor modification, less invasive treatment and less guideline-recommended secondary preventive medication after a cardiac event. Efforts must be made to improve the risk profile, awareness and treatment of cardiovascular disease among women in Australia.
- Cardiovascular disease remains the leading cause of death in Australia and represents a major threat to the health of Australian women, in whom it is under-recognised.
- Compared with men, women have a higher prevalence of certain traditional cardiac risk factors but receive less intensive risk factor modification.
- Women have greater mortality associated with cardiovascular disease.
- Women with acute coronary syndromes present differently to men and are often undertreated.
- There is potential to improve awareness and treatment of cardiovascular disease among women in Australia.
Cardiovascular disease remains the leading cause of death in Australia and around the world. It incorporates a group of highly preventable and treatable diseases affecting the heart and blood vessels, including coronary artery disease, heart failure, stroke and peripheral vascular disease.1 These conditions represent a major threat to the health of Australian women, the extent of which is often underestimated because of a misconception that women are ‘protected’ against cardiovascular disease.2
Compared with men, women have a higher prevalence of certain traditional risk factors, such as hypertension and diabetes, but often receive less intensive risk factor modification.3 Additionally, women present later and have greater mortality associated with their disease.4,5 There is potential to improve the risk profile, awareness and treatment of cardiovascular disease among Australian women, thereby reducing the number of women affected by these conditions.
This article focuses on the female pattern of ischaemic heart disease specific to acute coronary syndromes (ACS), broadly including takotsubo cardiomyopathy and ischaemia with no obstructive coronary artery disease (INOCA), and the investigation and management considerations that are important in this population.
Presentation
ACS is defined as any group of clinical symptoms compatible with acute myocardial ischaemia. This includes unstable angina, non-ST-segment myocardial infarction and ST-segment-elevation myocardial infarction (STEMI) and has traditionally been associated with obstructive coronary artery disease.6
Acute occlusion of the coronary arteries is caused by disruption of plaque and formation of a thrombus, which subsequently limits blood flow to the myocardium.7 The pathophysiology of coronary artery disease and ACS is different in women than in men, as women are less likely to present with plaque rupture.8
There are also significant differences in the clinical presentation of ACS between men and women. Women frequently present later and with more atypical symptoms, such as pain in the upper back and neck, fatigue, nausea and vomiting.9 These differences in symptom presentation are thought to account in part for the underdiagnosis and undertreatment of women with ACS.10
Prognosis
There is an alarming gender gap in mortality associated with coronary artery disease and myocardial infarction. Women, particularly younger women (less than 55 years of age), face a worse prognosis than men when presenting with ACS.11,12 Adjustment for disease severity, comorbidity and treatment does not fully account for this gap, which may represent a sex-specific pathophysiology of ACS that remains poorly understood.
Management
The use of guideline-directed therapy after ACS is beneficial to both men and women.13 Despite overall improvements in the implementation of guideline-directed therapy, optimal medical therapy continues to be underused in women compared with men.14
Recently published data from the Australian CONCORDANCE (Cooperative National Registry of Acute Coronary Care, Guideline Adherence and Clinical Events) registry showed that women with STEMI were less likely than men to have undergone coronary angiography, timely revascularisation or primary percutaneous coronary intervention.10 Furthermore, on discharge, women were significantly less likely to receive guideline-recommended secondary preventive medications. These discrepancies in management were seen after adjusting for confounding factors, such as age, comorbidities and baseline risk levels.10
More work is needed to identify the persisting barriers to the equitable treatment of ACS in women.
Takotsubo cardiomyopathy
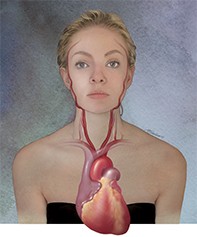
ACS can be mimicked by other conditions, such as takotsubo cardiomyopathy (Figure). This is a transient nonischaemic cardiomyopathy that is characterised by left ventricular dysfunction and is often accompanied by ECG changes and elevation in cardiac biomarker levels consistent with myocardial infarction. It is likely mediated by catecholamine excess and is usually seen in the context of acute physical or psychological stress.15
Takotsubo cardiomyopathy is thought to represent up to 2% of all admissions with presumed ACS and is almost always seen in women. A large-scale US database study looking at trends of takotsubo cardiomyopathy over five years showed that women consistently represented more than 90% of presentations.16 The mechanism behind this gender difference is unclear, although oestrogen is thought to play a role in the catecholaminergic response to stress.17
Reported outcomes in patients with takotsubo cardiomyopathy are generally favourable, with low in-hospital mortality and recovery of left ventricular function within weeks to months in most patients.18 Although the prognosis for takotsubo cardiomyopathy is typically very good, some patients experience a recurrence. The determinants of this are not well understood, although recurrence often occurs in patients who had severe left ventricular dysfunction at the index event and in younger female patients (aged less than 50 years).19
There are no consensus guidelines on the management of takotsubo cardiomyopathy and, as such, treatment is individualised. Long-term beta blocker therapy is often adopted, with the goal of preventing recurrence. Serial imaging with transthoracic echocardiography is warranted to exclude dangerous complications, such as left ventricular thrombus or outflow tract obstruction, and to ensure the recovery of the left ventricle.15
Further investigation is needed to identify optimal management of this condition and to clarify the pathogenic background that results in the gender-related differences in prevalence.
Spontaneous coronary artery dissection
Spontaneous coronary artery dissection (SCAD) is a cause of ACS that is more prominent in women than men and often affects patients under the age of 50 years who have minimal or no cardiac risk factors.20 It is caused by a tear in the wall of the coronary artery, which results in the formation of a haematoma, leading to obstruction of coronary artery blood flow to the myocardium.7
Although previously thought to be a rare condition, advancements in intravascular imaging used at the time of coronary angiography have improved awareness and diagnosis of SCAD.21 Notably, recent studies have implicated SCAD in 35% of myocardial infarctions among women aged under 50 years, and SCAD is the most common aetiology of pregnancy-associated myocardial infarction.22,23
Management of SCAD is usually conservative, and there are low rates of inhospital adverse events. Despite this, recurrent cardiovascular events are common in this group, with up to 10% of patients having another episode of SCAD. The use of beta blockers and aggressive treatment of hypertension are thought to be protective and should be considered in all patients with SCAD.24
Ischaemia with no obstructive coronary artery disease
INOCA is prevalent among women. First described more than 40 years ago, the aetiology and pathogenesis of this phenomenon are still a source of debate. Proposed mechanistic pathways include adverse coronary reactivity, distal embolisation, concealed atherosclerosis and endothelial and microvascular dysfunction.25
Given the array of possible underlying mechanisms, there is considerable variability in prognosis and management. The Cardiovascular Disease in Women Committee of the American College of Cardiology and other interested groups recently convened a working group to develop a consensus on the syndrome of INOCA. It found that these patients have an elevated risk of a cardiovascular event, including ACS, hospitalisation for heart failure, stroke and repeated cardiovascular procedures.26 Despite this, the lack of obstructive coronary artery disease in these patients leads to under-recognition of heart disease and thus less aggressive treatment strategies.
There is a paucity of evidence for the treatment of this condition, and management is focussed on symptom control alone. This is in part because clinical trials of patients with ischaemic heart disease and ACS have focused on the traditional mechanism of plaque rupture and obstruction. As women are more likely to present without plaque rupture or obstruction, women with INOCA have been under-represented in these trials.
Conclusion
Persisting differences in the investigation and management of men and women with coronary artery disease are disconcerting. Undertreatment of women with coronary artery disease has been a consistent feature of ACS management in several studies.5,9,11 This might be caused by poor awareness of their risk or by clinician bias towards undertreatment, based on a misunderstanding of the pathophysiology of coronary artery disease in women. Whatever the mechanism, this gender disparity must be addressed. Attention should be given to improving the risk profile, awareness and treatment of cardiovascular disease among Australian women, thereby reducing the number of women affected by these conditions. MT