Male genital dermatology. Part 2: Noninflammatory lesions
Many male patients with genital disease have an underlying fear of genital cancer. A compassionate approach, accurate diagnosis and appropriate treatment and follow up are essential to minimising personal and relationship distress for patients with benign, premalignant or malignant lesions.
- Accurate diagnosis of any hyperpigmented genital lesion is important as such lesions may raise concerns about genital melanoma.
- Genital melanotic macules need to be differentiated from melanoma.
- Genital dysaesthesia is an increasingly recognised disorder of male genitalia that often leads to marked distress.
- Genital seborrhoeic keratoses need to be differentiated from sexually acquired genital warts (condyloma acuminata) because a wrong diagnosis may lead to both significant personal and relationship distress.
- Penile intraepithelial neoplasia or in situ squamous cell carcinoma (SCC) is the most important premalignant male genital skin disease.
- Penile SCC is an uncommon cancer affecting mostly uncircumcised older men that is increasing in the developed world.
The first part of this review of male genital dermatology in the April issue of Medicine Today covered inflammatory male genital dermatoses. This second part covers pigmentary disorders of the male genitalia, genital dysasthesia and premalignant and malignant genital skin diseases.
Pigmentary disorders
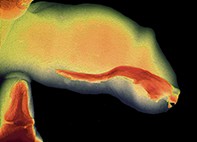
The male genitalia vary greatly in colour and appearance. The most important causes of acquired depigmentation or hypopigmentation are vitiligo and lichen sclerosus. Important acquired hyperpigmentary disorders of the male genitalia include postinflammatory hyperpigmentation, lichen planus, benign tumours (melanocytic naevi, seborrhoeic keratoses), genital melanotic macules (genital melanosis; Figure 1) is very rarely melanoma.
Genital melanotic macules (genital melanosis) is a benign, acquired pigmentary disorder that needs to be differentiated from the more serious genital melanoma. These two distinct disorders can have a similar appearance but have dramatically different prognoses. The cause of genital melanotic macules is unknown but may represent postinflammatory hyperpigmentation to cutaneous disorders such as lichen planus. Genital melanotic macules usually present as well-circumscribed, asymptomatic tan to dark brown macules or small patches (flat) on the foreskin, glans or penile shaft. These hyperpigmented macules or patches may cause great concern due to fear of a genital melanoma. Genital skin biopsy is essential to make the diagnosis. Genital melanotic macules usually persist long-term. Long-term follow up with clinical photographs is wise to detect any change as a genital skin biopsy is usually only a sample of any hyperpigmentary macule or patch (as the whole lesion is usually not totally removed).
Genital melanoma usually appears as an irregular hyperpigmented patch on the glans, foreskin or penile shaft, with an irregular border and uneven pigmentation. Genital melanoma needs to be diagnosed promptly as a delay in diagnosis may worsen the prognosis. As with all genital malignant disease it is important to submit as much tissue as possible combined with clinical notes to help the histopathologist make a diagnosis. Ideally, the entire hyperpigmented macule or patch should be removed for histological examination. However sometimes only a sample of the hyperpigmented macule or patch can be sampled for histological examination. If there is any doubt about the diagnosis, expert opinion should be sought.
Genital dysaesthesia
Genital dysaesthesia is also known as red scrotum syndrome, burning scrotum syndrome and penoscrotodynia (Figure 2). The condition results in burning or an irritable sensation with variable levels of distress. The genitalia of men with genital dysaesthesia appear normal and are not necessarily red in colour. Asymptomatic redness of the scrotum is seen in many men with a fair complexion and rosacea.
Genital dysaesthesia is both under-reported and challenging to manage, and a supportive doctor-patient relationship is important. The aim of treatment is to reduce the severity of symptoms and not necessarily ‘cure’ genital dysaesthesia. Treatments include off-label use of oral amitriptyline, doxycycline, gabapentin, pregabalin and serotonin and noradrenaline reuptake inhibitors. Topical treatments include cool compresses, 1% menthol in aqueous cream and topical lignocaine (lidocaine) spray. No treatment works for every patient, and patients need reassurance that they do not have a sexually transmissible infection (STI) or genital cancer.
Benign skin lesions
Benign acquired melanocytic naevi may occur on genitalia. Occasionally dysplastic (atypical) melanocytic naevi are also seen, causing concern about possible melanoma. Although acquired melanocytic naevi are the most common benign skin lesion in people under 40 years of age, seborrhoeic keratoses become more common later in life (Figure 3). The cause of seborrhoeic keratoses is unknown. They usually present as asymptomatic warty (verrucous) papules or plaques, ranging from skin-coloured to brown or black. Seborrhoeic keratoses may occur on male genitalia and are often confused with genital warts, bowenoid papulosis, genital melanotic macules or even melanoma.
Premalignant genital diseases
The most important premalignant genital diseases are lichen sclerosus and penile intraepithelial neoplasia (PIN). It is uncertain whether erosive lichen planus is precancerous for penile squamous cell carcinoma (SCC). Rarer premalignant genital diseases include penile horn and pseudoepitheliomatous keratotic and micaceous balanitis (PEKMB).
PIN has the histological features of intraepithelial carcinoma or in situ (level 1) SCC and has three morphological forms: erythroplasia of Queyrat, Bowen’s disease and bowenoid papulosis. It most commonly presents as asymptomatic red macules, papules, nodules or plaques. PIN of the glans penis or foreskin was previously known as erythroplasia of Queyrat (Figure 4). PIN located on the penile shaft or scrotum is termed genital Bowen’s disease. Bowenoid papulosis has the same histological features but is more strongly associated with human papillomavirus (HPV) infection and follows a relatively benign course.
The aetiology of PIN is not certain, but the risk factors are similar to those for penile SCC (discussed below): being uncircumcised, having lichen sclerosus, HPV infection, smoking and immunosuppression. Although PIN usually presents as red macules, papules, nodules or plaques, it may present as diffuse redness of the glans and inner foreskin (balanoposthitis). It may be asymptomatic, itchy or irritated, or may occasionally bleed. If PIN is suspected, skin biopsy is mandatory. A low threshold for genital skin biopsy is recommended if premalignant or malignant disease cannot be confidently excluded.
Once diagnosed, the most important initial treatment for PIN of the glans or foreskin is circumcision. Circumcision debulks precancerous disease, removes tissue with subclinical HPV infection, makes application of topical therapy easier and reduces the likelihood of missing the development of invasive SCC. Circumcision is combined with different local treatments including shave excision, cryotherapy, curettage and electrocautery, topical fluorouracil, topical imiquimod, surgical excision, Mohs micrographic surgery and total resurfacing of the glans with skin grafting. Use of topical cidofovir, laser destruction and photodynamic therapy has also been reported. The role of HPV vaccination as adjuvant treatment for PIN is unproven and controversial. Long-term follow up is essential to assess response to treatment and to detect recurrence of PIN and development of invasive SCC. Persistent PIN requires surgical excision with penile preserving techniques.
Bowenoid papulosis usually presents as multiple papules varying in colour from skin-coloured to red or brown on the foreskin, distal penile shaft and glans. Younger, sexually active, heterosexual males are more commonly affected, and there is a strong association with HPV infection. The risk of malignant transformation is unknown, but bowenoid papulosis rarely progresses to invasive SCC. Circumcision is an important part of treatment combined with cryotherapy, curettage and electrocautery or topical imiquimod. Bowenoid papulosis is probably often mistaken for and treated as genital warts. The strong association between bowenoid papulosis and HPV infection supports use of HPV vaccination as an adjuvant treatment for bowenoid papulosis. Long-term follow up is essential for assessing the response to treatment and monitoring for possible malignant transformation, even if this is very unlikely. Partners of patients need to be screened for other HPV-associated disease (cervical, vulval and anal intraepithelial neoplasia). The importance of HPV vaccination should be discussed.
Genital cancer
Penile SCC is an uncommon cancer seen in uncircumcised older men. Penile cancer is increasing in the developed world. The cause of this increase is unknown but may partly be due to decreasing rates of male (infantile) circumcision, earlier onset of sexual activity and an increase in the lifetime number of sexual partners.
Aetiological factors for penile SCC are similar to those for PIN, including increasing age, presence of a foreskin (neonatal circumcision reduces the risk), phimosis, chronic inflammatory genital disease (mostly penile lichen sclerosus), smoking, treatment with photochemotherapy (psoralen and ultraviolet A [PUVA] therapy), multiple sexual partners (with earlier onset of sexual activity) and immunosuppression. Treating chronic inflammatory genital disease, limiting genital HPV infection, treating phimosis, avoiding genital ultraviolet exposure and helping patients to stop smoking all help reduce a patient’s risk of penile SCC.
Routine vaccination of adolescent males with HPV vaccine before they become sexually active is an important part of limiting HPV infection. About 50% of penile SCCs are associated with HPV infection, so it is hoped there will be a reduction in penile SCC in the future. However, HPV vaccination may not have the same impact on male genital cancer as seen in the reduction of female genital tract cancer.
Penile SCC usually presents as an asymptomatic plaque or nodule on the glans (Figure 5). Ulceration may be evident. Early SCC of the glans may be subtle induration rather than an exophytic nodule. There may be evidence of coexistent PIN or lichen sclerosus (both premalignant diseases). Histological confirmation of the diagnosis and clinical assessment of regional lymph nodes and internal organ enlargement to detect metastatic disease are essential. Sentinel lymph node biopsy, CT scanning and MRI can help stage penile cancer.
Treatment of metastatic disease is undertaken by a multidisciplinary team of urological surgeons, radiation oncologists and medical oncologists. Treatment of penile cancer involves surgical resection, radiotherapy, chemotherapy and modern targeted therapy. Penile preserving surgery is important, but total glansectomy or total penectomy may occasionally be necessary. Long-term follow up is essential.
Rarer genital cancers include giant condyloma acuminatum (Buschke-Lowenstein tumour) or verrucous carcinoma, extramammary Paget’s disease, melanoma, basal cell carcinoma, Kaposi’s sarcoma and cutaneous penile metastases.
Conclusion
Many men who approach their GP with concerns about genital lesions are fearful of having an STI or cancer. Accurate diagnosis based on thorough examination and a broad knowledge of the features of the wide range of both inflammatory and noninflammatory male genital disorders is crucial to providing appropriate treatment and follow up. MT