Leprosy: a forgotten disease?
Despite a dramatic fall in the worldwide prevalence of leprosy and the widespread availability of curative therapy, new cases continue to be reported in Aboriginal Australians and in migrants from countries where the disease remains endemic. Leprosy must not become a forgotten disease, as ongoing awareness among health professionals is essential to ensure early detection and effective drug therapy.
Leprosy (Hansen’s disease) is a chronic granulomatous disease caused by Mycobacterium leprae. It primarily affects the skin and peripheral nerves but the eyes, testes, bones and upper respiratory tract may also be affected. A number of unique features of the disease present significant diagnostic and management challenges for clinicians. The spectrum of disease expression is wide and the incubation period is variable and potentially lengthy (five to 30 years). The duration of therapy is prolonged (six to 24 months) and there is potential for nerve damage at any stage of the disease. Leprosy remains a feared disease, and patients are often very concerned about social stigma and deformity.
Epidemiology
In 1991, the World Health Organization (WHO) resolved ‘to eliminate leprosy as a public health problem by the year 2000’, with elimination being defined as fewer than one case per 10,000 population.1 Through the use of free multidrug therapy, enhanced case detection and other measures, a striking fall in worldwide prevalence has been achieved, from more than five million cases in 1985 to 174,608 in 2015 (prevalence defined as the number of patients on drug therapy).2 It is important to note that these prevalence figures are significantly affected by operational factors, such as intensity of case finding activities. The reduction in the new case detection rate (a more accurate marker of transmission) has been far more modest. Despite the availability of curative drug therapy, it has not been possible to eliminate leprosy in many parts of the world.
Although Australia has achieved the WHO goal of eliminating leprosy as a public health problem (i.e. <1 case/10,000 population), there continues to be a small number of cases recorded each year. The majority of these are acquired overseas in countries where leprosy is endemic, particularly Sri Lanka, India, the Philippines and Indonesia. Locally acquired infections, which are uncommon, almost exclusively affect Aboriginal Australians, with the highest case rates recorded in Western Australia, followed by the Northern Territory.3
Pathogenesis
M. leprae is an acid-fast bacillus and the only pathogen to cause infection of peripheral nerves, with nerve damage resulting from both direct invasion and the host immune response to the pathogen.4 Understanding of the pathogenesis of the disease has been hindered by an inability to culture the organism in the laboratory (due to its requirement for highly specialised ecological niches). Humans and armadillos (in the Americas) are the only known reservoirs of infection. Transmission is believed to occur primarily by aerosol spread of droplets from the nasal mucosa of a subgroup of infectious patients.5 Not all patients are infectious, and prolonged periods of close household contact (>6 months) are thought to be required in most cases.
When M. leprae enters the body, most people mount an effective immune response and do not develop disease. Clinical expression of disease in the remainder is determined by each individual’s cell-mediated immunity (CMI), with tuberculoid disease occurring in those with a strong CMI response and lepromatous disease in those with a very poor CMI response to the infection. Patients that fall into the borderline states between these two polar forms have variable and unstable CMI responses (Figure 1).
Disease classification
There are two systems of classification currently in use for leprosy. These are used to determine infectivity and predict complications, as well as to guide therapy and contact tracing.
- The Ridley–Jopling classification system (Table 1) identifies five forms of leprosy on the basis of clinical features, histopathology and microbiology. These range from the polar tuberculoid form (localised disease with M. leprae undetectable in slit skin smear specimens), through three immunologically unstable borderline forms to the polar lepromatous form (disseminated disease with M. leprae abundant and readily detectable in slit skin smear samples).6
- The WHO classification system identifies two categories of leprosy and is designed to simplify diagnosis in the field. It is based on the number of skin lesions, with up to five lesions classified as paucibacillary leprosy and more than five lesions as multibacillary leprosy.
Pure neural leprosy, in which skin lesions are absent, is not included in either of the above mentioned classification systems. A high degree of clinical suspicion, exclusion of other diagnoses and compatible epidemiology (with or without nerve biopsy) are required for a diagnosis of pure neural leprosy.
Clinical features
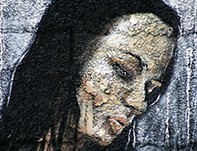
Clinical expression of leprosy is highly variable and the presentation is dependent on the type and stage of disease. Macules, papules, plaques and urticaria-like lesions with central clearing and skin infiltration can occur (Figures 2 to 4). Involved peripheral nerves become enlarged and may be tender (Figure 5). Nerve involvement can result in damage to sensory, autonomic and motor fibres, resulting in anaesthesia, skin dryness and weakness, predisposing to trauma and chronic ulceration (Figure 6). The most commonly involved nerves are the supraorbital, greater auricular, ulnar, median, radial cutaneous, common peroneal and posterior tibial nerves. M. leprae grows optimally at 27 to 32oC, which explains the predilection for nerves at the most superficial and cooler body sites.
Patients with tuberculoid leprosy often present with one or few skin lesions (Figure 2), and may or may not have symptoms related to an enlarged peripheral nerve (e.g. numbness, tingling, pain or weakness). Patients with lepromatous leprosy tend to present later, with widespread symmetrical skin lesions (Figure 4) and milder nerve involvement of multiple nerve trunks (occasionally presenting as mononeuritis multiplex); they may also have other symptoms such as nasal stuffiness, peripheral oedema, visual disturbance and manifestations of organ involvement. Most patients fall into the borderline states between these two polar forms, and present with features along this spectrum.
The first presentation of leprosy may be a lepra reaction, which is a host immunological reaction to the infection. The symptoms of lepra reactions include nerve pain and/or tenderness, acute nerve palsy, multiple new skin lesions (often nodular) and eye pain (uveitis). There may also be systemic febrile illness, which is usually associated with other features.
Diagnosis
The diagnosis of leprosy requires a high level of clinical suspicion. The differential diagnosis is extremely broad and includes cutaneous tuberculosis, cutaneous sarcoidosis, fungal infection, birthmarks, discoid eczema and systemic lupus erythematosus. Careful adherence to the National Notifiable Diseases Surveillance System (NNDSS) case definition for leprosy is required to avoid misdiagnosis; a summary is presented in Box 1, and further information is available from the Department of Health website.
A diagnosis of leprosy should be considered in Aboriginal patients and those from endemic regions presenting with unexplained skin or nerve symptoms. Patient assessment includes a careful history (including place of birth, travel and contacts) and clinical examination of the skin and peripheral nerves. Peripheral nerve function should be assessed with voluntary motor and sensory testing.
An eye examination should be conducted, looking for ocular manifestations of leprosy such as madarosis, lagophthalmos, blink dysfunction and signs of lepra reactions (e.g. iridocyclitis, scleritis). The risk of eye damage is highest in patients with facial skin lesions and those with lepromatous disease.
A slit skin smear test is indicated when there is clinical suspicion of leprosy to detect acid-fast bacilli in tissue fluid. Skin biopsy (ideally full-thickness elliptical) may be necessary, to assess for histological changes and to detect acid-fast bacilli on staining and M. leprae DNA on polymerase chain reaction (PCR) testing.7
Nerve conduction studies and nerve biopsy are required rarely.
Referral
A definite case of leprosy should be notified to the relevant state public health unit (Box 1) and referral arranged for specialist review. Referral pathways differ by state, but it would be appropriate to refer to an infectious diseases physician, clinical microbiologist or dermatologist for assessment. Referral of a patient should also be arranged when there is suspicion of leprosy but the diagnosis is uncertain.
Management
Multidrug therapy (MDT) is the cornerstone of management of patients with leprosy. Baseline investigations prior to commencing drug therapy include:
- full blood count
- electrolytes, urea and creatinine
- liver function testing
- hepatitis, HIV and strongyloides serology
- glucose-6-phosphate dehydrogenase (G6PD; increased risk of haemolytic anaemia with dapsone in patients with G6PD deficiency)
- Mantoux test and chest x-ray (to exclude active tuberculosis or latent tuberculosis infection).
A summary of recommended MDT regimens for leprosy in adults, including the WHO regimen, is presented in Table 2.8-10 Local guidelines often differ with regard to duration of therapy – for example, the US National Hansen’s Disease Program recommends 12 months of treatment for paucibacillary disease and 24 months for multibacillary disease,9 and the Northern Territory Centre for Disease Control recommends 24 months of treatment for patients with more severe forms of multibacillary disease.10 Single skin lesion leprosy is treated as paucibacillary leprosy. Pure neural leprosy is generally treated like multibacillary leprosy. The medications are most commonly distributed in prepackaged blister packs (‘WHO packs’), which are provided at no cost to all patients around the world. Latent tuberculosis can be treated simultaneously.
Management of patients with leprosy requires a multidisciplinary approach. MDT is generally prescribed through a specialist centre, with GPs playing a central role in ensuring uninterrupted drug supply, monitoring for side effects (Box 2), assisting with compliance and providing psychological support. Case management involves patient education, as well as prompt diagnosis and management of lepra reactions (see below) and co-ordination of allied health professionals involved in long-term follow up (e.g. physiotherapists and podiatrists for patients with irreversible nerve impairment). Silent or painless neuropathy is common in patients with leprosy, highlighting the importance of regular testing of voluntary motor and sensory function; the procedure for performing the tests and recording results is described in Guidelines for the Control of Leprosy in the Northern Territory.10 Any deterioration in function should prompt urgent specialist referral to avoid permanent nerve injury.
Lepra reactions
Patients may experience lepra reactions before, during or even after completion of curative therapy for leprosy. These immunological reactions can result in inflammation of peripheral nerves and existing skin lesions (type 1 reaction) or in severe systemic illness as in erythema nodosum leprosum (ENL; type 2 reaction). Prompt diagnosis and treatment are essential to prevent permanent nerve and eye damage, and consequent deformity and disability.
Presentations
Patients with type 1 reactions often present with inflammation of existing skin lesions, with or without nerve pain or tenderness or impaired nerve function. Features that may suggest ENL include new skin lesions, eye erythema and pain, nephritis, fever, arthritis, dactylitis, lymphadenopathy, generalised pain and malaise. Voluntary motor and sensory function testing should be performed frequently during lepra reactions.9
Treatment
Mild lepra reactions can be treated with rest and NSAIDs. More severe reactions with nerve function impairment (sensory or motor) and ENL are treated with prednisolone. The dose and duration of prednisolone required to manage type 1 reactions are often underestimated: doses of at least 1 mg/kg are required at commencement of therapy, tapered over six to nine months. ENL has a tendency to recur, so prednisolone courses are weaned more rapidly. Managing complications associated with prednisolone use is essential and often challenging due to the long duration of therapy required. Prophylaxis for chronic hepatitis B may be required if corticosteroid therapy is indicated.
ENL that is resistant to corticosteroid therapy, particularly if chronic or recurrent in nature, often requires thalidomide (prescribed under highly restricted guidelines because of the well-known risk of teratogenicity).
Prevention
Prevention of M. leprae infection is an ongoing global challenge. Current preventive measures are based primarily around early case detection and adequate treatment, as well as contact tracing and health education. Patients are rendered noninfectious rapidly with drug therapy so isolation is not necessary.
Guidelines for contact tracing vary, but it is generally accepted that this should include all household members (>6 months’ duration), with a single clinical examination at baseline for contacts of paucibacillary cases and with annual examination for at least six years for contacts of multibacillary cases.
Bacille Calmette–Guérin (BCG) vaccine provides some protection against M. leprae, with vaccination policies varying by state and territory. Research into the efficacy, safety and feasibility of using rifampicin with or without BCG vaccine for post-exposure prophylaxis is currently in progress, with no clear guidelines yet available.11
Conclusion
Despite a dramatic fall in prevalence and the ready availability of curative therapy, leprosy remains the leading cause of infectious disability worldwide and continues to ignite fear and stigma in society. GPs play a crucial role in diagnosis, which is primarily clinical and often extremely challenging, and in management as part of a multidisciplinary team. A summary is presented in Box 3.
Leprosy must not become a forgotten disease in Australia, as awareness among health professionals is an essential tool in reducing the burden of disease and, one day, reaching the goal of worldwide disease elimination. MT
COMPETING INTERESTS: None.
References
- World Health Assembly. Elimination of leprosy: Resolution 44.9, 13 May 1991. Handbook of resolutions and decisions of the World Health Assembly and the Executive Board. Vol III, 3rd ed. Geneva: WHO; 1993.
- World Health Organization. Global leprosy update, 2015: time for action, accountability and inclusion. Wkly Epidemiol Rec 2016; 91: 405-420. Available online at: http://apps.who.int/iris/bitstream/10665/249601/1/WER9135.pdf (accessed April 2017).
- Toms C. Surveillance report: leprosy in Australia, 1995-2014. Australian Government Department of Health; 2015 [unpublished].
- Scollard DM, Adams LB, Gillis TP, Krahenbuhl JL, Truman RW, Williams DL. The continuing challenges of leprosy. Clin Microbiol Rev 2006; 19: 338-381.
- Bratschi MW, Steinmann P, Wickenden A, Gillis TP. Current knowledge on Mycobacterium leprae transmission: a systematic literature review. Lepr Rev 2014; 86: 142-155.
- Ridley DS, Jopling WH. A classification of leprosy for research purposes. Lepr Rev 1962; 33: 119-128.
- Martinez AN, Talhari C, Moraes MO, Talhari S.PCR-based techniques for leprosy diagnosis: from the laboratory to the clinic. PLoS Negl Trop Dis 2014; 8: e2655.
- World Health Organization. Global strategy forfurther reducing the leprosy burden and sustaining leprosy control activities (2006-2010). Operational guidelines. New Delhi: WHO Regional Office for South-East Asia; 2006. Available online at: http://www.who.int/lep/resources/SEAGLP20062.pdf (accessed April 2017).
- Health Resources and Services Administration, USA. National Hansen’s Disease (Leprosy) Program. Available online at: https://www.hrsa.gov/hansensdisease/diagnosis/recommendedtreatment.html (accessed April 2017).
- Guidelines for the control of leprosy in the Northern Territory. 3rd ed. Darwin: Centre for Disease Control, Department of Health and Families, Northern Territory Government; 2010. Available online at: http://digital library.health.nt.gov.au/prodjspui/handle/10137/526 (accessed April 2017).
- Barth-Jaeggi T, Steinmann P, Mieras L, et al; LPEP Study Group. Leprosy Post-exposure Prophylaxis (LPEP) programme: study protocol for evaluating the feasibility and impact on case detection rates of contact tracing and single dose rifampicin. BMJ Open 2016; 6: e013633. Available online at: http://bmjopen.bmj.com/content/bmjopen/6/11/e013633.full.pdf (accessed April 2017).