Peer Reviewed
Feature Article Gastroenterology
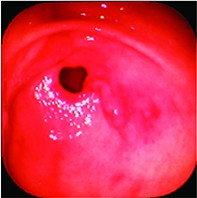
Towards a diagnosis of functional dyspepsia
Abstract
Which patients with dyspepsia should be tested for Helicobacter pylori infection, given a trial of acid suppression or have endoscopy performed, and how is functional dyspepsia diagnosed?
Key Points
- Functional dyspepsia is characterised by a history of at least three months of chronic dyspeptic symptoms in the absence of any relevant organic disease.
- Individual dyspeptic symptoms or groups of symptoms cannot be used to help distinguish organic dyspesia (ie. that caused by chronic peptic ulcer disease, gastro-oesophageal reflux or malignancy) from functional dyspepsia. Therefore it is often difficult to distinguish between these conditions without investigations.
- Empirical therapy for dyspepsia involves testing for Helicobacter pylori and treating if infected, followed by acid suppression with a proton pump inhibitor (PPI) if symptoms remain, or if negative for H. pylori, a trial of PPI therapy.
- Endoscopy should be performed before H. pylori testing and treatment in patients with new symptoms who are older than 55 years or who have alarm symptoms.
- If acid suppression fails in a patient in whom H. pylori has been excluded or eradicated, the symptoms and diagnosis should be reappraised. Prokinetics, antidepressants, psychological therapies or complementary therapies may be helpful.
- Alarm features (red flags) for upper gastrointestinal malignancy include onset of dyspepsia at an older age (over 55 years), a family history of upper gastrointestinal cancer or symptoms such as unexplained weight loss, recurrent vomiting or progressive dysphagia.
Purchase the PDF version of this article
Already a subscriber? Login here.