Peer Reviewed
Gastroenterology clinic
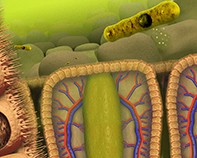
Clostridium difficile diarrhoea: a side effect of health care
Abstract
Clostridium difficile is the most common bacterial cause of antibiotic-associated diarrhoea. Treatment with metronidazole is usually successful, but recurrence is common. A range of treatment options exist for recurrence, from antibiotics to faecal microbial transplantation.
Key Points
- Depending on the antibiotic, between 5 and 25% of patients prescribed a course of antibiotics will experience diarrhoea. Clostridium difficile is the most commonly identified bacterial cause, accounting for 10 to 20% of cases. Severe C.difficile infection can lead to toxic megacolon, perforation and death through enterotoxin-mediated inflammation.
- Rates of C. difficile colonisation range from 5% in healthy adults up to 50% in healthcare workers, nursing home residents and hospitalised patients.
- C. difficile-associated diarrhoea (CDAD) generally requires a disturbance of the faecal microbiota (most commonly caused by antibiotic use) and colonisation through the faecal–oral route. C. difficile spores are detectable on the hands, stethoscopes and clothing of healthcare workers and can persist for months on objects such as toilets and other hospital furnishings.
Remember
Picture credit: © Carol and Mike Wener/Science Source/Diomedia.com
Purchase the PDF version of this article
Already a subscriber? Login here.