Anticoagulation – extended treatment for venous thromboembolism
Indefinite anticoagulation with direct oral anticoagulants (DOACs) is increasingly being recommended after symptomatic venous thromboembolism (VTE) in many clinical scenarios. This is because of the ease of use and lower bleeding risk of DOACs compared with warfarin and cumulative evidence of recurrence risk if anticoagulants are stopped, particularly after unprovoked VTE. The decision for extended use should be tailored to each patient, based on the risk of recurrence and bleeding, and patient preference.
- Patients with symptomatic venous thromboembolism (VTE) associated with a major provoking factor can usually stop anticoagulation after three to six months.
- Patients with a persisting provoking factor, including malignancy or antiphospholipid syndrome, and those with recurrent unprovoked VTE should receive anticoagulation indefinitely.
- The decision to extend anticoagulation beyond three to six months among those with first unprovoked or minimally provoked VTE is nuanced, and based on the individual’s recurrence and bleeding risk and patient preference.
- Radiological findings at the end of the treatment phase of anticoagulation (three to six months) should not dictate duration of anticoagulation but are useful to establish a new baseline.
- Monitoring patients on extended anticoagulation should include six- to 12-monthly assessment of renal and liver function, bleeding risk and new medications.
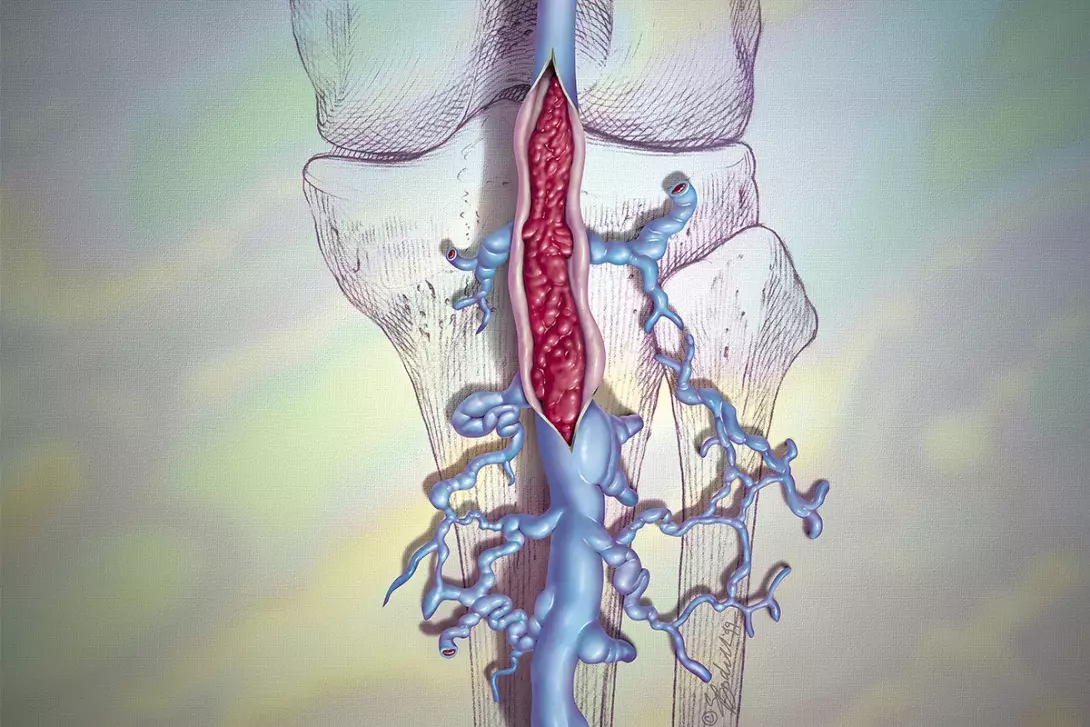
A key decision in the management of patients with venous thromboembolism (VTE) is determining the optimal duration of anticoagulation therapy. The advent of direct oral anticoagulants (DOACs), particularly low-dose formulations, which have a lower bleeding risk than vitamin K antagonists (VKAs), has led to a lower threshold for continuing anticoagulation beyond three to six months in those deemed at high risk of recurrence if anticoagulation is ceased. Although the decision in some situations is clear, such as continuation in patients with cancer-associated thrombosis (CAT) or antiphospholipid syndrome (APLS), or cessation in those whose thrombosis was clearly provoked, many scenarios are much less straightforward. This review discusses the background and evidence for extended treatment for deep vein thrombosis (DVT) and pulmonary emboli (PE) and provides guidance on identifying patients who may benefit from extended-duration anticoagulation, choice of anticoagulant and how these patients should be monitored.
How long should anticoagulants be continued in patients with VTE?
Most patients with VTE require three months of anticoagulation therapy, at which point a decision regarding cessation or continuation needs to be made.1 VTE recurrence risk differs markedly depending on the type of provocation; therefore, establishing if a DVT or PE was transiently or persistently provoked, minimally provoked or unprovoked is key to deciding whether anticoagulants should be continued or stopped after the initial treatment phase (Table 1).2 The Flowchart summarises the duration of therapy recommended for these different scenarios.3,4 In situations where there is equipoise, such as a first unprovoked or minimally provoked VTE (as will be discussed), patient involvement is crucial to gauge their preference based on risks, and to maintain adherence.5
Distal DVT
Distal DVT is defined as thrombosis distal to, and not including, the popliteal vein and uncertainty exists about the value of anticoagulation in its treatment.3,6 Isolated distal DVTs may have a low rate of recurrent VTE or proximal propagation.7 In patients with a high bleeding risk, forgoing anticoagulation and instead monitoring with serial weekly ultrasounds to assess for proximal extension is recommended, particularly if the patient is asymptomatic.8 If the decision is made to treat with anticoagulation, international guidelines recommend anticoagulation therapy for six to 12 weeks; however, recent evidence suggests a shorter duration can be safe and effective. The TWISTER trial (Two Weeks of Low Molecular Weight Heparin for Isolated Symptomatic Distal Vein Thrombosis) showed that two weeks of anticoagulation therapy was sufficient for patients with no persisting symptoms and no extension of thrombus on ultrasound at two weeks.7 In those with persisting symptoms or thrombus extension after two weeks of anticoagulation, treatment should be continued for a further four weeks to complete six weeks in total. The recurrence risk after stopping anticoagulation in this scenario is low, and most patients with a distal DVT do not need extended anticoagulation.1
Provoked PE or proximal DVT
Anticoagulation therapy for three months is usually sufficient for those with a proximal DVT (i.e. involving the popliteal or more proximal deep vein) or PE provoked by a major reversible risk factor. Extending treatment to six months can be considered in those with a very large initial DVT or PE (e.g. a PE associated with right ventricular dysfunction), or when symptoms are persistent.
As shown in Table 2, patients with a VTE associated with a minor or nonsurgical reversible risk factor have a higher recurrence risk than those with a VTE provoked by a major risk factor.2,3 Most of these patients may also stop anticoagulation therapy after the initial three- to six-month treatment phase. However, in those with very borderline provocation (such as onset following prolonged car travel) and low bleeding risk, anticoagulants may be extended beyond six months with annual review after discussion of recurrence risk and in line with patient preference.4,5
Persistent provoking factor
Patients with a persistent provoking factor, such as cancer, APLS or inflammatory bowel disease, should continue anticoagulation therapy indefinitely. Most cases of CAT require at least six months of full-intensity anticoagulation, even if the initial VTE is an incidental finding or the patient is asymptomatic. A recent systematic review found that recurrence beyond six months is common after anticoagulation cessation, and that continuation of anticoagulation therapy has an acceptable safety profile and, therefore, extended duration anticoagulation therapy is recommended in patients with active cancer..9,10 Patients with cancer need close monitoring as they have a higher bleeding risk than those on anticoagulation therapy without cancer.11
Unprovoked VTE
Individuals with a first unprovoked VTE are at a high risk of recurrence (Table 2).2,3 Continuing anticoagulation therapy beyond the first three- to six-month treatment phase reduces the risk of recurrence by about 90% in these patients compared with stopping anticoagulation therapy.12,13 It is important to understand that the benefit of reduced risk of recurrence is only attained while patients receive anticoagulation, and is not maintained once discontinued – i.e. the risk of recurrence returns to baseline levels once anticoagulation is stopped.14,15
Those with two or more unprovoked episodes of VTE should continue anticoagulation therapy indefinitely. A decision on duration of anticoagulation therapy is more difficult after a first unprovoked event. For each patient, the benefits in reducing recurrence risk need to be weighed against the bleeding risk associated with continuing therapy. The risk of major bleeding with DOACs is low (about 1% per patient-year) compared with about 4% per patient-year for warfarin.12,16,17 Men with a first unprovoked event should be encouraged to continue anticoagulants indefinitely as their baseline recurrence risk is higher than for women (Table 3).18-21 Women with a first unprovoked event are in a situation of clinical equipoise for continuing therapy; continuation of anticoagulation is reasonable if the bleeding risk is low and it is the patient’s preference. The presence of moderate to severe post-thrombotic syndrome, a form of chronic venous insufficiency occurring after (usually) extensive proximal DVT, may sway the decision towards indefinite anticoagulation.22 Those who stop anticoagulation therapy should be carefully educated on the signs and symptoms of recurrence and advised to seek medical attention urgently if they occur.
Estimating recurrence risk
Clinical prediction tools can be used to estimate recurrence risks after stopping anticoagulation in those with unprovoked VTE. The most widely used tools include the HERDOO2 rule (hyperpigmentation, oedema, or redness in either leg; D-dimer level ≥250 mcg/L; obesity with body mass index ≥30 kg/m2; or older age, ≥65 years), the Vienna prediction model and DASH (D-dimer, age, sex, hormonal therapy) (Table 3). These prediction tools may help identify those at highest risk of recurrence based on clinical variables, particularly women with first unprovoked VTE where there is clinical equipoise, and allow a decision on extending anticoagulation to be tailored accordingly.21
Assessing bleeding risk
Bleeding risk assessment is an important factor in the decision to continue anticoagulation for an extended period.3 The strongest predictor for bleeding during anticoagulation therapy is the presence of bleeding over the preceding three to six months.23 Other predictors include severe renal impairment, active cancer and the presence of a lesion that could bleed (e.g. peptic ulcer disease). However, the overall risk of major bleeding with DOACs is low (about 1% per year). The risk of bleeding with ‘prophylactic’ doses of apixaban (2.5 mg twice daily) and rivaroxaban (10 mg daily) has been shown to be similar to the risk in patients who are not taking anticoagulants, although the short 12-month follow up in this trial should be noted.24
When to refer to a haematologist
It is the authors’ opinion and practice that all patients with unprovoked or recurrent VTE should be referred to a haematologist or physician with an interest in thrombosis. If there is doubt about the optimal duration of anticoagulation, we suggest continuing anticoagulants in those with a low bleeding risk until a haematologist opinion is sought. This enables guidance for the optimal duration of anticoagulation and allows ongoing shared care with the GP, particularly if the patient continues extended anticoagulation. These patients may also need guidance on perioperative management of anticoagulation.
Role of laboratory testing and repeat imaging
The presence or absence of an inherited thrombophilia rarely dictates decision-making on the duration of anticoagulation and, in many cases of VTE, testing is not needed. Testing for thrombophilia should be considered for those with an unprovoked VTE at a young age (<50 years), a strong family history for VTE or VTE at an unusual site.25 Those with a ‘strong’ thrombophilia, such as the rare antithrombin deficiency, or protein C or S deficiency with a family history, are more likely to need indefinite anticoagulation. We strongly discourage thrombophilia testing in those with a clearly provoked event as, regardless of the result, a fixed duration of anticoagulation is likely appropriate.
It is usually clinical context of the VTE rather than the thrombophilia that drives decisions about the duration of anticoagulation.25 Even among patients with unprovoked VTE, the risk of recurrent VTE is similar regardless of the presence or absence of thrombophilia.26 The caveat is APLS, the presence of which alters decisions regarding duration of therapy (indefinite) and choice of anticoagulant (warfarin), and should be tested for in individuals of any age with unprovoked VTE.25
D-dimer is a fibrin degradation product released when cross-linked fibrin is cleaved by plasmin. It may be used as an adjunct to clinical predictors to assess recurrence risk and is used in some clinical prediction tools (Table 3). A positive D-dimer test result 30 days after cessation of anticoagulation (which the patient had received for three months) for an unprovoked VTE is associated with a higher risk of recurrent VTE (15%) than a normal D-dimer test result (6.2%).13 Although even those with a normal D-dimer test result have an elevated recurrence risk, D-dimer testing may be useful in situations of clinical equipoise, such as after a first unprovoked VTE, particularly in women.6
Imaging at the end of the initial three- to six-month treatment period is performed to establish a new baseline for the patient and is most useful in those who stop anticoagulation. Residual vein occlusion or thrombosis is common – up to 50% of individuals have residual chronic thrombosis after acute PE or DVT.27-29 Although evidence is conflicting and there may be a modestly increased recurrence risk, the utility of residual occlusion to predict recurrence is minimal and repeat imaging should generally not be used to guide decision-making about the duration of anticoagulation.21
Choice of anticoagulant for different patient groups
DOACs are first-line agents for both acute and extended treatment of VTE as they are well-tolerated, have predictable pharmacokinetics, few food and drug interactions and a lower bleeding risk than VKAs.3 After the initial three- to six-month therapeutic anticoagulation treatment period, dose reduction to a ‘prophylaxis’ dose (i.e. apixaban 2.5 mg twice daily or rivaroxaban 10 mg daily) may be considered. These doses have been shown to be as efficacious as the ‘full dose’ (rivaroxaban 20 mg daily or apixaban 5 mg twice daily) but are associated with a lower risk of nonmajor bleeding.16,24 Empirically, our practice is to continue the full dose in individuals with obesity, and those who have had recurrent VTE, have a high-risk thrombophilia such as antithrombin deficiency and who have had a breakthrough thrombosis while on a low-dose DOAC.16,24 Alternative agents (i.e. warfarin or low molecular weight heparin) should be considered in the following scenarios.
- In patients with APLS. VKAs remain standard of care in these patients, particularly those with a triple positive antiphospholipid antibody profile (anticardiolipin, beta-2-glycoprotein and lupus anticoagulant positive). Recent randomised trials show a higher rate of ischaemic stroke in patients with APLS treated with rivaroxaban or apixaban compared with those treated with VKAs, and DOACs should be avoided in this context.30,31
- In those with morbid obesity. Initial clinical trials of DOACs excluded those weighing more than 120 kg, and there have been concerns about the efficacy of DOACs in the obese population. However, real-world phase 4 data on use of DOACs in people with obesity have shown both rivaroxaban and apixaban to be adequate in treating VTE regardless of body weight and body mass index, with the acknowledgement there is no data for dose reduction to prophylaxis dose.32
- In patients with CAT. DOACs are now considered first-line therapy for CAT after the pivotal CARAVAGGIO and SELECT-D trials showed them to have efficacy on par with dalteparin.33,34 Low molecular weight heparins remain the preferred treatment option in those with unresected luminal gastrointestinal or genitourinary cancers as DOACs have a higher bleeding risk.10 Drug-drug interactions, thrombocytopenia and absorption are also important factors to consider in therapy selection for CAT treatment.
- After bariatric surgery, because of variable absorption.
- For patients receiving certain medications such as azoles, antiretrovirals and some antiepileptics because of drug-drug interactions.6,32
- In patients with severe renal or hepatic impairment.
Before the advent of DOACs, aspirin was often recommended for VTE after the initial three- to six-month treatment period.35 Evidence shows reduced-dose DOACs have similar bleeding risks to aspirin but with a 70% lower recurrence of VTE; therefore, aspirin is no longer recommended as an alternative to extended anticoagulation.16 Despite this, the recently updated American College of Chest Physicians (CHEST) guidelines suggested using aspirin over no therapy in patients deemed suitable for extended anticoagulation but who decide to stop anticoagulants. This recommendation is questionable and puts patients at risk of bleeding without having any benefit over DOACs, except perhaps being lower cost.6
Monitoring a patient on long-term anticoagulation
Patients on extended anticoagulation for VTE should be reviewed at least yearly to ensure the benefits of continuing anticoagulation continue to outweigh risks (i.e. bleeding) and assess new medications for drug-drug interactions and renal and liver function. Even if the initial decision had been made to anticoagulate indefinitely, treatment may subsequently be stopped if the risk of bleeding increases, such as the development of a new bleeding event or new renal or hepatic impairment. If anticoagulation is stopped, it is important to educate patients on the risks, symptoms and signs of recurrent VTE and instruct them to seek medical attention urgently if these occur.
Conclusion
Due to the relative safety of DOACs and growing evidence regarding risk of recurrent VTE following anticoagulant cessation, it is increasingly being recommended that anticoagulation therapy be continued for extended periods. In some clinical situations, the decision to time limit (e.g. isolated distal DVT, VTE with major provocation) or extend (e.g. cancer, APLS, recurrent unprovoked VTE) anticoagulation is clear. For patients with a first unprovoked or minimally provoked VTE, an individualised approach to anticoagulation duration is needed, with the decision to stop or extend treatment being based on recurrence and bleeding risk. MT
