The rise of egg freezing

As elective oocyte cryopreservation becomes more mainstream, women seeking this procedure are likely to present to their GPs first. GPs have the opportunity to educate their patients about fertility, counter false beliefs and undertake initial assessments.
Formerly considered an experimental procedure, oocyte cryopreservation entered mainstream medicine in 2012, when the American Society for Reproductive Medicine removed the experimental label. In 2019, Australian experts agreed, stating that one in six women and couples in Australia experience infertility, with a rising proportion of cases related to advanced maternal age; this is associated with poorer oocyte quality and outcomes of in vitro fertilisation (IVF).1 Internationally, IVF treatment using cryopreserved oocytes from women aged under 35 years provides similar live-birth outcomes to IVF treatment using fresh oocytes.1
According to the Victorian Assisted Reproductive Treatment Authority, 4048 women had eggs in storage in Victoria at the end of 2019-2020, compared with 3124 women the previous year – a 30% increase.2 They include women facing fertility-threatening medical treatment, such as some cancer therapy, those not in a position to have a child during their most fertile years for personal reasons and those at risk of premature menopause or with endometriosis. However, the use of frozen eggs to conceive is still uncommon. In 2018-2019, fewer than 1% of all IVF cycles involved thawed eggs, and 34 babies were born to women who used their own thawed eggs.2
Reasons behind the trend for women to undertake egg freezing likely include the improved success rates of oocyte cryopreservation and social and mainstream media reports. Many celebrities have openly discussed their decision to undertake elective egg freezing, and others such as Jennifer Aniston have expressed regret that they did not do so.3,4 We also hope that women are gaining a better understanding of their own fertility and an appreciation that IVF is not a panacea for the age-related decline in fertility.
The first stop for most women pursuing elective egg freezing will be their GP. Misconceptions about fertility, ovarian reserve testing and the promise of egg freezing abound. For example, women may request anti-Müllerian hormone (AMH) testing to ‘check their fertility’. GPs have the best opportunity to educate their patients about future fertility and to counter false beliefs through counselling.
This article discusses the rationale and process of elective oocyte cryopreservation. It also outlines a suggested approach for GPs to patients who request elective egg freezing.
Why freeze eggs?
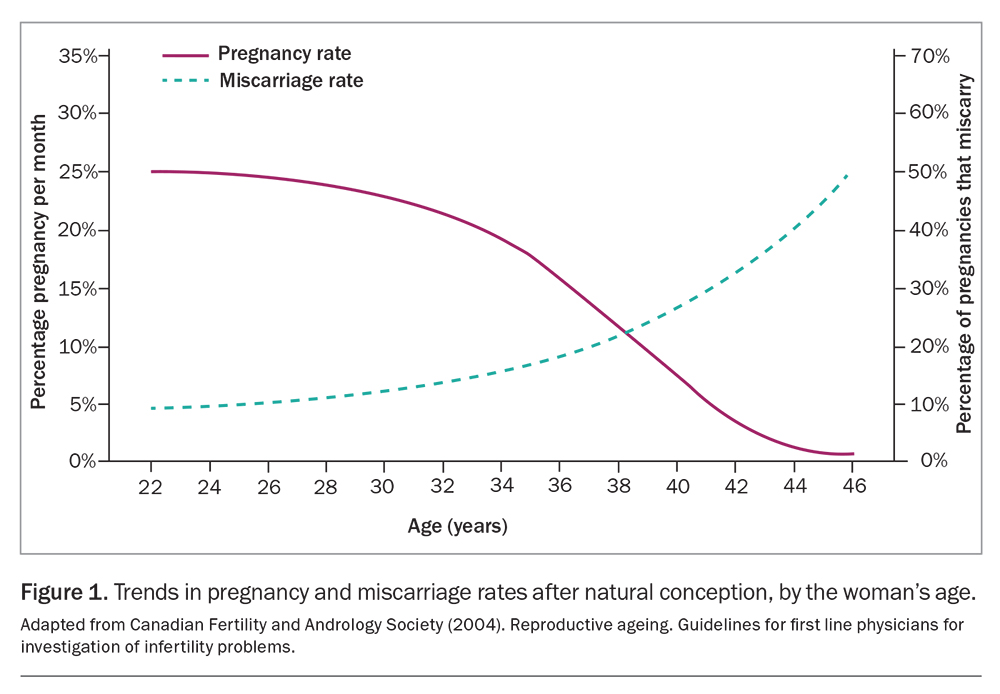
From a fertility perspective, everything becomes more difficult as women age: it is more difficult to get pregnant and more difficult to stay pregnant, with an increasing risk of miscarriage (Figure 1). Women are born with about two million oocytes, which declines initially through atresia to 300,000 by puberty. The number is down to 30,000 by age 35 years and to around 1000 by age 51 years.5 The decline in number of oocytes is accompanied by a decrease in their quality, primarily through increasing rates of aneuploidy.6
Elective oocyte cryopreservation is a strategy to improve a woman’s longitudinal fertility potential with her own oocytes in the absence of a medical diagnosis of infertility or a contraindication to pregnancy. This option affords women the opportunity to conceive a biological child at a later age.7,8
Assessing ovarian reserve
Assessment of ovarian reserve (egg quantity) helps in decision-making around egg freezing as well as in managing expectations about the likelihood of success. As yet, there are no biomarkers of egg quality.
Ovarian reserve assessment methods
Ovarian reserve (number of remaining oocytes) can be assessed by two methods:
- a blood test to measure AMH level
- ultrasound imaging of the ovaries to assess the antral follicle count (AFC).9
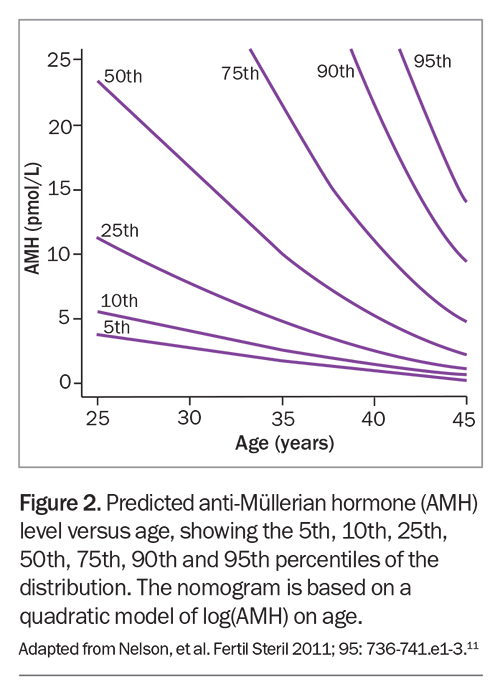
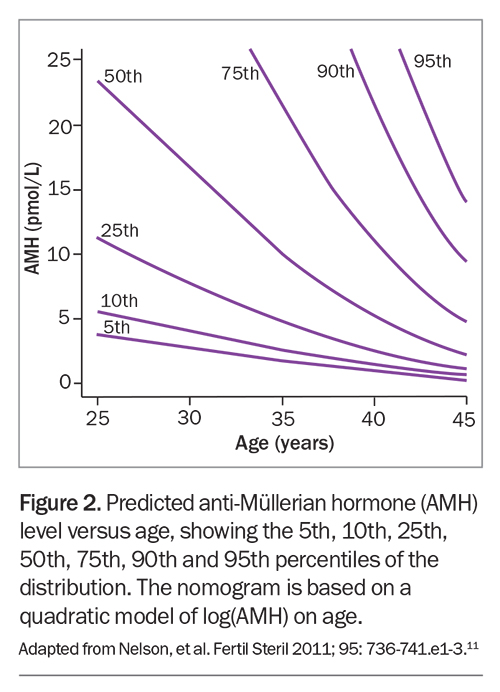
AMH is produced by the granulosa cells of primary, pre-antral and antral follicles. It acts by two mechanisms: inhibiting initial follicle recruitment from the resting pool of primordial follicles; and inhibiting the sensitivity of antral follicles to follicle- stimulating hormone (FSH). Overall, the role of AMH is to prevent premature depletion of the follicle pool.10 AMH level thus reflects the number of remaining oocytes and decreases with the age-related decline in follicle numbers (Figure 2).11
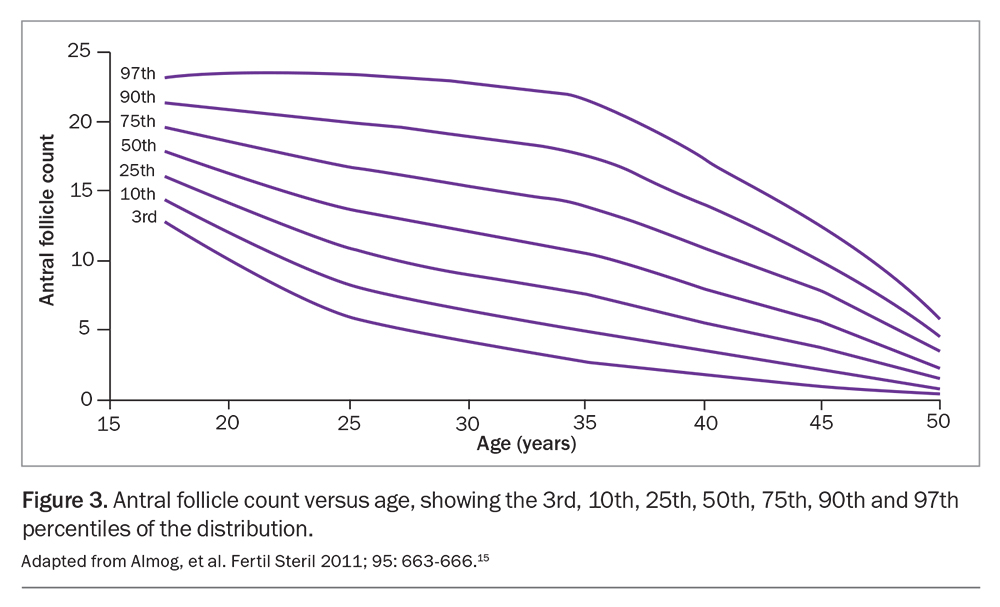
The AFC is the sum of antral follicles across both ovaries determined by a transvaginal ultrasound examination. Typically, antral follicles are measured at a diameter of 2 to 10 mm in the early follicular phase of the menstrual cycle, between days 5 and 9.12
Limitations of ovarian reserve measurements
Although AMH and AFC are markers of egg quantity, they do not reflect oocyte quality or predict the chance of conception or of having a live birth.
AMH is reasonably correlated with a patient’s potential response to hormonal stimulation. It is helpful to estimate egg numbers and to guide dosing in artificial reproductive technology.13 A challenge with interpretation of the AMH level is the high inter- and intra-individual variability, regardless of the type of assay (Figure 2).11
The use of hormonal contraception can also influence AMH levels. A cross-sectional study analysing different forms of contraceptive and AMH levels in women of reproductive age found a statistically significant decrease in AMH level with the combined oral contraceptive pill (24%), contraceptive implant (23%), vaginal ring (22%), progestin-only pill (15%) and hormonal intrauterine device (7%).14
The AFC can vary between individuals because of the natural variability in the number of antral follicles among women of the same age group (Figure 3).15 In addition, interobserver reliability when assessing AFC depends on the experience of the centre where the scan is performed.13
Ovarian stimulation and egg collection
For the oocyte cryopreservation process, the ovaries are stimulated with injections of gonadotrophins for about 10 to 12 days to recruit multiple dominant follicles. Premature spontaneous ovulation is prevented with injections of a gonadotrophin-releasing hormone (GnRH) antagonist or, increasingly, oral progestogens. When the leading follicle reaches a diameter of 17 to 19 mm, an ovulation trigger is administered 36 hours before oocyte retrieval. The latter is accomplished using a transvaginal approach under ultrasound guidance.
The main risk associated with ovarian stimulation is ovarian hyperstimulation syndrome (OHSS). OHSS is an exaggerated response of the ovaries to human chorionic gonadotrophin (hCG), leading to the release of proinflammatory mediators such as vascular endothelial growth factor and subsequent vascular permeability. The latter results in loss of fluid into the third space, which manifests as ascites, pleural and pericardial effusions. Given the advances in reproductive technology, such as adoption of an antagonist protocol and agonist trigger rather than hCG, these side effects are rarely seen.
The process of oocyte retrieval is also associated with surgical risks. These include limited vaginal haemorrhage from the puncture site (8%), infection (0.3 to 0.6%), and, rarely, acute haemorrhage from the ovary or haematoma secondary to uterine, ovarian or iliac vessel injury (0.04 to 0.07%).16-19
Success of egg freezing
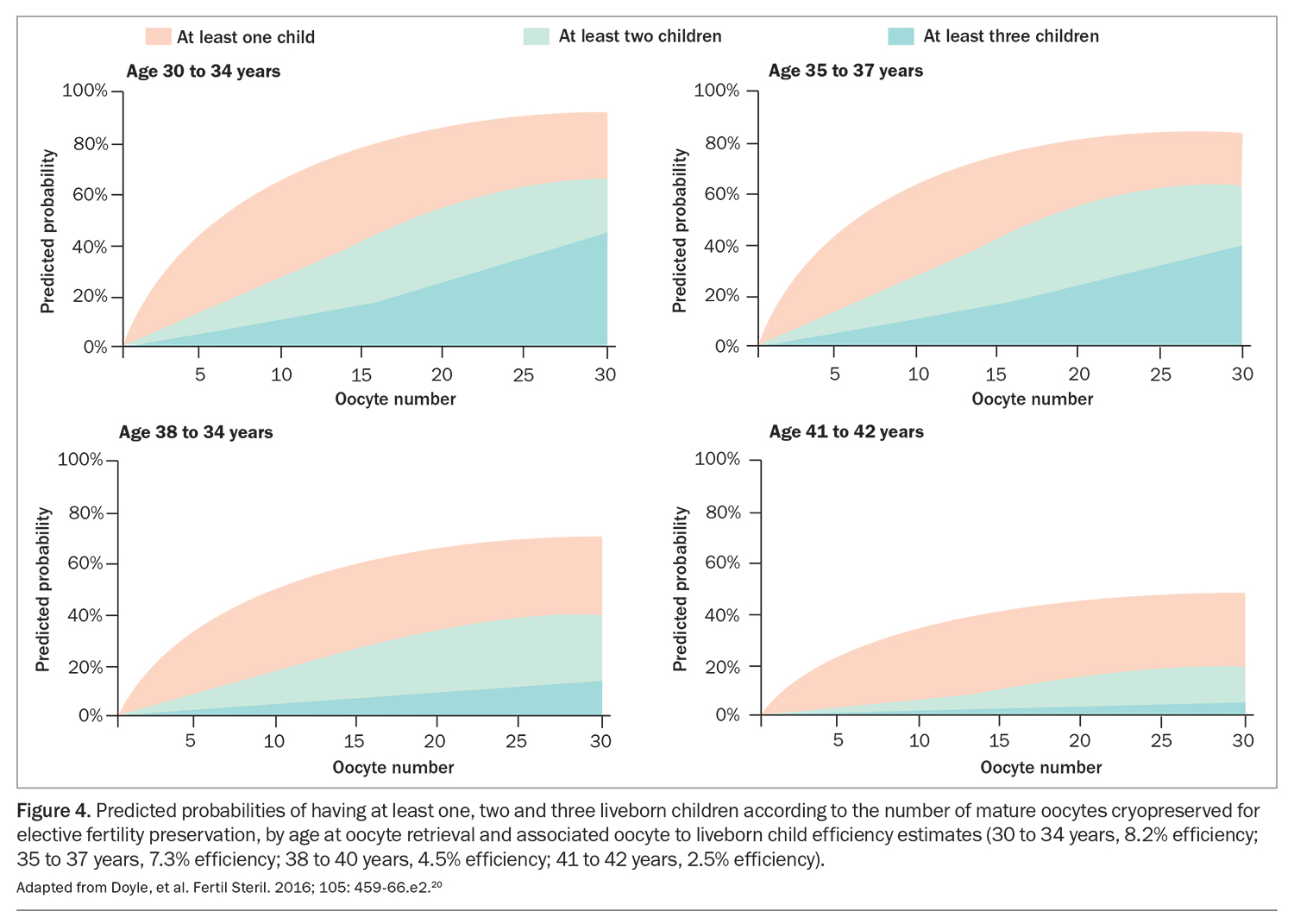
The primary goal of ovarian stimulation is to obtain the maximum number of oocytes that will enable the best chance of achieving a live birth while minimising the risk of side effects. The live birth rate is determined by the patient’s age and egg quality at the time of freezing. The success rate correlates with the age and number of eggs.1
As it is not possible to conduct a randomised controlled trial, we rely on modelling to inform patients about expected success (Figure 4).20 Just as IVF is not a reliable back-up plan for age-related infertility, neither is egg freezing. At some point, artificial intelligence may be able to predict the potential of frozen eggs; however, at present, women will not know the outcome of their frozen eggs until they use them, which to date only 10 to 12% have done.1
Psychosocial aspects
The decision to undertake egg freezing involves complex emotions, ranging from feeling empowered about increased control of one’s reproductive journey to anxiety and concern about the procedure itself.21 Patients may also reflect on their decision after the procedure regarding future parenthood, impact on relationships, and need to re-evaluate personal goals, desires and expectations.22,23
The cost of oocyte retrieval and cryopreservation varies widely, depending on the clinic and factors such as anaesthetist and theatre fees. There is no Medicare rebate for elective egg freezing.
GP work up
For patients who ask about elective egg freezing, clinicians should explore the rationale for considering this procedure, offer appropriate counselling and evaluate ovarian reserve. A comprehensive assessment should also be undertaken, including history taking to assess for reproductive risk factors, systemic health conditions and relevant family history. Optimising pre-existing medical conditions, reinforcing positive lifestyle habits and performing a wellbeing check for up-to-date cervical screening and vaccinations at the initial assessment is ideal. If the woman is in a relationship, preconception carrier screening should be discussed.
As discussed above, AMH measurement is a simple blood test to assess ovarian reserve that can be carried out at any point in a woman’s menstrual cycle. However, if the AMH level is found to be unexpectedly low, ultrasound assessment of AFC in the early follicular phase may be a useful adjunct to gauge a woman’s ovarian reserve. Women should be advised that the AMH level is not a measure of current or future fertility, even if it is low.24,25
How far a GP goes in evaluating the patient before referral to an IVF specialist depends on their scope of practice. At a minimum, specialists would like an AMH result so they can adequately counsel patients about expectations.
Conclusion
The increase in women seeking elective oocyte cryopreservation has gained significant momentum over recent years. Empowerment over one’s reproductive journey is a powerful tool and cannot be underestimated. However, as clinicians, it is our duty of care to provide unbiased, objective and realistic discussions about the process of oocyte cryopreservation. MT
COMPETING INTERESTS: Dr Lieberman is a consultant and speaker for Besins, Ferring, Merck and Organon; and a shareholder in City Fertility. Dr Arulpragasam: None.
References
1. Lew R, Foo J, Kroon B, Boothroyd C, Chapman M; Australian CREI Consensus Expert Panel on Trial evidence (ACCEPT) group. ANZSREI consensus statement of elective oocyte cryopreservation. Aust N Z J Obstet Gynaecol 2019; 59: 616-626.
2. Victorian Assisted Reproductive Treatment Authority. Fertility treatment. Preserving fertility. Available online at: https://www.varta.org.au/fertility-treatment/preserving-fertility (accessed August 2023).
3. Harvey-Jenner C. 13 celebrities who have frozen their eggs for fertility reasons. Cosmopolitan 2020; Oct 1. Available online at: https://www.cosmopolitan.com/uk/body/a34218729/celebrities-freezing-eggs-fertility/ (accessed August 2023).
4. Siegel E. Jennifer Aniston opens up about IVF and fertility struggles. Allure 2022; Nov 9. Available online at: https://www.allure.com/story/jennifer-aniston-ivf-fertility-struggles (accessed August 2023).
5. Wang X, Wang L, Xiang W. Mechanisms of ovarian aging in women: a review. J Ovarian Res 2023; 16: 67.
6. Vollenhoven B, Hunt S. Ovarian ageing and the impact on female fertility. F1000Res 2018; 7: F1000 Faculty Rev-1835.
7. Stern K. Elective egg freezing: offering empowerment or false hope? O & G Magazine 2015; 17(3). Available online at: https://www.ogmagazine.org.au/17/3-17/elective-egg-freezing-offering-empowerment-false-hope/ (accessed August 2023)
8. Stoop D, Nekkebroeck J, Devroey P. A survey on the intentions and attitudes towards oocyte cryopreservation for non-medical reasons among women of reproductive age. Hum Reprod 2011; 26: 655-661.
9. Copp T, Nickel B, Lensen S, et al. Anti-Mullerian hormone (AMH) test information on Australian and New Zealand fertility clinic websites: a content analysis. BMJ Open 2021; 11: e046927.
10. Weenen C, Laven J, Von Bergh A, et al. Anti Müllerian hormone expression pattern in the human ovary: potential implications for initial and cyclic follicle recruitment. Mol Hum Reprod 2004; 10: 77-83.
11. Nelson SM, Messow MC, Wallace AM, Fleming R, McConnachie A. Nomogram for the decline in serum antimüllerian hormone: a population study of 9,601 infertility patients. Fertil Steril 2011; 95: 736-741.e1-3.
12. Deb S, Jayaprakasan K, Campbell BK, Clewes JS, Johnson IR, Raine-Fenning NJ. Intraobserver and interobserver reliability of automated antral follicle counts made using three-dimensional ultrasound and SonoAVC. Ultrasound Obstet Gynecol 2009; 33: 477-483.
13. Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril 2020; 114: 1151-1157.
14. Hariton E, Shirazi TN, Douglas NC, Hershlag A, Briggs SF. Anti-Müllerian hormone levels among contraceptive users: evidence from a cross-sectional cohort of 27,125 individuals. Am J Obstet Gynecol 2021; 225: 515.e1-515.e10.
15. Almog B, Shehata F, Shalom-Paz E, Tan SL, Tulandi T. Age-related normogram for antral follicle count: McGill reference guide. Fertil Steril 2011; 95: 663-666.
16. Practice Committee of Society for Assisted Reproductive Technology; Practice Committee of American Society for Reproductive Medicine. Essential elements of informed consent for elective oocyte cryopreservation: a Practice Committee opinion. Fertil Steril. 2008; 90(5 Suppl): S134-S135.
17. Taylor HS, Pal L, Seli E. Oocyte retrieval. In: Speroff’s clinical gynecologic endocrinology and infertility. 9th ed. Lippincott Williams and Wilkins; 2019: 2936-2937.
18. Royal College of Obstetricians and Gynaecologists. The management of ovarian hyperstimulation syndrome. Green-top guideline no. 5. 3rd ed. London: RCOG; 2016. Available online at: https://www.rcog.org.uk/media/or1jqxbf/gtg_5_ohss.pdf (accessed August 2023).
19. Mourad S, Brown J, Farquhar C. Interventions for the prevention of OHSS in ART cycles: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017; 1(1): CD012103.
20. Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016; 105: 459-66.e2.
21. Petropanagos A. Reproductive ‘choice’ and egg freezing. Cancer Treat Res 2010; 156: 223-235.
22. Polyakov A, Piskopos J, Rozen G. Elective egg freezing: State of the ART. Aust J Gen Pract 2023; 52: 20-23.
23. Caughey LE, White KM. Psychosocial determinants of women’s intentions and willingness to freeze their eggs. Fertil Steril 2021; 115: 742-752.
24. Slater A, Lew R, Peate M. Age-related fertility decline and elective oocyte cryopreservation: knowledge, attitudes and practices in a pilot study of general practitioners. Aust J Gen Pract 2022; 51: 611-619.
25. Dalton A, Koch J. A patient asks about her reproductive potential: when and how should I recommend oocyte cryopreservation? O & G Magazine 2019; 21(4). Available online at: https://www.ogmagazine.org.au/21/4-21/qa-ocyte-cryopreservation/ (accessed August 2023).