Antibiotic use may increase inflammatory bowel disease, especially in the over 40s
By Melanie Hinze
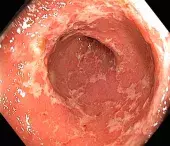
Antibiotic exposure is a risk factor for the development of inflammatory bowel disease (IBD), especially in people aged 40 years or older, research published in Gut suggests.
Researchers used Danish nationwide registries to recruit a population-based cohort of more than 6 million individuals (50.4% female) aged 10 years or older with no prior diagnosis of IBD, between the years 2000 and 2018.
Overall, 5.5 million (91%) individuals were prescribed at least one course of antibiotics between 2000 and 2018, during which time just over 36,018 new cases of ulcerative colitis and 16,881 new cases of Crohn’s disease were diagnosed.
The researchers found that antibiotic exposure was associated with an increased risk of IBD when compared with no antibiotic exposure in all age groups; however, the association was greatest in those aged 40 years and older. The association was seen for both ulcerative colitis and Crohn’s disease.
The risk of IBD increased with cumulative antibiotic exposure and with antibiotics targeting gastrointestinal pathogens, and it was most pronounced one to two years after antibiotic exposure.
Associate Professor David van der Poorten, Staff Specialist Gastroenterologist at Westmead Hospital, Sydney, and Clinical Associate Professor at The University of Sydney, said the overall risk for IBD with antibiotics in the study was small; however, the findings were in keeping with other evidence that factors that induced gut dysbiosis were related to the development of IBD.
‘A bad diet with too much processed food and emulsifiers does this and antibiotics do this too,’ he said.
Associate Professor van der Poorten said gastrospecific antibiotics were a bigger risk, particularly nitroimidazoles and fluoroquinolones (e.g. metronidazole, ciprofloxacin and norfloxacin), which target Gram-negative bacteria and anaerobes.
Associate Professor van der Poorten said the finding that older ages were more at risk was very useful information, as was the likely time gap of one to two years.
‘I see this as good news, because that means there is plenty of time to get the microbiome back to full health by some simple interventions like providing advice to eat lots of whole foods, fresh fruit and vegetables during and after the course of antibiotics.’
He said for those needing multiple courses of antibiotics or gastrointestinal antibiotics, ‘perhaps making this more formal advice with a handout including examples of prebiotics and fermented foods could be beneficial.’
‘We don't need to be alarmed about antibiotics, just aware,’ he said, adding that the findings provided a further reason to think twice about prescribing antibiotics, specifically gastrointestinal ones, if there were other alternatives.