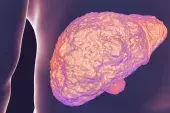
Mortality rates high despite hepatitis C cure
By Melanie Hinze
The results of a new study highlight the need for continued support and follow up of patients after successful treatment for hepatitis C to maximise the impact of direct-acting antivirals.
The population-based cohort study, published in the BMJ, involved 21,790 participants from Canada, Scotland and England, who were successfully treated for hepatitis C in the era of interferon-free antivirals (2014 to 2019). Participants were divided into three liver-disease severity groups: those without cirrhosis, those with compensated cirrhosis and those with end-stage liver disease.
Overall, 7% of participants died during follow up due to drug-related mortality (24%), liver failure (18%) and liver cancer (16%). All-cause mortality rates were significantly higher than those of the general population across all disease severity groups. The researchers found that higher mortality rates were seen in patients with recent substance misuse, alcohol misuse, older age and comorbidities.
Associate Professor Simone Strasser, Senior Staff Specialist in the AW Morrow Gastroenterology and Liver Centre and Director of Hepatology Clinical Trials at the Royal Prince Alfred Hospital, Sydney, told Medicine Today that successful treatment of hepatitis C with direct acting antiviral agents has significant benefits in terms of reducing liver-related mortality and liver-cancer development.
‘However, the data in this study demonstrate how important it is to treat people before the development of cirrhosis or end-stage liver disease, where excess mortality remains despite successful viral eradication,’ she said.
Professor Strasser, who is also Director of The Liver Foundation, said that although early treatment before the development of cirrhosis prevented liver-related mortality, drug misuse remained a significant cause of death in this population, underlining the essential role of linkage to long-term harm reduction strategies.
‘In Australia, GPs deliver the majority of treatments for hepatitis C in the community,’ she said. ‘It is therefore essential that patients with cirrhosis are identified prior to direct-acting antiviral therapy to ensure they are engaged in long-term surveillance for liver cancer after viral cure, and that patients with ongoing drug use are engaged in harm reduction to prevent drug-related deaths,’ she said.
Professor Strasser added that patients with end-stage liver disease should be under the care of liver specialists, as they remain at significant risk of liver-related mortality.
BMJ 2023; 382: e074001; http://dx.doi.org/10.1136/bmj-2022-074001.