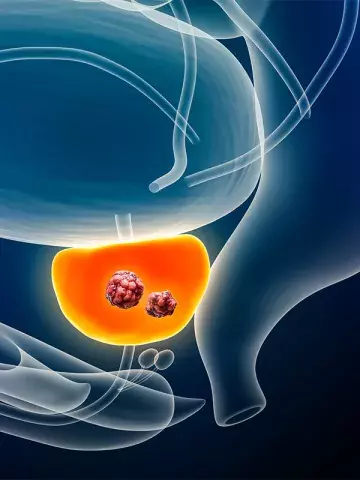
Active surveillance for prostate cancer: long-term outcomes assessed
By Melanie Hinze
Protocol-directed active surveillance (AS) is a safe management strategy for favourable-risk prostate cancer, which helps clinicians to avoid overtreatment and prevent undertreatment, according to research published recently in JAMA.
The Canary Prostate Active Surveillance Study (PASS) was a prospective cohort study initiated in the USA in 2008.
A total of 2155 men (median age 63 years) with localised prostate cancer and no prior treatment were followed for a median of 7.2 years. At diagnosis, the men had a median prostate-specific antigen (PSA) of 5.2ng/mL and 90% had been diagnosed with grade group 1 cancer. Follow up involved PSA testing every three to six months, confirmatory biopsies at six to 12 months after diagnosis and subsequent biopsies every two years.
Ten years after diagnosis, 49% of the cohort remained free of progression or treatment. The cumulative incidence of biopsy grade reclassification was 43% and an estimated 49% of the cohort underwent treatment. Progression to metastatic cancer occurred in 21 patients (1.4%) and there were three prostate-cancer related deaths (0.1%).
Associate Professor David Smith, Prostate Cancer Stream Lead at The Daffodil Centre, The University of Sydney, Sydney, told Medicine Today that at the very top level this paper shows the safety of a conservative approach for men with low- and very low-risk prostate cancer using AS rather than surgery or radiation. AS was safe, well tolerated and very often used in Australia, he added.
Professor Smith recommended that when assisting men to make shared decisions about prostate cancer testing, GPs indicated that many cancers detected in asymptomatic men would be managed conservatively.
‘Active surveillance is an important tool used to minimise the harms of over-treatment,’ he said.
AS, or deferred treatment, was now recommended in almost all major guidelines, including Australian guidelines, as the primary management approach for men with low-risk cancers. However, a current problem, Professor Smith said, was the wide variety in the approach used to recruit, monitor and manage men on AS.
‘A recent systematic review showed 375 different active surveillance protocols being used internationally,’ said Professor Smith. ‘Most of these predate some of the current tools used in clinical practice, and very few used mpMRI [multiparametric MRI] in the selection of patients or in the monitoring protocols,’ he added.
‘MRI is now a vital part of the process of diagnosis and follow up of Australian men on active surveillance, having been listed on MBS in 2018.’
Professor Smith noted that another identified problem in Australia has been very poor adherence to commonly accepted AS protocols.
‘A previous study from Victoria showed that almost three-quarters of men with low-risk disease did not have either regular PSA tests or biopsies that would be expected with a conservative active surveillance protocol,’ he said.
‘By offering a structured and protocol-based system of follow up and delaying or avoiding radical treatment, patients can postpone or completely avoid the often severe and long-term side effects of treatment, such as erectile dysfunction, urinary incontinence and sometimes bowel problems, without impacts on their survival,’ he added.