Updated guidelines on preventing and managing poor bone health in the over 50s
By Rebecca Jenkins
Updated evidence-based recommendations on preventing and managing poor bone in older patients have been released by the Royal Australian College of General Practitioners (RACGP) in partnership with Healthy Bones Australia.
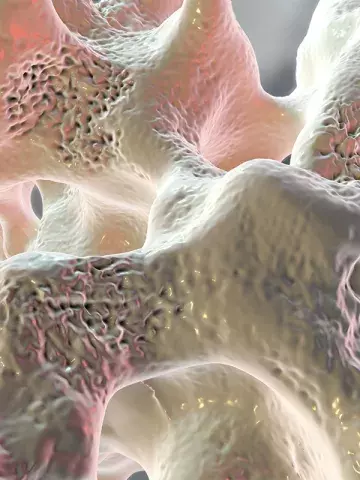
First published in 2017, the latest edition of the Osteoporosis Prevention, Diagnosis and Management in Postmenopausal Women and Men Over 50 Years of Age guideline aims to help GPs manage patients over 50 years of age with poor bone health, including osteopenia and osteoporosis.
Among the updates in this edition are recommendations on the use of fracture risk assessment tools for screening.
Associate Professor Peter Wong, Chair of the National Osteoporosis Guidelines Review Committee, said the guidance recommended using the Fracture Risk Assessment Tool FRAX® (https://fraxplus.org) to calculate 10-year absolute fracture risk, rather than the Garvan Fracture Risk Calculator (https://www.garvan.org.au/promotions/bone-fracture-risk/calculator/).
‘Feedback from GPs after the previous guideline edition was that they wanted clear advice about which absolute risk factor fracture calculator they should use,’ he told Medicine Today. ‘However, the Garvan calculator still has a role in someone with frequents falls as falls is one of its input criteria.’
Professor Wong, who is Honorary Medical Director of Healthy Bones Australia (formerly, Osteoporosis Australia), said other guideline updates included advice on the importance of giving denosumab on time to avoid risk of rebound vertebral fractures, especially in those with pre-existing vertebral fractures.
‘If planning to cease denosumab there is a need to follow up with 12 months of oral or intravenous bisphosphonate to “lock in” the gain in bone mass density (BMD) seen with denosumab and to lower the risk of rebound vertebral fractures,’ he added.
‘However, denosumab is a pretty safe drug to continue long term as it has a lower risk of delayed dental healing or atypical femoral fracture than with a bisphosphonate.’
The guideline also stated that the identification of patients at imminent, very high or high fracture risk was emerging as an important part of osteoporosis care.
Professor Wong said this cohort of patients should be referred for specialist care and considered for early use of bone-anabolic agents such as teriparatide and the newer medication romosozumab.
Romosozumab had several advantages over teriparatide, Professor Wong noted, including that it required monthly administration over 12 months compared with the daily subcutaneous injections needed over 18 months for teriparatide.
‘It also produces a marked increase in BMD over teripara tide due to its dual effect of increasing bone anabolism and lowering bone resorption, which is a novel mechanism of action,’ he said.
The guideline also contained updated recommendations on delayed dental healing and the management of bone health in patients undergoing androgen deprivation therapy for prostate cancer or aromatase inhibitor treatment for breast cancer.
Professor Wong noted the guidance includes a onepage flowchart for osteoporosis risk assessment, management and diagnosis, which he encouraged GPs to print out for easy reference.