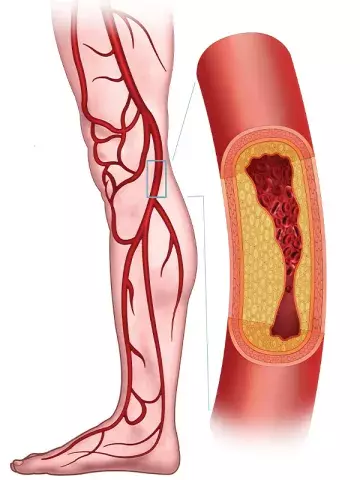
Peripheral artery disease: age-related differences in amputation risk after revascularisation
By Rebecca Jenkins
Patients aged under 60 years with peripheral artery disease (PAD) are at increased risk of major amputation after lower limb revascularisation compared with older patients, a large study finds.
Researchers used data from the Hospital Episode Statistics Admitted Patient Care register to identify patients (≥50 years of age) who underwent lower limb revascularisation for PAD in England from April 2013 to March 2020.
A Markov illness-death model was developed to describe patterns of survival after the initial lower limb revascularisation, if and when patients experienced major amputation, and survival after amputation.
Most of the 94,690 people in the study cohort were men (65.6%), and the median age was 72 years, researchers reported in Circulation.
One-third (34.8%) of patients had nonelective revascularisation, whereas the remainder had elective procedures.
For nonelective patients, the amputation rate was 15.2% and 19.9% at one and five years after revascularisation, respectively. For elective patients, the corresponding amputation rate was much lower: 2.7% and 5.3%, respectively.
‘Overall, the risk of major amputation was higher among patients who were younger, had tissue loss, diabetes, greater frailty, non-elective revascularization, and more distal procedures,’ the researchers wrote.
The mortality rate at five years after revascularisation was 64.3% for nonelective patients and 33.0% for elective patients.
‘Mortality increased with age, but patients <60 years of age were at a higher risk of major amputation than patients ≥80 years of age, particularly after nonelective revascularization,’ the researchers reported.
Patients also had an increased risk of mortality after major amputation if they underwent the procedure within six months of their index revascularisation.
‘More than two-thirds of major amputations performed on patients with previous revascularization were after nonelective revascularizations, whereas the majority of major amputations occurred within six months of the index revascularization, suggesting precise treatment plans could be developed to help improve patient outcomes,’ the researchers said.
Limb salvage after revascularisation was particularly poor in patients aged under 60 years of age, they added, and focus was required on timely treatment options to improve the outcomes for this patient subgroup.
Professor Rob Fitridge, Professor of Vascular Surgery at the University of Adelaide and Consultant Vascular Surgeon with the Central Adelaide Local Health Network, Adelaide, said the study was interesting and novel in using the illness-death happened to patients after revascularisation.
However, it was unlikely there was an absolute definition used by UK clinicians to define elective versus nonelective patients, which made interpretation difficult.
Nonetheless, the overall message from the study
was that PAD requiring intervention, particularly in urgent situations, was associated with high morbidity and mortality.
‘Early diagnosis of PAD and management of risk factors (diabetes, smoking, hyperlipidaemia and hypertension) is really important to reduce the need for urgent surgery, amputation and death,’ Professor Fitridge told Medicine Today.
‘The younger (middle-aged) patients having a higher risk of major amputation after revascularisation is likely to reflect worse tissue loss and likely infection in the younger patients at presentation,’ he added.
Circulation 2024; 150: 261-271.