Evaluation and management of nail diseases

Nail disease is a common presentation in general practice. Recognising the clinical features of the various nail diseases can ensure that patient referrals to a dermatologist are prompt and that diagnosis and treatment are not delayed.
- Nail disease is a common presentation in general practice and can often be representative of systemic disease.
- The most frequent conditions presenting to general practice include onychomycosis, psoriasis, trauma and melanonychia.
- Recognition of the common clinical features of nail disease, particularly those representing malignancy, can ensure that patients are appropriately referred to a dermatology service and that diagnosis and treatment are not delayed.
- Nail disease can be difficult to treat given the anatomy and associated poor penetrance of treatments, and results may take time to occur; thus, having realistic expectations of treatment outcomes and knowing when to refer in treatment failure is important.
- Patients with longitudinal melanonychia and other features demonstrating dystrophy in the absence of trauma should be promptly referred to a dermatology service.
Nail presentations in general practice are often benign but can provide important clues to the diagnosis of systemic or localised disease. Nails protect the ends of each digit and contribute to dexterity; as such, nail disease can cause pain and lead to functional impairment, as well as aesthetic concerns. Recognising and assessing these changes and features ensures timely diagnosis to facilitate appropriate management. Management is largely facilitated within the primary care setting, but several conditions warrant further specialist input.
The treatment of nail disease can often be challenging owing to the anatomy of the nail, the refractory and indolent nature of many nail conditions and often, the limited scope of treatment options within general practice. The most common nail diseases seen within primary care include fungal infections, psoriasis, trauma and melanonychia. This article summarises common nail presentations and provides an overview of their assessment and treatment.
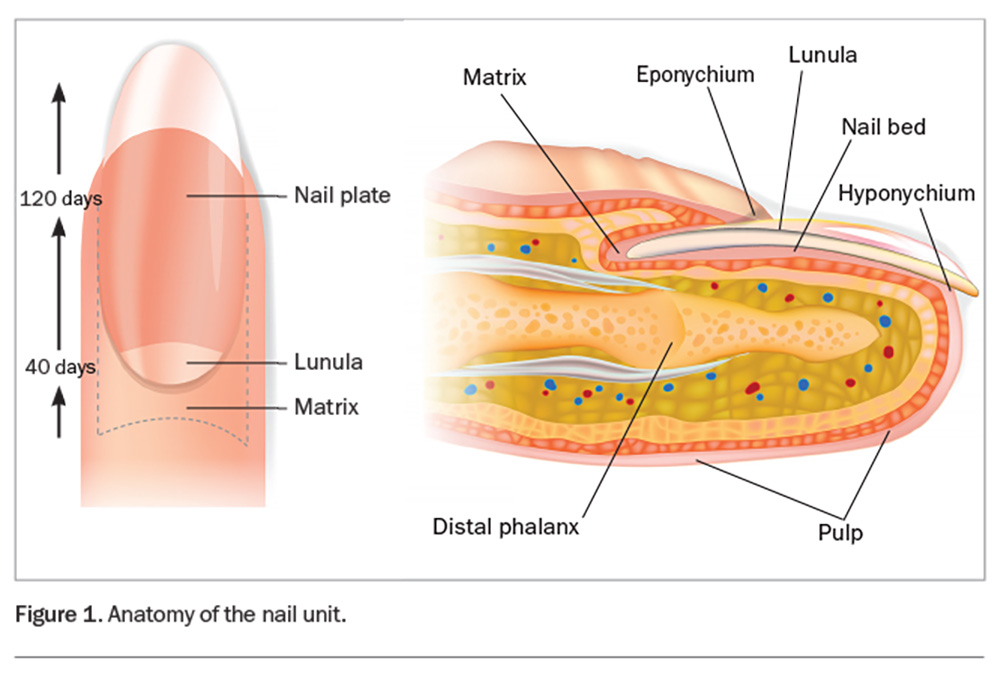
Nail anatomy
Understanding the anatomy of the nail provides insight to the origins of nail disease, as well as the foundations for targeted treatment approaches (Figure 1). The nail matrix is the underlying tissue from which the nail is formed; it is covered by the proximal nail fold and lies close to the bone of the terminal phalanx. The bone is important in forming the shape of the nail. The cuticle (eponychium) arises from the proximal nail fold and is important in protecting the nail matrix by forming a waterproof seal. The nail plate consists of keratin filaments and lies in close apposition to the nail bed. It has longitudinal grooves that interdigitate with the corresponding grooves in the nail bed, allowing for firm adhesion; the area of strongest adhesion is the distal margin of the nail bed, with a corresponding deeper pink hue.1
Assessment
The assessment of nail disease requires a thorough history and examination. The personal or family history of cutaneous malignancy, history of preceding trauma or procedures (podiatry, manicuring), presence of systemic disease (e.g. psoriasis, lichen planus), nutritional status, medications being taken, ethnicity, occupation and hand dominance are all part of history taking.
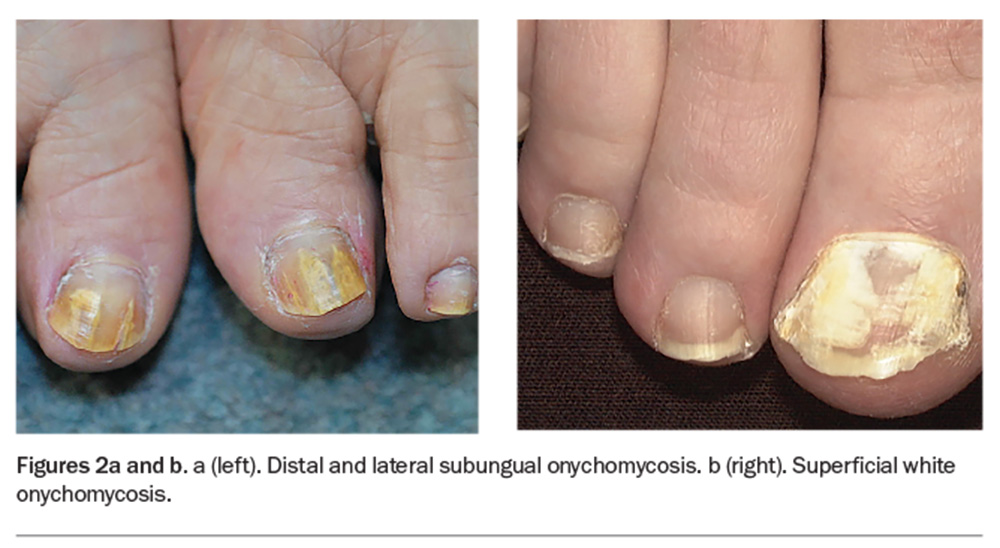
Nails can be affected by infection, trauma, inflammatory disease and malignancy. The common clinical features to identify and assess and the differential diagnoses to consider during an examination of a diseased nail are summarised in Table 1.
Investigations
Most nail diseases can be diagnosed with thorough examination, often in conjunction with dermoscopy. In some cases, further assessment may be required through biopsy. Nail samples, including clippings or scrapings, can be collected in general practice and sent for microscopy and culture, histology or polymerase chain reaction (PCR) testing.
Occasionally, other imaging modalities may be required for further characterisation. Ultrasounds are useful for detecting cystic lesions (e.g. pseudomyxoid), whereas magnetic resonance imaging is useful for detecting glomus tumours. Plain film radiography and broader investigations may form part of the work up to investigate other systemic underlying diseases. Confocal laser scanning microscopy is an innovative, non invasive imaging technique allowing for the examination of nail specimens, thereby avoiding the need for biopsy.2
Referral
Patients with refractory conditions, particularly in conjunction with other cutaneous disease or where malignancy needs to be ruled out, should be referred to a specialist dermatology or nail service. Malignant melanoma forms an important differential for any presentation of melanonychia or nail dystrophy in the absence of trauma (amelanotic melanoma).
Common nail diseases
Patients may present with one or more of the many common nail diseases.
Onychomycosis
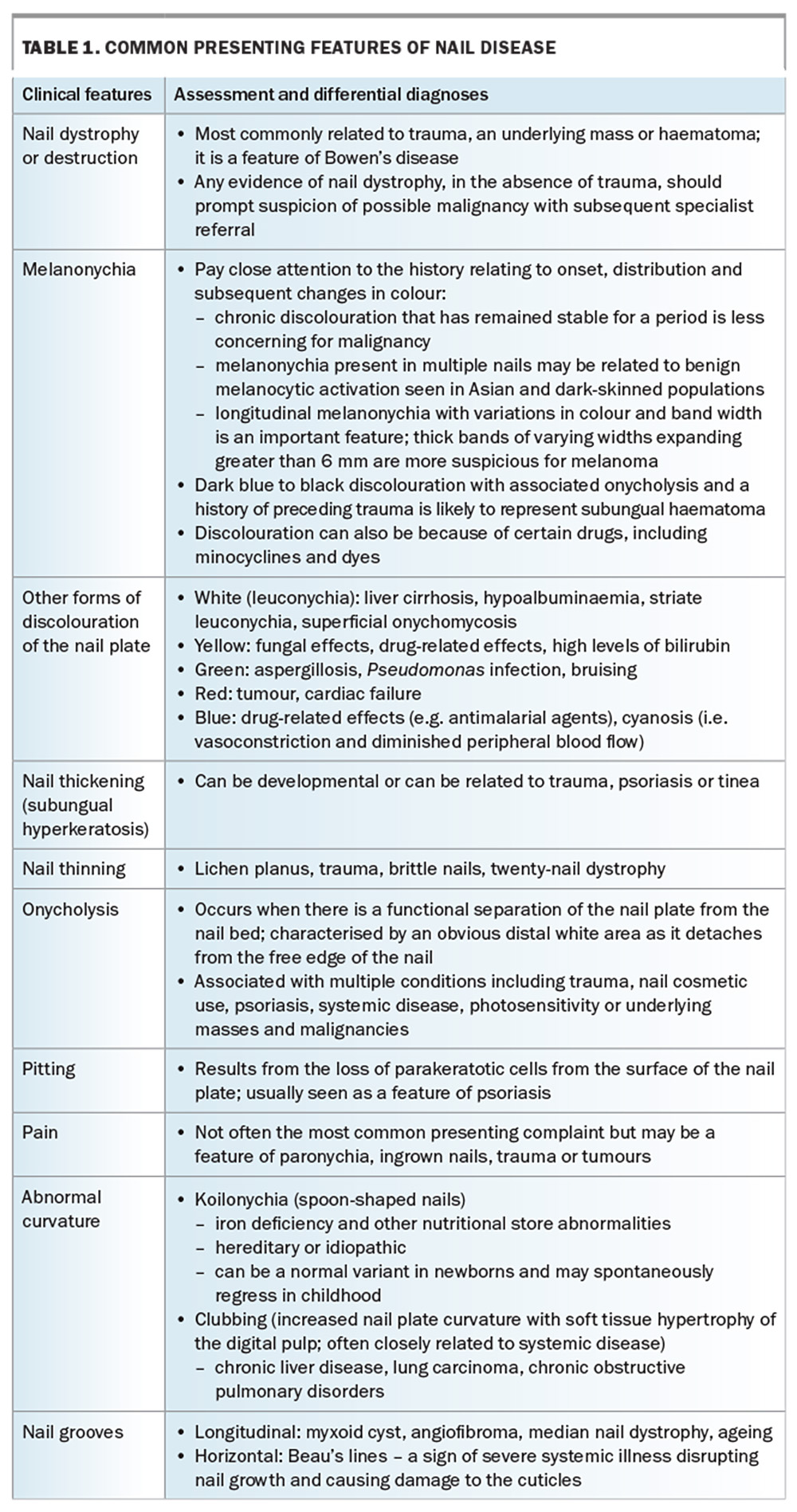
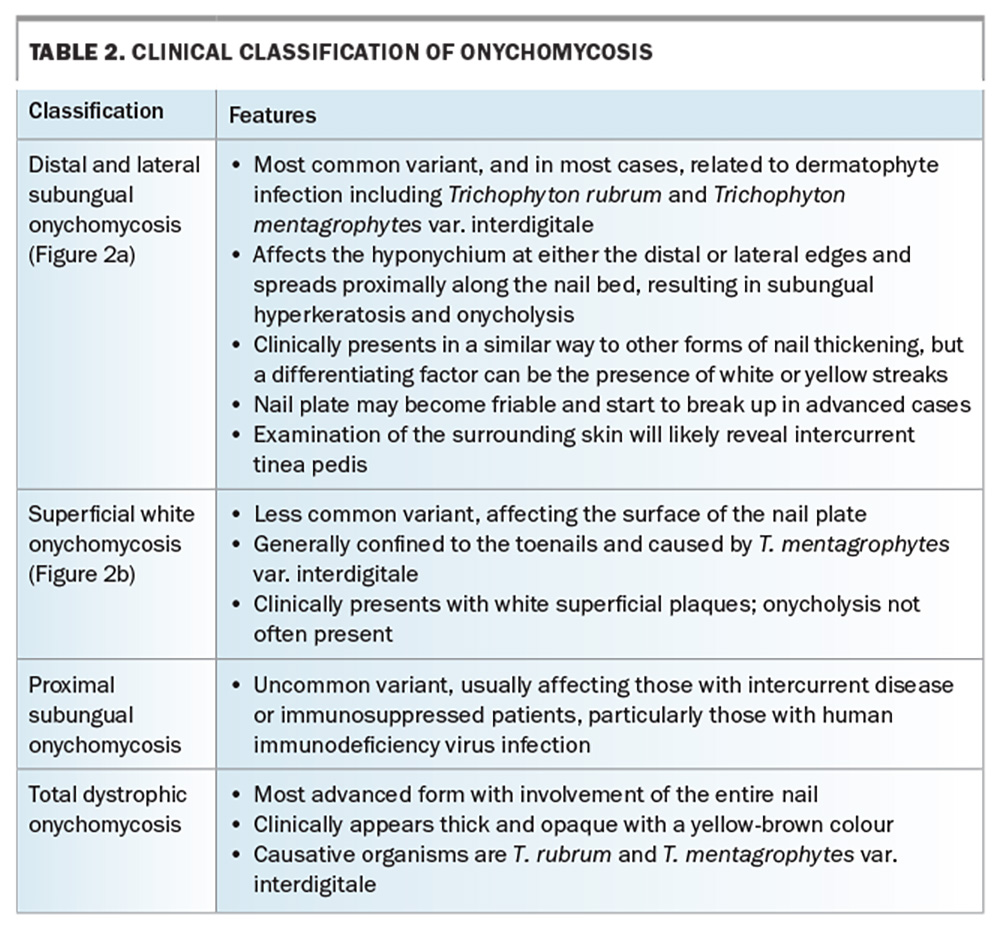
Onychomycosis, or fungal infection, is the most common nail disease (Figures 2a and 2b). It is a treatable cause of nail thickening, and the toenails are more often involved than the fingernails. The risk factors include immunosuppression, advancing age and the presence of diabetes. Fungal infections are mostly caused by dermatophyte infections, with 80% of cases caused by Trichophyton rubrum or Trichophyton mentagrophytes var. interdigitale, as well as other nondermatophyte causes include yeasts (Candida) and moulds (including Aspergillus).3 Patients should be assessed for intercurrent tinea pedis. Although onychomycosis is often a cosmetic problem, it can lead to pain or cellulitis if left untreated. Clinical classification is based on the site of fungal invasion (Table 2).
Diagnosis
When a fungal infection is suspected, several samples of nail clippings, nail scrapings and subungual debris should be sent for microscopy and culture, ensuring the nail is adequately cleaned beforehand to prevent contamination. Direct light microscopy using a potassium hydroxide solution can detect hyphae, which confirms fungal infection. However, a culture is required to identify the fungus, the results of which often take four to six weeks to obtain. Histological evaluation can also detect fungal infection with periodic acid-Schiff staining.
Treatment
Eradication of a fungal infection and complete treatment are often difficult to achieve as there is a tendency for recurrence.4 Cures can be defined as mycotic, indicating the absence of the disease-causing organism on microscopy and culture, or clinical, indicating improvement in the appearance of the nail. It can take up to a year to achieve a completely normal appearance of the nail and, therefore, giving patients realistic expectations of the trajectory and outcome is important.
The treatment of choice is terbinafine (250 mg daily for three months), with 70 to 80% of patients showing complete improvement, and a 10% recurrence rate affecting toenails. For fingernails, a six-week course is sufficient. The side effects include gastrointestinal complications, and monitoring with liver function tests is advised.5,6
Alternatively, itraconazole administered in pulse doses can help achieve a cure rate of 70%, with an 11% recurrence rate. The dose is 200 mg twice a day for one week each month, and the number of pulses may differ between fingernails and toenails. This dose regimen is often better tolerated by patients than the terbinafine treatment regimen, promoting greater compliance. Itraconazole has a broader spectrum of activity, including against Candida and mould, compared to that of terbinafine, with a similar side effect profile.5,6
Topical therapies such as nail lacquers (e.g. amorolfine) and over-the-counter mentholated ointments have varying success. These are more effective for superficial white onychomycosis. In general, it is more difficult for these treatments to penetrate through the nail plate. New triazole-based antifungal agents, including posaconazole and ravuconazole, warrant further exploration as treatment options.
Referral to a dermatology service is required for treatment-resistant cases. In treatment-refractory cases, some patients may require whole or partial nail removal. Physical therapies, such as photodynamic therapy with the use of aminolevulinic acid and excimer pulsed dye lasers, may be effective against onychomycosis. The laser penetrates and heats the nail to destroy the disease-causing organism. However, these treatments are painful and expensive.7
Nail psoriasis
Nail psoriasis can present like onychomycosis; the clinical features are often nonspecific and may be common with those of other conditions. Psoriasis affecting the nail bed may include onycholysis, subungual keratosis, oil spot discolouration and splinter haemorrhages (Figure 3). Nail matrix disease may present as pitting, a crumbling nail plate, red spots in the lunula or leuconychia.
Nail psoriasis is present in about half of patients with psoriasis and may be associated with greater severity in terms of the extent of body surface involvement and treatment resistance.8,9 The incidence of nail disease in patients with psoriatic arthritis is greater than 80%. It is important to assess the quality of life in patients with nail psoriasis, given both the functional and emotional impacts of the disease.8
Assessment
The assessment of nail psoriasis includes ruling out onychomycosis by microscopy and culture of nail clippings. Histopathological features suggestive of psoriasis include parakeratosis. The Nail Psoriasis Severity Index is a simple assessment tool to evaluate nail psoriasis.10 To obtain a score on this index, each nail is divided into four quadrants and a score is ascribed depending on the presence of specific features in each quadrant.
Management
The management of nail psoriasis involves avoiding trauma; this includes manicuring and nail biting. As with cutaneous psoriasis, nail psoriasis exhibits the Koebner phenomenon (the appearance of new skin lesions in previously unaffected areas), by which trauma exacerbates the disease.
Topical treatment includes topical corticosteroids or calcipotriol in ointments, creams, lotions or nail lacquers that can be used for disease affecting the nail matrix or nail bed; however, treatment success is poorly documented.11 The side effects of topical corticosteroids may include telangiectasia or atrophy of the surrounding skin.
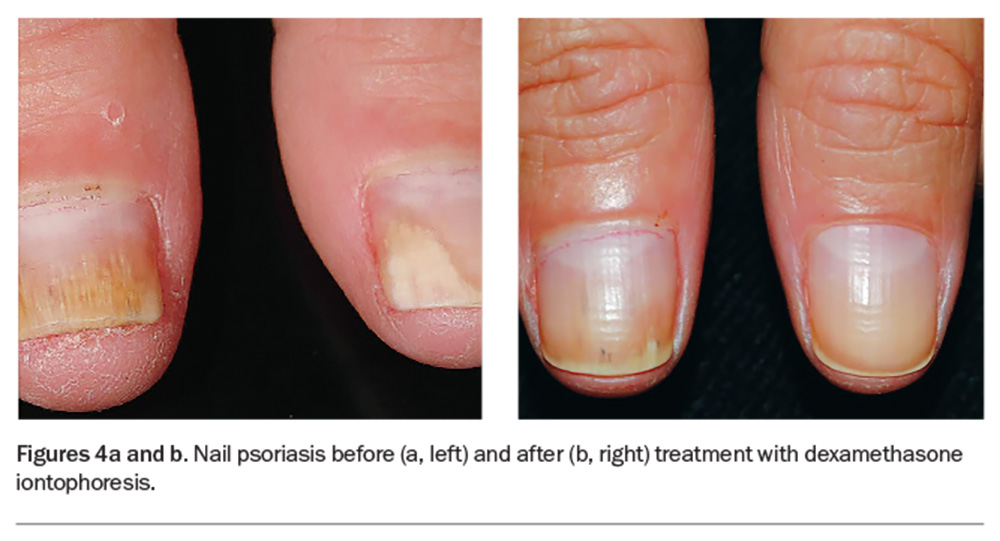
Intralesional corticosteroid injections into the nail matrix or nail bed are effective, albeit a painful option.12 Dexamethasone iontophoresis has minimal side effects and may be beneficial for patients who are resistant to topical treatments.13 The therapy duration is 20 minutes weekly, for four to six months (Figures 4a and 4b).
Systemic treatments include methotrexate, ciclosporin, acitretin and apremilast. These are generally used for patients with concurrent systemic psoriasis. Systemic biologic therapies for the treatment of cutaneous psoriasis have additionally demonstrated efficacy in patients with nail psoriasis; as such, future treatment may centre on these emerging therapies.14 However, these are not currently PBS subsidised for nail disease alone so they are not accessible for patients in the absence of systemic disease.
Longitudinal melanonychia
The presentation of longitudinal melanonychia on the nail plate represents a spectrum of benign conditions including melanocytic nevus or racial melanonychia. Despite this, it is often difficult to distinguish features clinically from nail unit melanoma, which carries a disproportionally high mortality rate when compared with other forms of cutaneous melanoma.15
Nail unit melanoma is a malignant melanoma of the acral lentiginous type and can involve any part of the nail matrix. It is rare, accounting for 1 to 2% of all cutaneous presentations, with a higher incidence in Asian populations. Some patients report a history of preceding trauma.
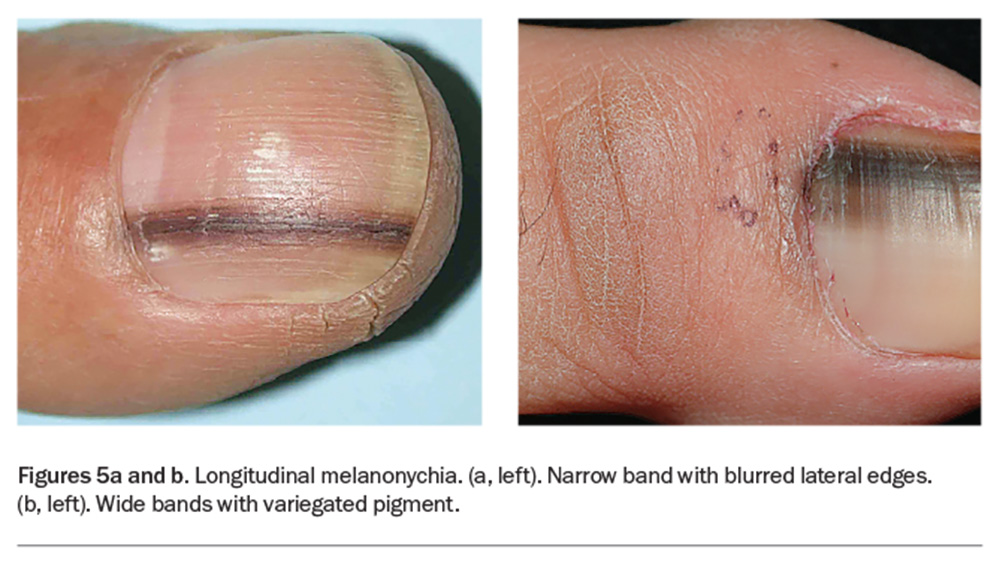
Longitudinal melanonychia is characterised by dark brown or black longitudinal streaks within the nail plate (Figures 5a and 5b). The disease presents when melanocytes within the nail matrix are either activated or proliferate (benign or malignant). The most common locations are on the thumb or great toe, presenting on an isolated digit.
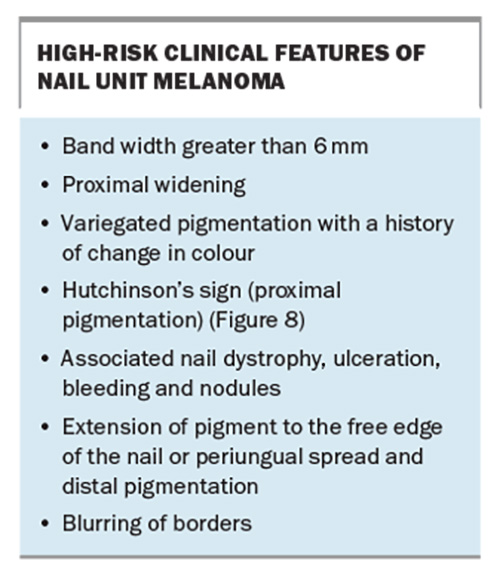
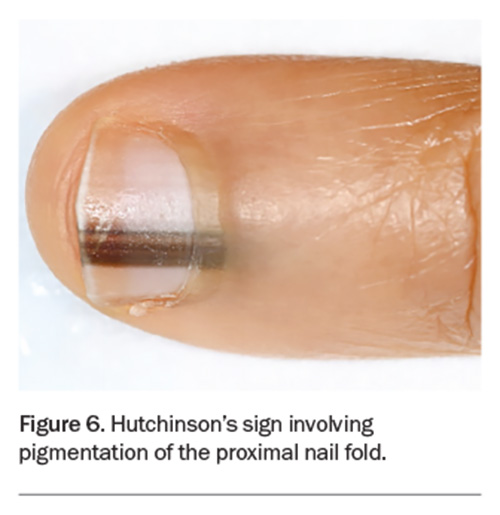
The associated high-risk clinical features that should raise suspicion for nail unit melanoma are summarised in the Box. No single feature is pathognomonic. Any case of nail destruction or dystrophy, in the absence of trauma, should warrant suspicion and prompt referral to a dermatology or nail service. Hutchinson’s sign, both a clinical and dermoscopic feature, is an extension of the darker pigment originating in the nail matrix onto the adjacent cuticle and proximal or lateral nailfolds. It is an important clue for melanoma; however, this is not present in all cases of malignancy (Figure 6).16 Treatment and prognosis are guided by the thickness and level of invasion of melanoma. Malignant melanoma will often require wide local excision and amputation of the distal phalanx, and patients may be referred to a multidisciplinary team to co-ordinate adjunctive therapies.
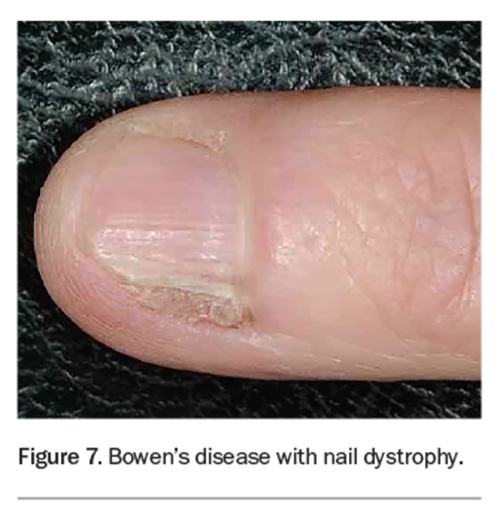
Bowen’s disease (squamous cell carcinoma in situ)
Bowen’s disease, an intraepithelial carcinoma, is one of the most frequently occurring nail malignancies, often presenting as verrucous lesions with associated nail plate dystrophy involving multiple fingernails (Figure 7). It often follows a slow, asymptomatic clinical course before becoming invasive. As such, misdiagnosis, or a delay to diagnosis, is common. It is associated with human papillomavirus (HPV; subtypes 16 and 32) and genital warts.17
Diagnosis is based on the results of punch or longitudinal biopsy. PCR assays are used to detect HPV DNA. The treatment includes photodynamic therapy or imiquimod, although the latter has poor results.18 Mohs surgery is often the most successful approach, allowing for complete eradication of the tumour while preserving normal tissue and function.19 Patients presenting with dystrophy or warty lesions should be referred to a dermatology service to rule out Bowen’s disease.
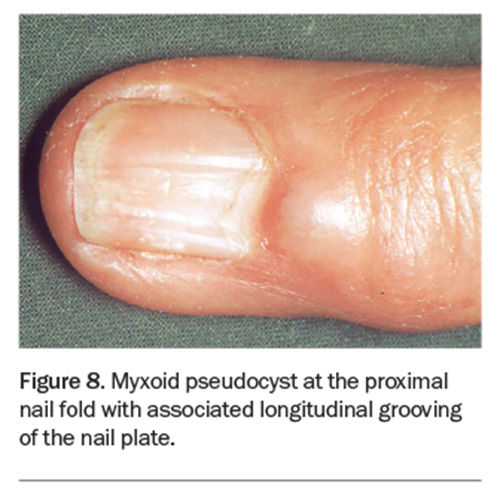
Myxoid pseudocysts
Myxoid pseudocysts occur as firm cysts that are red or translucent in the proximal nail folds of the fingers, and longitudinal grooving of the nails may occur as a result. They do not contain an epithelial lining, differentiating them from true cysts (Figure 8). These cysts have tracts that connect back to the joint from the fingernail or toenail; arthritis at the end of the finger may predispose development. Recurrence is common.
Management involves physical therapies (e.g. cryotherapy, electrocautery, sclerosant injections, intralesional corticosteroid injections or excision of the cyst) or surgery (involving incision and drainage or cyst removal).
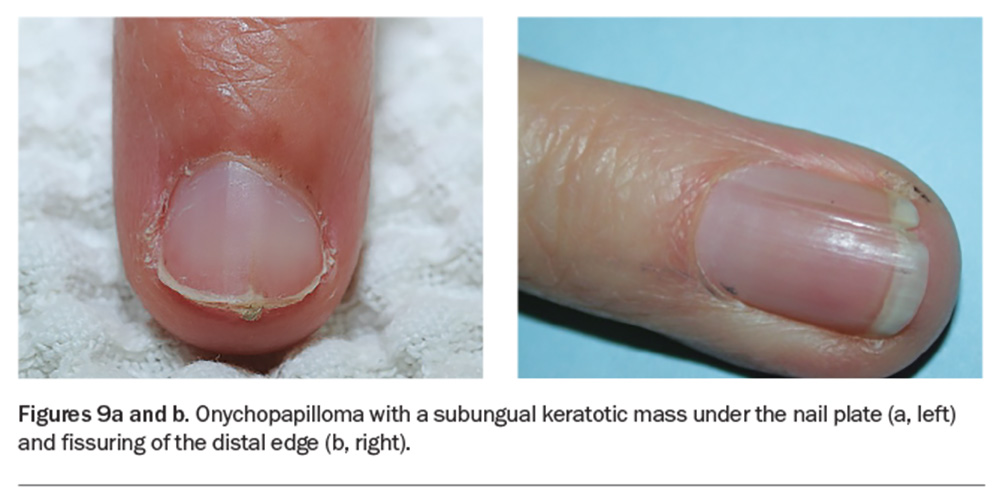
Onychopapilloma
Onychopapilloma is a benign neoplasm of the nail bed and nail matrix. The most common associated clinical features are red or white longitudinal streaks (erythronychia and leuconychia) and a subungual keratotic mass (Figure 9a). Melanonychia, splinter haemorrhage, distal fissuring and onycholysis have all been described (Figure 9b).20 It is usually painless but may impact dexterity.
Onychopapilloma can be diagnosed through the assessment of a nail clipping; samples should include the entire distal nail plate, not just the affected portion. Definitive diagnosis requires excision of the tumour, which is the mainstay of treatment.
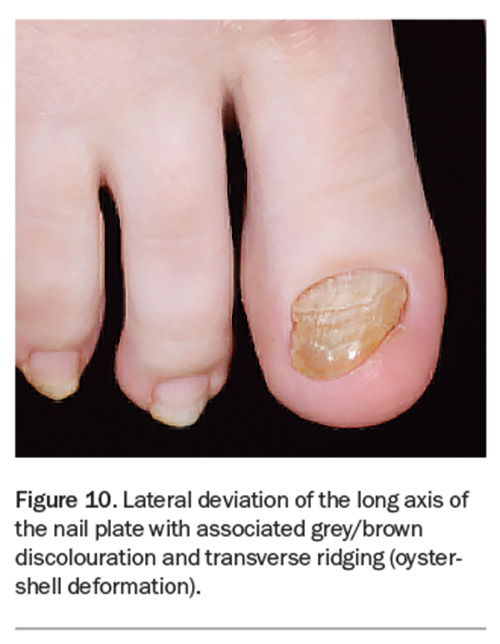
Malalignment
Malalignment refers to deviation of the long axis of the nail from the axis of the terminal phalanx with clinical features (Figure 10). It can be congenital, post-traumatic (laceration to the nail matrix or fractures of the terminal phalanx) or iatrogenic (wide lateral nail biopsies), and usually affects the great toenails. About half of congenital cases will spontaneously resolve by the age of 10 years.
Late-onset malalignment without an inciting precipitant is often the result of unnoticed mild or minimal deviation in childhood, and then repeated chronic low-grade trauma, including exercise or tight footwear against the toenail.21
Treatment includes ensuring footwear fits appropriately and maintaining a shorter nail length. Toe taping works to counter the lateral pull exerted by the extensor tendons of the hallux and ameliorate distal nail wall hypertrophy. Podiatrists can assist with burring the thickened nail. Cases of severe or persisting malalignment may need surgery involving rotation of the whole nail unit (nail matrixectomy).
Chronic paronychia
Chronic paronychia is most prevalent in people with frequent exposure to water, soap and detergents. Damage to the cuticle occurs, leading to erythema of the proximal nail fold and swelling (Figure 11). The damaged cuticle is more susceptible to water and chemical penetration to the nail matrix and inflammation on the surface of the nail fold. It is also associated with dermatitis and infection with Candida albicans or Pseudomonas.
Management is environmental, with the avoidance of contact with aggravating agents, wearing of gloves, avoidance of trauma around the cuticles and application of barrier creams such as petroleum jelly to the nail fold. Cuticle regeneration usually takes six weeks.
Conclusion
Patients often present with nail disease in general practice, and these presentations can be acute or chronic. The most common presentations include onychomycosis, psoriasis, trauma and melanonychia. Recognising the key clinical features and management options can prevent treatment delays. Most nail diseases can be investigated and treatment initiated within the general practice setting; however, treatment may require persistence, and failure is common. Referring these patients, as well as red-flag presentations, promptly to a dermatologist or dedicated nail service can expedite and improve the management outcomes for these patients. MT
COMPETING INTERESTS: None.
References
1. Rich P. Nail surgery. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology, 2nd ed. St. Louis: Mosby/Elsevier; 2006. p. 2260.
2. Sattler E, Kaestle R, Rothmund G, Welzel J. Confocal laser scanning microscopy, optical coherence tomography and transonychial water loss for in vivo investigation of nails. Br J Dermatol 2012; 166: 740-746.
3. Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther 2010; 35: 497-519.
4. Tosti A, Piraccini BM, Stinchi C, Colombo MD. Relapses of onychomycosis after successful treatment with systemic antifungals: a three-year follow-up. Dermatology 1998; 197: 162-166.
5. Lipner SR, Scher RK. Onychomycosis: treatment and prevention of recurrence. J Am Acad Dermatol 2019; 80: 853-867.
6. Tinea. Expert Group for Dermatology. Melbourne: Therapeutic Guidelines Limited; 2015. Available online at: https://tgldcdp.tg.org.au/index
7. Watanabe D, Kawamura C, Masuda Y, Akita Y, Tamada Y, Matsumoto Y. Successful treatment of toenail onychomycosis with photodynamic therapy. Arch Dermatol 2008; 144: 19-21.
8. Lawry M. Biological therapy and nail psoriasis. Dermatol Ther 2007; 20: 60-67.
9. de Jong EM, Seegers BA, Gulinck MK, Boezeman JB, van de Kerkhof PC. Psoriasis of the nails associated with disability in a large number of patients: results of a recent interview with 1,728 patients. Dermatology 1996; 193: 300-303.
10. Rich P, Scher RK. Nail Psoriasis Severity Index: a useful tool for evaluation of nail psoriasis. J Am Acad Dermatol 2003; 49: 206-212.
11. Jiaravuthisan MM, Sasseville D, Vender RB, Murphy F, Muhn CY. Psoriasis of the nail: anatomy, pathology, clinical presentation, and a review of the literature on therapy. J Am Acad Dermatol 2007; 57: 1-27.
12. Rigopoulos D, Baran R, Chiheb S, et al. Recommendations for the definition, evaluation, and treatment of nail psoriasis in adult patients with no or mild skin psoriasis: a dermatologist and nail expert group consensus. J Am Acad Dermatol 2019; 81: 228-240.
13. Le QV, Howard A. Dexamethasone iontophoresis for the treatment of nail psoriasis. Australas J Dermatol 2013; 54: 115-119.
14. Reich K, Sullivan J, Arenberger P, et al. Secukinumab shows high and sustained efficacy in nail psoriasis: 2.5-year results from the randomized placebo-controlled TRANSFIGURE study. Br J Dermatol 2021; 184: 425-436.
15. Chakera AH, Quinn MJ, Lo S, et al. Subungual melanoma of the hand. Ann Surg Oncol 2019; 26: 1035-1043.
16. Baran R, Kechijian P. Hutchinson’s sign: a reappraisal. J Am Acad Dermatol 1996; 34: 87-90.
17. Perruchoud DL, Varonier C, Haneke E, et al. Bowen disease of the nail unit: a retrospective study of 12 cases and their association with human papillomaviruses. J Eur Acad Dermatol Venereol 2016; 30: 1503-1506.
18. Wollina U. Bowen’s disease of the nail apparatus: a series of 8 patients and a literature review. Wien Med Wochenschr 2015; 165: 401-405.
19. Zaiac MN, Weiss E. Mohs micrographic surgery of the nail unit and squamous cell carcinoma. Dermatol Surg 2001; 27: 246-251.
20. Tosti A, Schneider SL, Ramirez-Quizon MN, Zaiac M, Miteva M. Clinical, dermoscopic, and pathologic features of onychopapilloma: a review of 47 cases. J Am Acad Dermatol 2016; 74: 521-526.
21. Wang CY, Kern J, Howard A. Late-onset malalignment of the great toenails. Australas J Dermatol 2019; 60: 315-317.