A progressive plaque on the lower limb
Test your diagnostic skills in our regular dermatology quiz. What is this enlarging plaque on a woman’s leg, which has recently become painful?
Case presentation
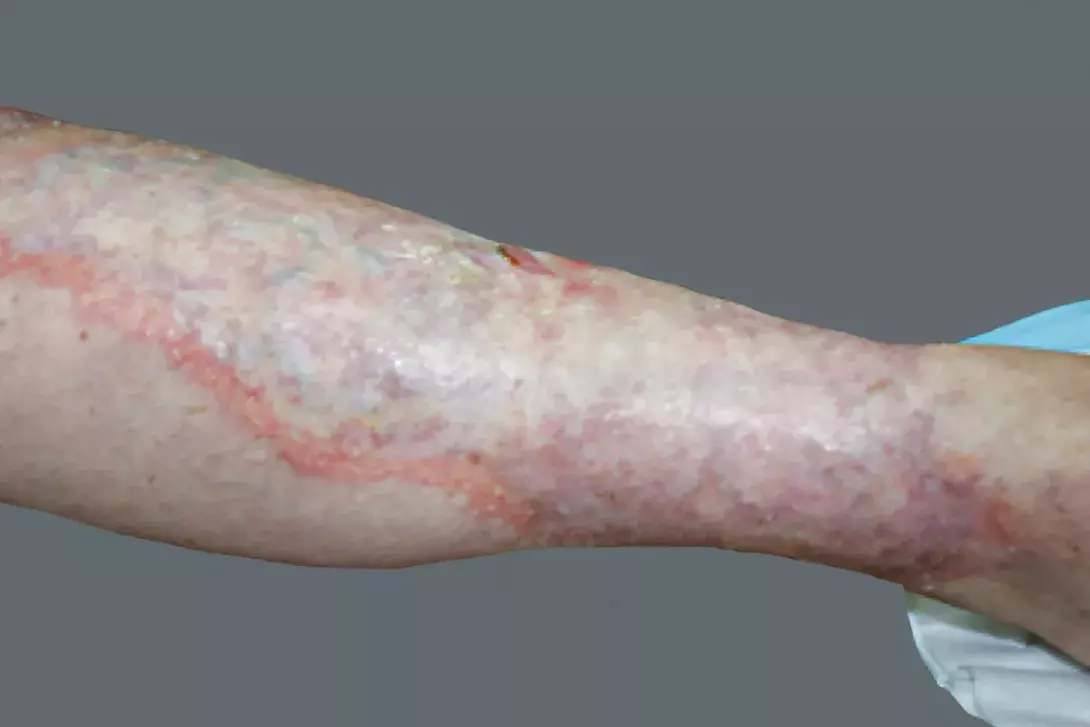
A 52-year-old woman with insulin-dependent diabetes presents with a yellow-red telangiectatic plaque on the pretibial surface of her left leg (Figure). The lesion is well-demarcated, with an elevated peripheral violaceous rim, and gradually enlarging. The lesion was painless but recently began to erode centrally and has become painful.
Differential diagnoses
Conditions to consider in a patient with evolving chronic erosive plaques include the following.
- Lipodermatosclerosis. This panniculitis has a predominance in females, with onset mainly in the fifth decade of life, and is associated with chronic venous insufficiency.1 The acute phase of lipodermatosclerosis is characterised by diffuse, erythematous induration that is warm and painful proximal to the medial malleolus. Chronic lesions are well-demarcated hyperpigmented, red-brown plaques, resulting in the classic ‘inverted bottle’ deformity.1 Although biopsy is seldom necessary, an early lesion would show a predominantly lobular panniculitis with septal lymphocytic infiltrate, whereas a chronic lesion would show septal sclerosis.1
- Xanthomas. This group of disorders relates to intra- and extracellular dermal deposition of lipids, which accumulate within macrophages and form foam cells. There are primary and secondary causes, the latter including diabetes mellitus, hypothyroidism, nephrotic syndrome, paraproteinaemia and primary biliary cirrhosis.2 Eruptive xanthomatosis occurs in the setting of primary and secondary hypertriglyceridaemia, with diabetes mellitus a known cause of the latter.3 Eruptive xanthomas typically present as painful and pruritic yellow-red papules with a surrounding inflammatory halo on the extensor surface of the extremities.3 Biopsy shows characteristic foam cells, lipid-laden macrophages within the reticular dermis, with a surrounding mixed lymphocytic-neutrophilic inflammatory infiltrate.3
- Necrobiotic xanthogranuloma. This rare systemic histiocytosis occurs as a result of an underlying lymphoproliferative disorder or monoclonal gammopathy.4 The cutaneous lesions of necrobiotic xanthogranuloma are painless, indurated violaceous papules or plaques with the yellow hue typical of xanthomas. Accompanying ulceration and central atrophy are also seen. They tend to involve the periorbital areas but can also occur on the face, trunk and proximal extremities and can also arise in existing scars. Systemic involvement is common, with half of patients showing concomitant ophthalmic manifestations, including diplopia, anterior uveitis and ectropion with lymphadenopathy.4 Serum electrophoresis detects an impressive monoclonal gammopathy in 80% of affected patients, with IgG-K the most common.4 Necrobiotic xanthogranuloma spares the epidermis and superficial dermis, with palisading granulomas composed of histiocytes, foam cells, lymphocytes, plasma cells, Touton giant cells and necrobiosis involving the mid-dermis with extension to the subcutis.4
- Necrobiosis lipoidica (NL). This is the correct diagnosis. Formerly known as necrobiosis lipoidica diabeticorum, this idiopathic noninfective granulomatous disease was renamed necrobiosis lipoidica because it affects both diabetic and nondiabetic individuals. It generally occurs between the third and fifth decades of life and has a predominance in females.5 The lesions begin as painless multiple small papules, commonly affecting the pretibial surfaces, that gradually enlarge, coalescing into well-demarcated yellow-red telangiectatic plaques with a violaceous rim and central area of waxy, epidermal atrophy.5 Initially asymptomatic, the lesions of necrobiosis lipoidica may cause dysesthesia, pruritus or pain; ulceration occurs in 33% of patients.5 Histopathological features of NL lesions depend on the patient: diabetic NL lesions show predominantly palisading granulomatous dermatitis (histiocytes surrounding degenerative collagen), whereas nondiabetic NL lesions have tuberculoid features, although both share mixed perivascular infiltrate composed predominantly of lymphocytes, and normal or atrophic epidermis.5
Management
An uncommon complication of a common disease, NL occurs in 0.3 to 1.2% of patients with diabetes.5,6 It is difficult to predict who will develop NL because it does not correlate with glycaemic control, although patients with NL have a higher incidence of microvascular complications of diabetes mellitus such as peripheral neuropathy and diabetic retinopathy.5 Furthermore, optimising glycaemic control in diabetic patients with NL does not alter the course of NL lesions.5
NL is notoriously difficult to treat. The mainstays of initial management include corticosteroids (topical and intralesional) and ulcer wound care. Patients should be educated about avoiding trauma to prevent further ulcers that are slow to heal.6
NL is a rare disease and there are no approved treatments. Those that have been reported to have shown benefit include phototherapy, platelet inhibitors, intralesional infliximab, topical tretinoin and tacrolimus.6 Immunosuppressants (e.g. cyclosporin, mycophenolate mofetil) are associated with improving healing in NL-related ulceration, although recurrences following cessation of treatment are common.6 Surgical excision down to the level of the fascia is usually reserved as a last resort because of potential koebnerisation and the requirement for skin grafting.6
Outcome
For this patient, biopsy was not performed because the lesion was advanced, with the characteristic appearance of NL, and there was a risk of suboptimal healing. Initial treatment consisted of intralesional corticosteroid injection around the edge of the lesion to halt progression. Ulcer dressings were used to treat the superficial ulceration, and protective bandaging was used to prevent further trauma-induced ulcers. The patient subsequently responded well to oral cyclosporin at 2.5 mg/kg/day. MT
