Thromboprophylaxis after fracture: aspirin as effective as low-molecular-weight heparin
By Rebecca Jenkins
Aspirin is noninferior to low-molecular-weight heparin for thromboprophylaxis in patients with orthopaedic trauma, a large study finds.
Researchers randomised 12,211 adults aged 18 years and older who had a limb fracture that required surgery or any pelvic or acetabular fracture to receive 30 mg of low-molecular-weight heparin (enoxaparin) twice daily by injection or 81 mg of aspirin orally twice daily.
At 90 days, the primary endpoint of death from any cause was similar between the two groups: 0.78% of patients in the aspirin group and 0.73% in the heparin group.
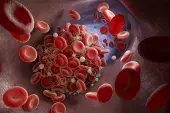
Deep-vein thrombosis (DVT) occurred in 2.51% of patients in the aspirin group and 1.71% in the heparin group, a difference of 0.80 percentage points, researchers reported in The New England Journal of Medicine.
‘The incidence of pulmonary embolism (1.49% in each group), bleeding complications, and other serious adverse events were similar in the two groups,’ they wrote.
The researchers included any fracture of an extremity from hip to midfoot and from shoulder to wrist that was treated operatively as well as any pelvic or acetabular fracture, treated operatively or nonoperatively.
Patients received a mean of 8.8±10.6 in-hospital thromboprophylaxis doses and were prescribed a median 21-day supply of thromboprophylaxis at discharge.
Dr Bronwyn Thorp, Clinical Haematologist at St Vincent’s Health Network Sydney, said the multicentre trial was a landmark study that potentially expanded the role of aspirin thromboprophylaxis in orthopaedics for use post-fracture.
‘The study should at least prompt review of the relevant local and international guidelines,’ she told Medicine Today.
The most significant potential advantage of aspirin over low-molecular-weight heparin was the ease of administration and therefore the rate of compliance.
‘Dosing is not impacted by renal function and extremes of body weight as with low-molecular-weight heparin,’ she said.
But Dr Thorp stressed that questions remained about the optimal use of aspirin for thromboprophylaxis after orthopaedic trauma. There were more symptomatic DVTs in the aspirin arm overall due to increased rates of lower limb DVTs, she noted.
‘Below-knee DVT, although less life threatening than proximal DVT, still necessitates a longer duration of anticoagulation and therapeutic doses, increasing the bleeding risk,’ she said.
‘As the median age was under 50 years in this study, evaluating these two drugs for this indication in an older population with inherent higher bleeding risk and risk of venous thromboembolism will be important.’
In practice, it might be that aspirin is considered an option for thromboprophylaxis in certain groups, such as those in whom compliance is a concern, or those at lower risk of venous thromboembolism, Dr Thorp suggested.