Sustained survival benefits seen with resynchronisation–defibrillation for heart failure
By Michael Doris MB BS
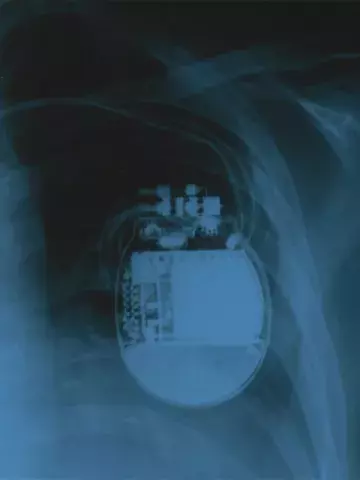
The enduring benefits of cardiac-resynchronisation therapy (CRT) combined with an implantable cardioverter–defibrillator (ICD) for patients with symptomatic heart failure have been confirmed in a long-term follow-up trial to The Resynchronization–Defibrillation for Ambulatory Heart Failure Trial (RAFT).
The original trial investigated whether the addition of CRT to an ICD (CRT-D) would yield superior outcomes compared with ICD alone. This multicentre, double-blind randomised, controlled trial included 1798 participants who had a left ventricular ejection fraction of 30% or less, a QRS complex duration exceeding 120 msec and New York Heart Association (NYHA) class II or III heart failure. After a median follow up of 40 months, those in the CRT-D group had a significantly lower risk of death or hospitalisation for heart failure compared with those in the ICD alone group.
The new follow-up trial, published in The New England Journal of Medicine, included 1050 of the RAFT participants (mean age 66.5 years; 83.8% men) from eight centres. During a median follow up of 7.7 years overall, and 13.9 years among patients who survived, death from any cause was more common in the ICD group (76%) than in the CRT-D group (71%). The time until death also appeared to be longer in the CRT-D group. A similar association was seen for the composite of death from any cause, heart transplantation or implantation of a ventricular assist device.
‘Among patients with a reduced ejection fraction, a widened QRS complex, and NYHA class II or III heart failure, the survival benefit associated with receipt of a CRT-D as compared with ICD appeared to be sustained during a median of nearly 14 years of follow-up,’ the study authors wrote.
Associate Professor Justin Mariani, Consultant Cardiologist, Heart Failure Specialist and Head of Pacing at The Alfred Hospital in Melbourne, said, ‘CRT remains a mainstay long-term treatment for patients with certain types of heart failure and systolic dysfunction.’
He said there were limitations with the study given the duration of follow up, including an absence of data on patients who changed from ICD only to CRT, as is often the case with progressive heart failure.
‘Another limitation was the introduction of more advanced heart failure therapy in the last five years, which have changed the landscape for heart failure. However, the durability of the sustained benefit of CRT in patients who survived compared to ICD alone is worth noting,’ he said, ‘particularly when there has been such a shift in therapies.’
Associate Professor Mariani highlighted the persistent cumulative mortality in both the CRT and ICD groups, as a reminder of the importance of chronic disease management in heart failure.
‘It provides reassurance that offering complex device therapy, even in less symptomatic patients, has meaningful outcomes,’ he told Medicine Today.