Acne scarring – why it occurs and what can be done

Acne scarring is associated with significant psychosocial morbidity. Early and effective treatment is essential for all patients with acne, regardless of the severity, to minimise the inflammation that drives scarring. There are a variety of treatment options for acne scarring and these may be best facilitated by referral to a dermatologist.
- Acne scarring affects about half of all patients with acne.
- Inflammatory acne lesions can stimulate an abnormal healing response, leading to atrophic or thickened scars, regardless of the acne severity.
- Early and effective treatment of acne is necessary to reduce the risk of acne scarring.
- All patients with acne should be informed about the risk of acne scarring.
- High-risk patients include those with severe acne, those with a family history of acne, males and individuals with skin of colour.
- There are a variety of treatment options for acne scarring; a referral to a dermatologist for the development of a comprehensive and multimodal approach should be considered.
- Active acne should be under control before initiating scar treatment.
- Patients should be provided with realistic expectations and a timeframe for treatment.
Acne vulgaris is a common skin disorder, affecting about 85% of individuals.1 Nearly half of these patients may go on to develop acne scarring, which can have significant psychological consequences, including reduced quality of life, depressed mood and, in severe cases, an increased risk of suicide.2 It is important for doctors to recognise that even mild acne can lead to scarring and that we should prioritise early and effective treatment, especially in patients at higher risk of scarring. Once acne scarring occurs, a range of treatment options are available, often requiring a multimodal approach. Many patients present with a combination of different scar types, as well as postinflammatory hyperpigmentation and erythema, all of which should be addressed for optimal outcomes. This article discusses the assessment of and preventive measures for patients with acne, and the available treatment options once scarring is present.
Why does acne scarring occur?
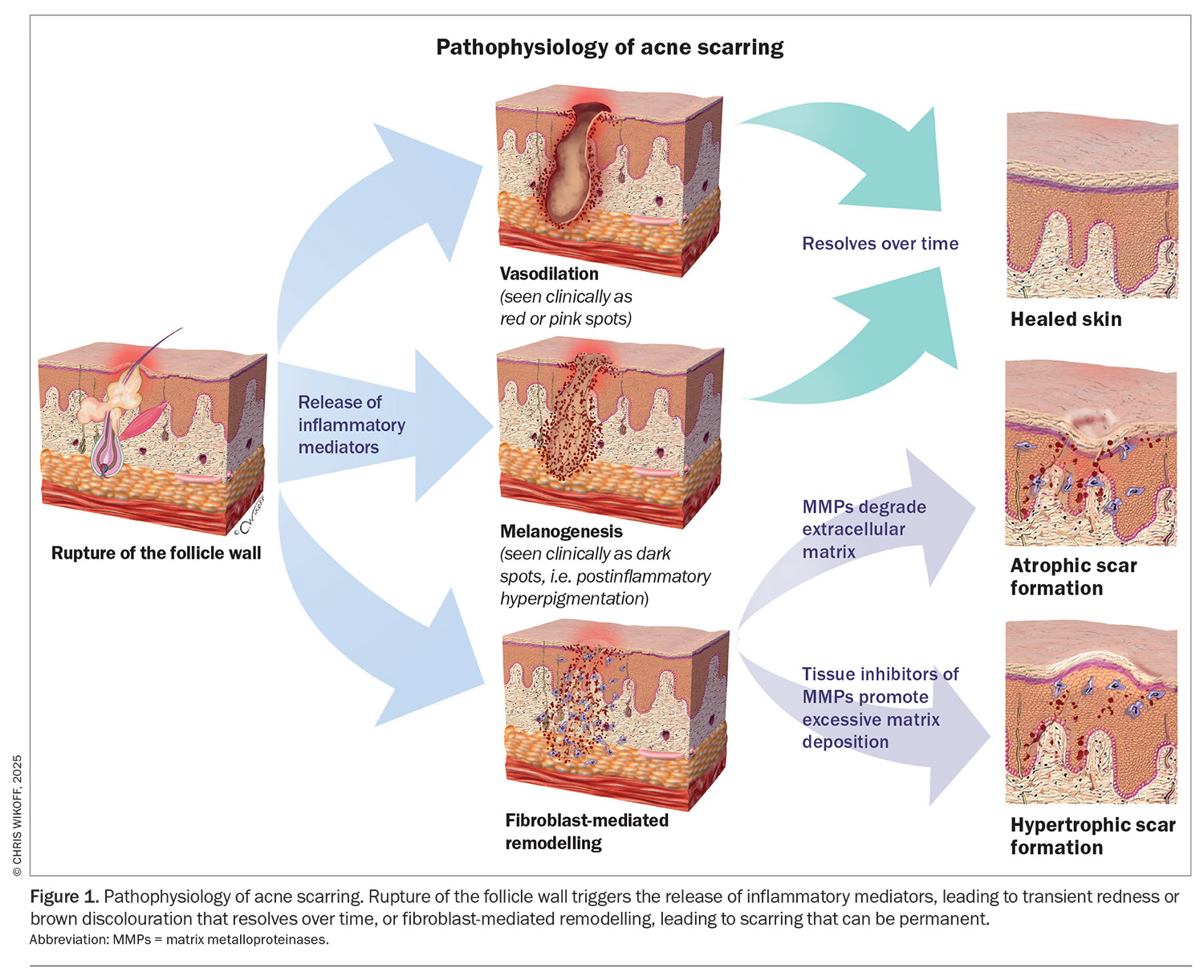
The rupture of the follicular wall in acne lesions triggers an inflammatory response, initiating a wound-healing response that can lead to atrophic or hypertrophic scarring (Figure 1). The location and severity of this wound-healing response determines the types of acne scars that develop. In the early stages, inflammation induces vasodilatation and melanogenesis, leading to postinflammatory erythema (PIE) or postinflammatory hyperpigmentation (PIH). This is followed by fibroblast-mediated matrix remodelling. The release of matrix metalloproteinases (MMPs) degrades the extracellular matrix and can result in atrophic scarring. In contrast, tissue inhibitors of MMPs promote excessive matrix deposition, leading to hypertrophic scarring.3
Atrophic scars are thought to form because the inflammation in an acne lesion is mostly localised to the infundibulum, which is located below the skin surface. Surface contracture creates an atrophic appearance.4 There is an association between this type of scarring and the severity and duration of the inflammatory response. Destruction of sebaceous structures may also contribute to the atrophic appearance.3
Hypertrophic scars are thought to arise from increased fibroblast activity, leading to excessive extracellular matrix formation and collagen overproduction.3
What do acne scars look like?
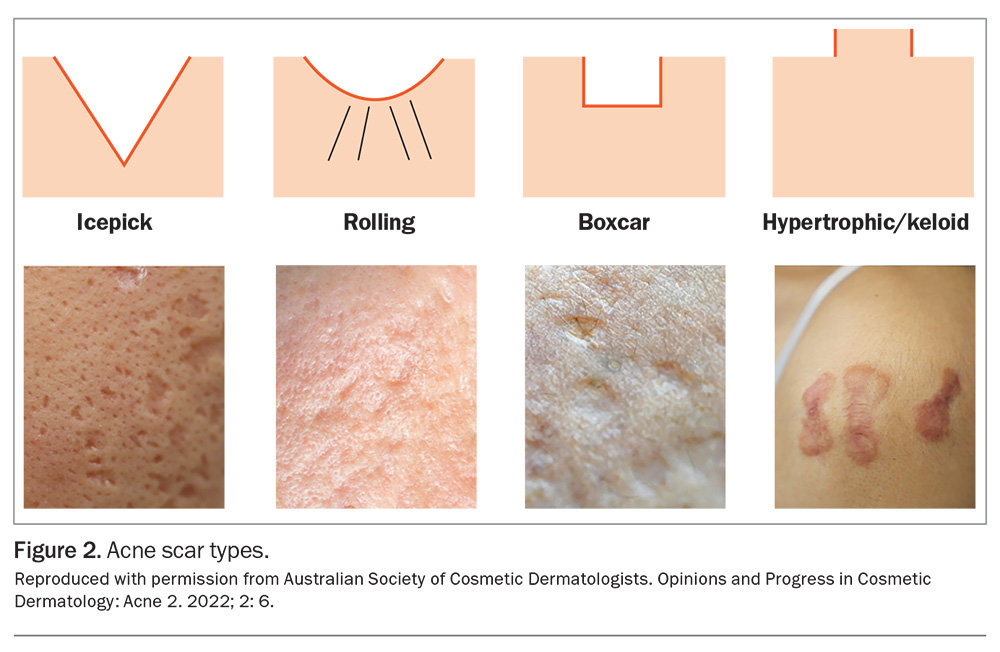
Acne scars are classified based on their appearance and are further defined within each category by structure and depth (Figure 2).
- Atrophic scars are the most common type, occurring three times more frequently than thicker (hypertrophic or keloid) scars. They are subdivided into icepick, boxcar and rolling scars, based on their shape and size.
- Hypertrophic and keloid scars typically develop on the back and shoulders.
- Papular scars most commonly occur on the jawline and trunk, presenting as firm, elevated lesions.
Who develops acne scarring?
Predicting which patients will develop acne scarring remains challenging. A recent meta-analysis identified three major risk factors: male sex, a positive family history of acne and acne severity.2 Additional factors that have been identified include the duration of acne, lifestyle factors, lesion manipulation (squeezing) and acne relapse. Genetic factors may play a role in acne scarring, potentially associated with inherited innate immunity profiles. Patients who are prone to scarring may exhibit a prolonged adaptive immune response, leading to persistent inflammation and impaired wound healing.
Although severe acne is often associated with prolonged and intense inflammation, scarring can also occur in patients with mild acne. Therefore, early and effective treatment is essential for all patients with acne, regardless of the severity, to minimise the inflammation that drives scarring.
The higher risk of acne scarring in males compared with females may be because of anatomical differences in the sebaceous glands, but possibly also because of differences in healthcare-seeking behaviours, as women may be more likely to seek treatment earlier.
The importance of colour
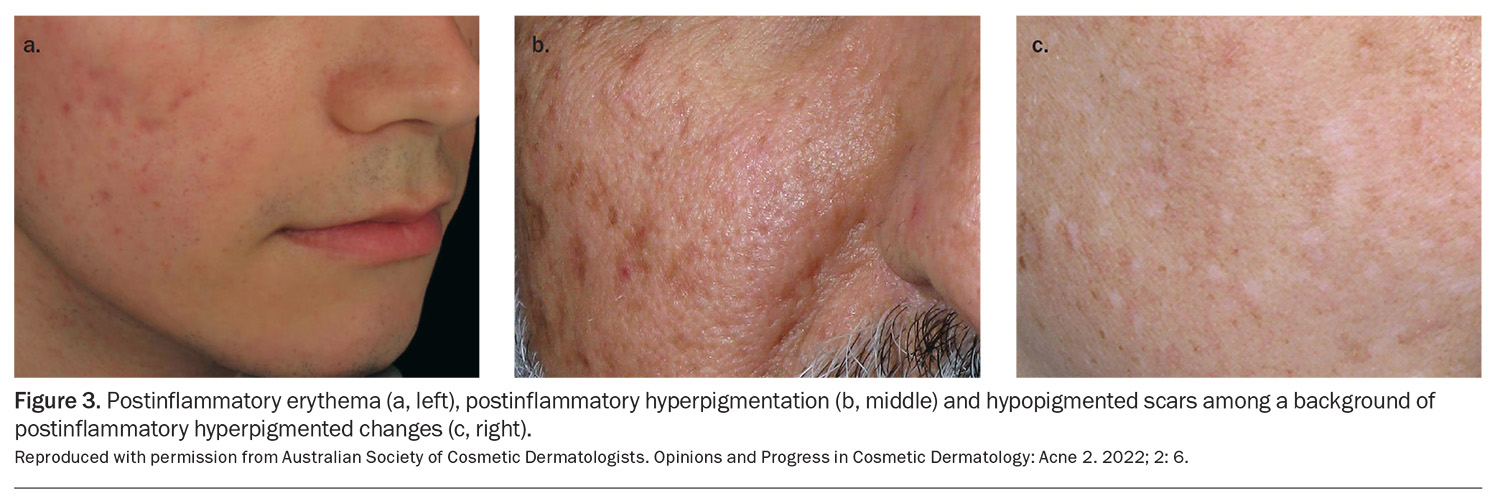
It is essential to distinguish between PIE and PIH versus true acne scarring (Figure 3). Unlike scarring, PIH and PIE are transient and will resolve over time. Therefore, assessment for textural changes, such as skin atrophy (indentation) or thickening, is important in determining whether permanent scarring is present. Side lighting can be useful in assessing this, as it enhances the distinction between textural changes and changes in colour alone. It is also important to note hypopigmented marks or macules. These can also follow inflammatory acne, especially with repetitive squeezing of the acne lesions. This may result in focal and permanent loss of pigment without textural alteration.
Patients should be asked about a previous history of keloid and hypertrophic scarring. Patients with skin of colour are at a higher risk of developing keloid and hypertrophic scars, and this may be because of genetic factors.5
Patient assessment
Early assessment and treatment during the initial stages of acne can significantly reduce the risk of acne scarring. Patients should be informed about the risk of acne scarring and advised to avoid squeezing acne lesions, as this can lead to prolonged inflammation and subsequent scarring.
When examining the patient, existing scars should be assessed for and the degree of inflammation noted. Photographs taken at the time of presentation can be a valuable reference point for monitoring disease progression and treatment response. One study analysing acne scarring found that 94% of patients were dissatisfied with the information they received from their healthcare provider.6 These patients expressed a desire for greater education from their doctors regarding available treatment options (46%), sequelae of acne and acne scarring on different skin types (44%), acne triggers (44%) and determination of acne severity (43%).6 These findings highlighted the need for comprehensive patient education to improve satisfaction and engagement in acne management.
Prevention and management of acne scarring
Timeline of treatment
Managing acne requires consistency, as noticeable improvement with any given treatment plan typically takes at least two to three months. Treating acne scarring is also a stepwise process, often requiring multiple treatment sessions spaced four to eight weeks apart, depending on the selected modalities.
Preventive treatment to reduce the risk of scarring
Preventive treatment for acne scarring aims to provide safe and effective early treatment for acne to minimise the risk of redness, pigmentary change and scarring. Topical retinoids are well established as effective treatments for acne, but several have also demonstrated efficacy in reducing atrophic acne scarring. As early as 1991, topical tretinoin 0.05%, applied daily for four months, has been reported to significantly improve superficial acne scars.7 More recently, both adapalene and the fixed-dose combination of topical adapalene 0.3%/benzoyl peroxide gel 2.5% have been shown to improve atrophic acne scarring.8
The newest topical retinoid, trifarotene, has demonstrated both preventive and therapeutic effects on atrophic acne scarring. In a randomised, split-face, double-blind study, 121 subjects with moderate-to-severe facial acne and acne scars were treated with either trifarotene or vehicle once, daily for 24 weeks. Trifarotene reduced atrophic acne scars at week 24, and differences between both sides were noted as early as week 2.9
Treatment options for scarring
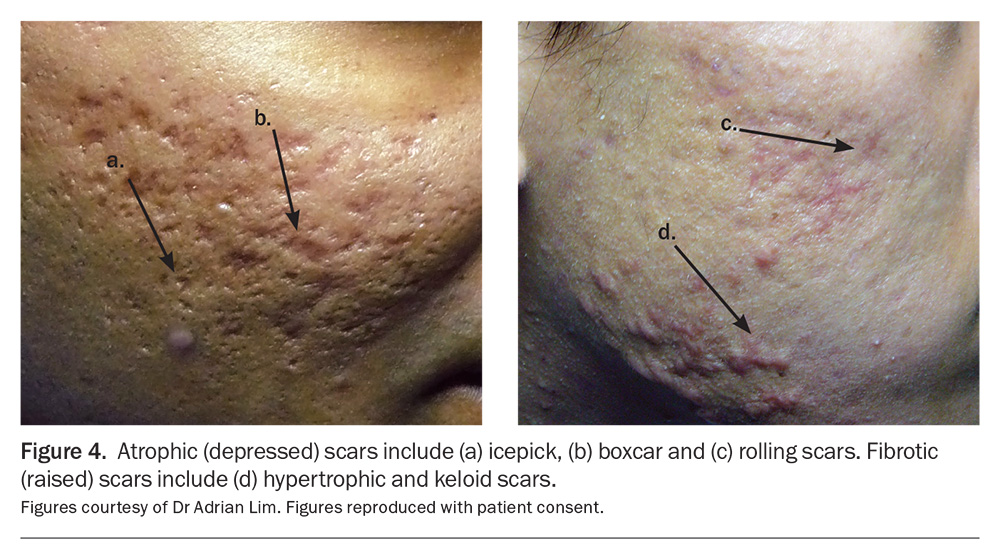
The management of acne scarring varies depending on the scar subtype (Figure 4). Although certain aspects of acne scar treatment, such as microneedling and radiofrequency therapy, are often performed by allied health professionals (e.g. nurses and dermal clinicians), referring patients to a dermatologist specialising in acne scarring can be highly beneficial. A specialist assessment enables a comprehensive treatment plan that incorporates a systematic approach, advanced techniques (as detailed below) and personalised treatment settings to optimise patient outcomes.
Treatment for hypertrophic versus atrophic scars
Hypertrophic and keloid scars are typically treated with intralesional corticosteroid injections, with or without the addition of 5-fluorouracil. The addition of 5-fluorouracil can be particularly beneficial for more resistant keloid scars and may help reduce the risk of steroid-related skin atrophy. Vascular laser treatments, such as pulsed-dye laser therapy, can be helpful as an adjunctive treatment, particularly to manage associated erythema and telangiectasias.
Atrophic scarring requires a thorough assessment of scar morphology and depth to guide treatment selection. The initial focus is often on addressing the deepest scars. Subcision, a surgical technique that most commonly uses a specialised tri-bevelled needle, is used to release fibrous bands tethering the base of the scar. This allows for elevation of the depressed area of scarring. Deeper, isolated scars may benefit from punch techniques, including punch excision or punch elevation.10
For mild-to-moderate atrophic scarring, a range of resurfacing energy-based devices are available. Radiofrequency is particularly suitable for darker skin types. Both non ablative and ablative laser resurfacing can be effective. Microneedling is another option, particularly for milder scarring. These treatments are based on the concept of creating controlled microscopic zones of injury to stimulate collagen remodelling, ultimately improving skin texture.10,11
Advanced treatments
Additional specialised techniques include trichloroacetic acid chemical reconstruction of skin scars (TCA CROSS), which involves focal application of high-concentration trichloroacetic acid (commonly 70 to 100%) to individual icepick scars. Dermal fillers may also be used to correct volume deficits, either by targeting individual scars with the ‘tower technique’ or by treating broader areas of atrophic scarring.12
An emerging approach involves transepidermal drug delivery. This can enhance healing and promote collagen remodelling through the application of growth factors, such as those found in platelet-rich plasma or insulin, following treatment with fractionated devices.13
Given the complexity of acne scarring, a multimodal treatment approach is often necessary to optimise outcomes. Although previous guidelines advised against cosmetic treatments in patients taking isotretinoin, this recommendation has evolved. With expert care by trained medical practitioners and individualised treatment settings, a range of interventions, excluding fully ablative laser and mechanical dermabrasion, can be safely performed.14
Early referral to a dermatologist specialising in acne scarring is key, ensuring comprehensive management of both active acne and residual scarring.
Conclusion
Scarring can occur in around half of patients with acne, even when the acne is mild. The risk of acne scarring and preventive measures should be discussed with all patients with acne. Treatment options for established acne scarring are varied and can be best facilitated by referral to a dermatologist to enable a comprehensive, multimodal approach, depending on the acne scar type. MT
COMPETING INTERESTS: Dr Gupta is a Board Member of the Australasian Society of Cosmetic and Procedural Dermatologists (ASCPD); is a Member of the All About Acne National Expert Team; and has received payment or honoraria for presentations from iNova and Pierre-Fabre. Dr See has received honoraria for consulting and speaking for Galderma, L'Oréal, SunPharma and Viatris; is co-chair of the All About Acne group and member of the Public Affairs Committee of the Australasian College of Dermatology.
References
1. Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol 2015 Jul; 172 Suppl 1: 3-12.
2. Liu L, Xue Y, Chen Y, et al. Prevalence and risk factors of acne scars in patients with acne vulgaris. Skin Res Technol 2023; 29(6): e13386.
3. Jennings T, Duffy R, McLarney M, et al. Acne scarring-pathophysiology, diagnosis, prevention and education: Part I. J Am Acad Dermatol 2024; 90: 1123-1134.
4. Goodman GJ. Post-acne scarring: a short review of its pathophysiology. Australas J Dermatol 2001; 42: 84-90.
5. Madu P, Kundu RV. Follicular and scarring disorders in skin of color: presentation and management. Am J Clin Dermatol 2014; 15: 307-321.
6. Tan J, Chien AL, York JP, Layton AM. Concerns, expectations, and management gaps relating to acne and associated scarring identified from survey data. J Drugs Dermatol 2021; 20: 600-606.
7. Harris DW, Buckley CC, Ostlere LS, Rustin MH. Topical retinoic acid in the treatment of fine acne scarring. Br J Dermatol 1991; 125: 81-82.
8. Dréno B, Bissonnette R, Gagné-Henley A, et al. Long-Term effectiveness and safety of up to 48 weeks’ treatment with topical adapalene 0.3%/benzoyl peroxide 2.5% gel in the prevention and reduction of atrophic acne scars in moderate and severe facial acne. Am J Clin Dermatol 2019; 20: 725-732.
9. Schleicher S, Moore A, Rafal E, et al. Trifarotene reduces risk for atrophic acne scars: results from a phase 4 controlled study. Dermatol Ther (Heidelb). 2023; 13: 3085-3096.
10. Renzi M, McLarney M, Jennings T, et al. Procedural and surgical treatment modalities for acne scarring: Part II. J Am Acad Dermatol 2024; 90: 1137-1150.
11. Boen M, Jacob C. A Review and update of treatment options using the Acne Scar Classification System. Dermatol Surg 2019; 45: 411-422.
12. Goodman GJ, Van Den Broek A. The modified tower vertical filler technique for the treatment of post-acne scarring. Australas J Dermatol 2016; 57: 19-23.
13. Pawar M, Singh M. Microneedling with autologous platelet-rich plasma versus microneedling with topical insulin in the treatment of postacne atrophic scars: a simultaneous split-face comparative study. J Am Acad Dermatol 2021; 84: 810-811.
14. Spring LK, Krakowski AC, Alam M, et al. Isotretinoin and timing of procedural interventions: a systematic review with consensus recommendations. JAMA Dermatol 2017; 153: 802-809.