Benign prostatic enlargement and lower urinary tract symptoms: an update on treatment
In recent years, the number of newer treatments for benign prostatic enlargement has increased dramatically. As a result, management of the condition requires a comprehensive, individualised approach and continual evaluation of treatment efficacy and patient preferences.
Correction
A correction for this article will be published in the July 2025 issue of Medicine Today. The online version and the full-text PDF of this article (see link above) have been corrected.
- Lower urinary tract symptoms (LUTS) are common among older men and often linked with benign prostatic enlargement, but they may not always correlate with prostate size.
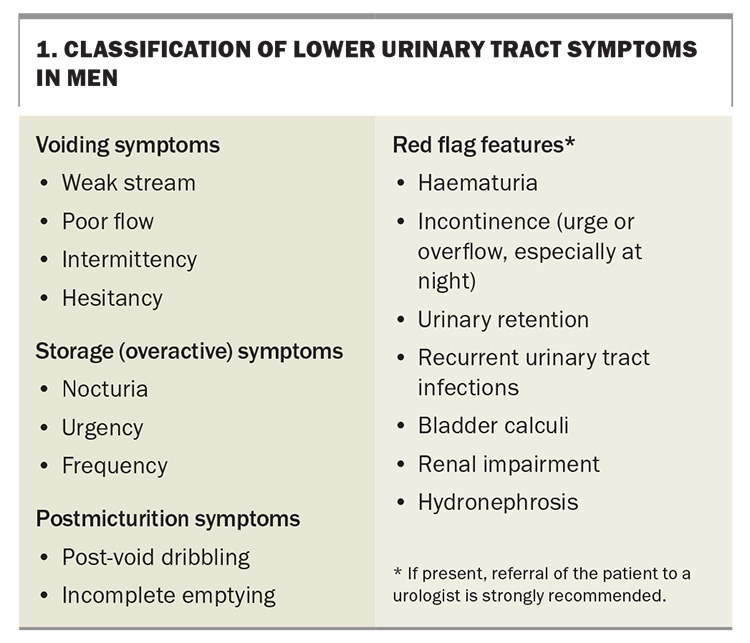
- LUTS are categorised into storage, voiding and postmicturition symptoms. These symptoms can significantly affect quality of life, leading to an increased healthcare burden.
- GPs play an important role in conducting a detailed patient history, physical examination and appropriate investigations to rule out other causes of LUTS.
- First-line treatment for LUTS often involves alpha-1 blockers for symptom relief. For patients with an enlarged prostate, 5-alpha reductase inhibitors may be considered to reduce the prostate size over time. Combination therapy may be considered.
- There are many surgical options available, and the choice is dependent on patient and disease factors, as well as patient wishes.
- Educating patients on dietary and lifestyle changes, including fluid management and behavioural modifications, can play a pivotal role in managing symptoms.
- Involving patients in their treatment decisions and discussing potential side effects and outcomes are vital for achieving satisfaction and adherence to therapy.
Lower urinary tract symptoms (LUTS) in men significantly affect their quality of life and have a significant economic impact on the healthcare system. Our new understanding of the lower urinary tract as a functional unit has shifted the focus to LUTS, away from the traditional emphasis on benign prostatic hyperplasia. Notably, this terminology is outdated, with the preferred terminology being benign prostatic enlargement (BPE).1
This article provides a comprehensive overview of LUTS in men and practical, evidence-based advice for assessing and treating non-neurogenic benign forms of LUTS. It is structured in a question-and-answer format, and the questions are based on queries often encountered by the authors in their everyday practice, from both patients and GPs encountering patients with LUTS. This article outlines key points in managing LUTS associated with BPE, including essential patient evaluation steps, ‘red flag’ symptoms to prompt early urologist referral, baseline investigations in primary care and an overview of medical and surgical treatment options available (including newer technologies). Through this discussion, we hope to equip healthcare providers with the knowledge needed to effectively counsel and treat men affected by this prevalent condition.
What are common LUTS?
As our understanding of BPE progresses, it has been recognised that it can lead to a variety of LUTS. These symptoms can manifest as either storage, voiding or postmicturition symptoms (Box 1).
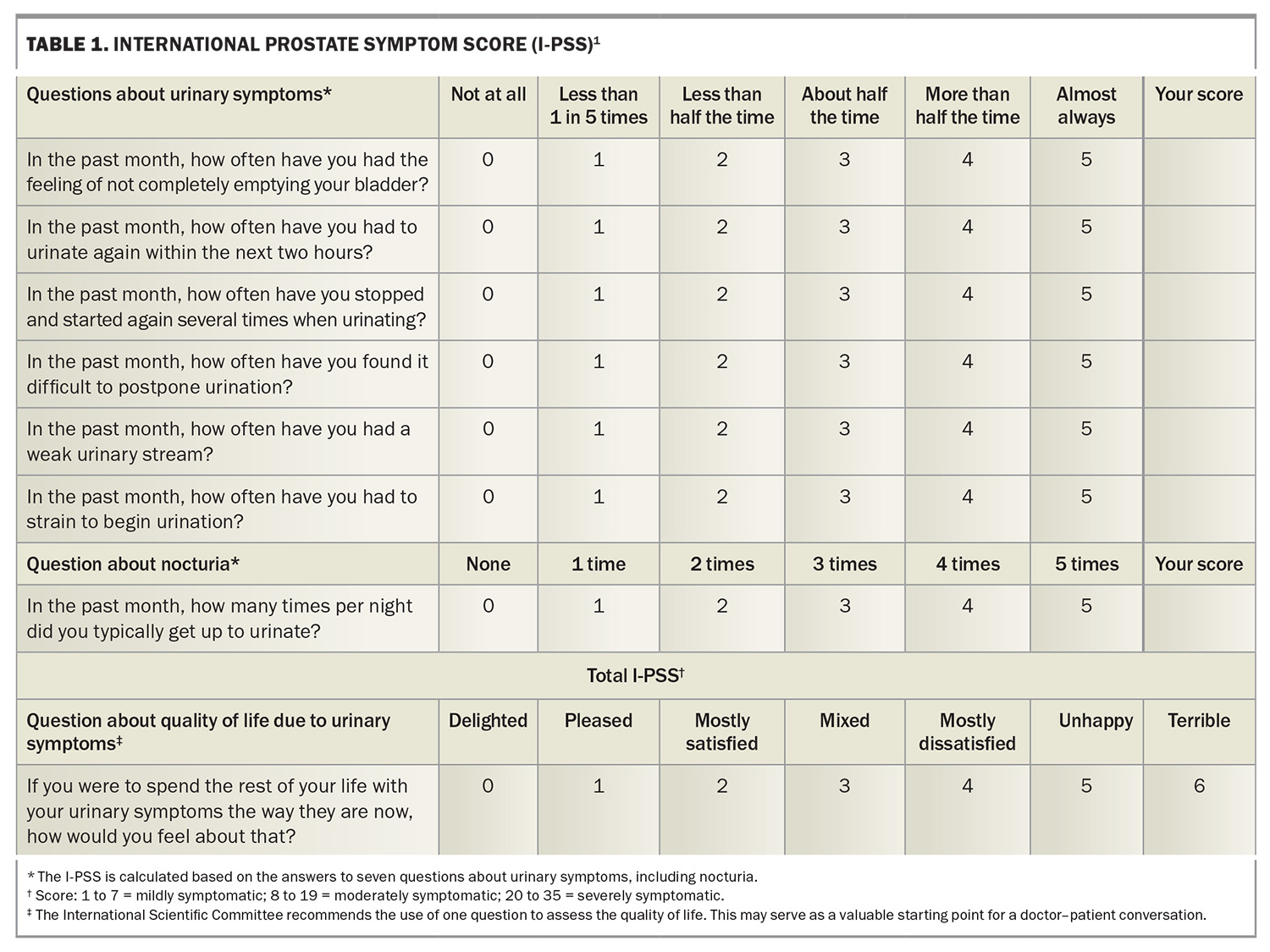
The International Prostate Symptom Score (I-PSS) continues to be a crucial tool for healthcare professionals (Table 1).2 This validated questionnaire not only helps evaluate the impact of BPE symptoms on patients but also identifies individuals who might benefit from therapeutic interventions. It can also be useful in tracking patient responses to treatment and highlighting key aspects of LUTS that may require a clinician’s attention.
How prevalent are LUTS?
LUTS are highly prevalent in the Australian population, affecting a significant portion of middle-aged and older men. Recent studies indicate that more than 50% of men in Australia older than 50 years of age experience some form of LUTS, with prevalence rates increasing with age.3
This is a major healthcare concern, given the ageing demographic in Australia. The impact of LUTS on quality of life can be profound, leading to sleep disturbances, stress and decreased daily functioning.1 As awareness grows, there is an increased emphasis within the Australian healthcare system on screening, early diagnosis and the management of LUTS to improve patient outcomes.
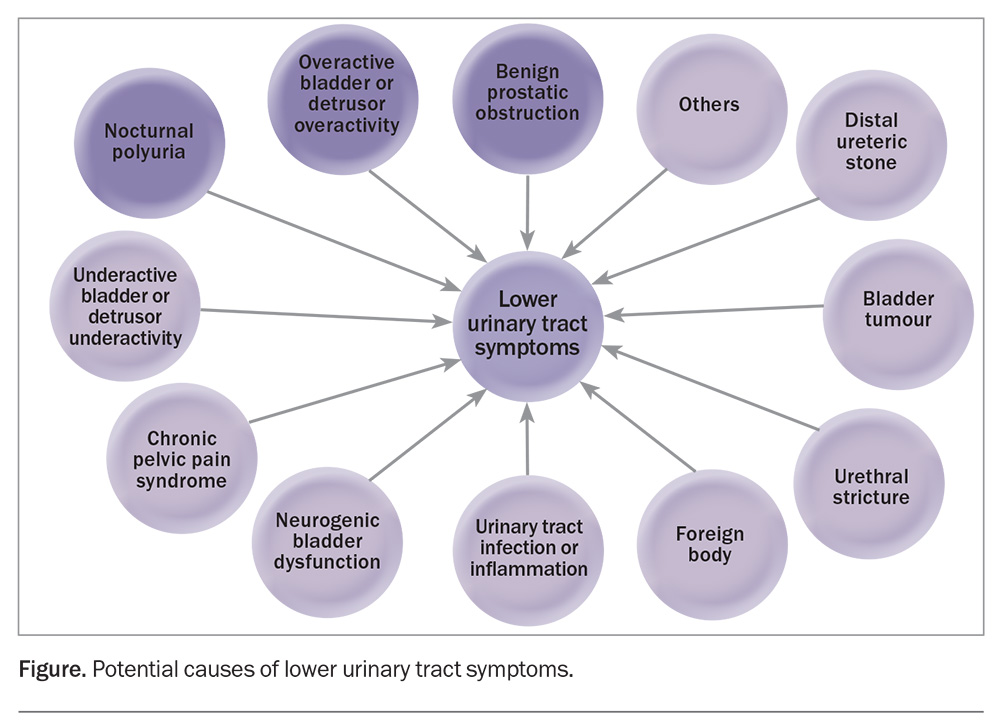
What causes LUTS?
The potential causes of LUTS are illustrated in the Figure.1
Are LUTS linked to other conditions?
LUTS are linked to several modifiable risk factors, indicating potential preventive targets, such as metabolic syndrome.4 Moreover, men with moderate to severe LUTS may face a heightened risk of experiencing major adverse cardiac events.5 Although LUTS, especially nocturia, may be associated with obstructive sleep apnoea (OSA), the nocturia is often a consequence of the OSA. Therefore, when the OSA is treated in such cases, the nocturia improves as well.
Are LUTS associated with prostate cancer?
LUTS are often associated with BPE, but very uncommonly with prostate cancer. In Australia, only a small proportion of men will have LUTS caused by prostate cancer. Nonetheless, it is important for men experiencing any urinary tract symptoms to seek evaluation and diagnosis from healthcare professionals. This underscores the importance of regular screenings and check-ups, particularly for those with a family history or other risk factors, to distinguish between BPE and prostate cancer.
LUTS can arise from various causes, with BPE being the most prevalent. Many men in Australia who present with LUTS do so because of concerns about prostate cancer. However, it is important to reassure patients that having LUTS does not increase their risk of prostate cancer compared with asymptomatic men.6,7
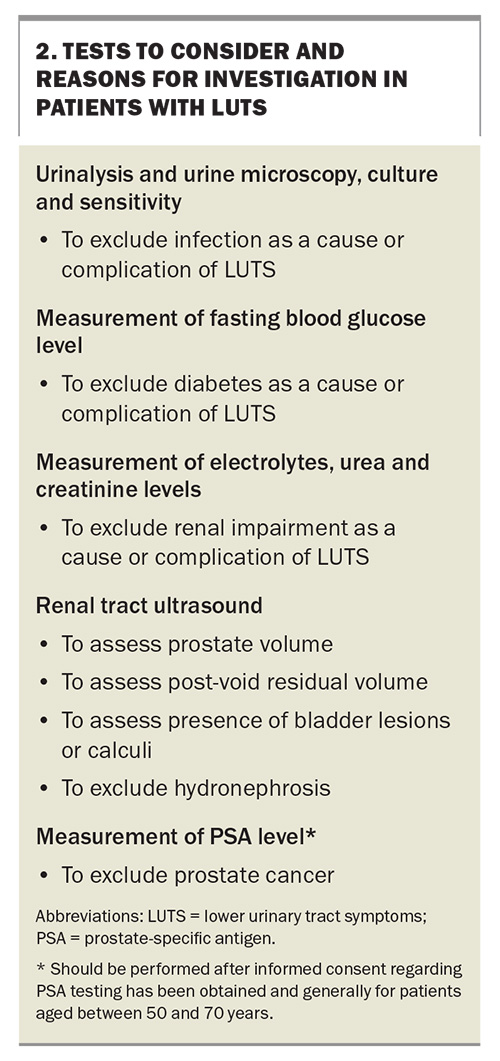
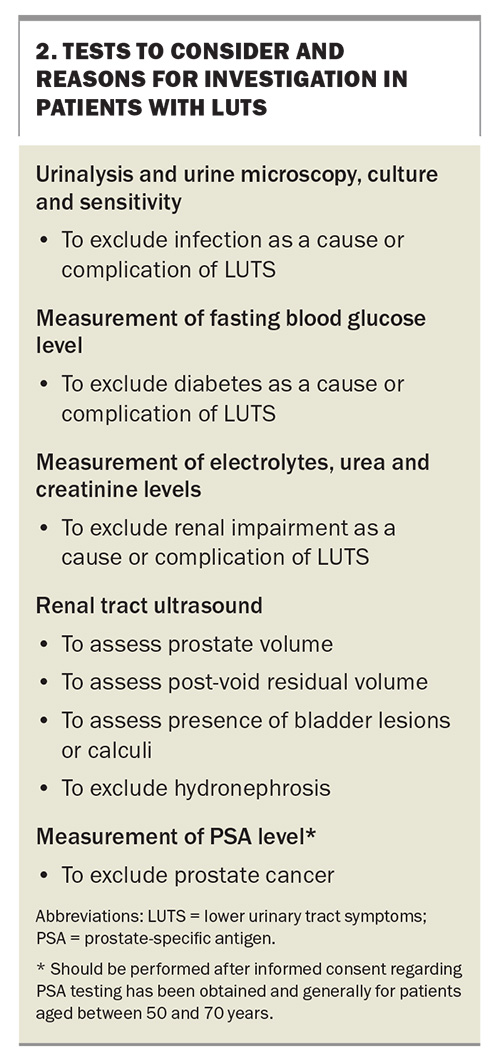
Which tests should a GP consider ordering for a patient with LUTS?
A list of tests that should ideally be conducted in the primary care setting for patients with LUTS is provided in Box 2. GPs may ask the patient to also complete a bladder diary over 48 to 72 consecutive hours to help distinguish between causes of LUTS (https://www.continence.org.au/resource/your-bladder-diary).
A prostate examination in general practice is controversial, but it may be helpful in detecting any prostate nodules and assessing the size of the prostate. We suggest that, at the very least, an examination of the patient’s foreskin be undertaken to exclude phimosis as a cause of the symptoms.8
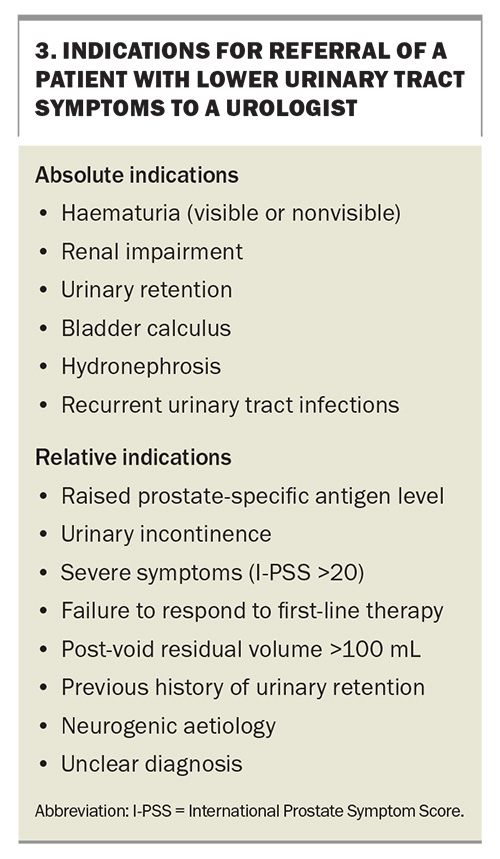
When should a patient be referred to a urologist?
In most cases, initial LUTS can be managed by a GP. However, a referral to a urologist may be necessary for further evaluation and treatment in the following cases:
- if there are other underlying medical conditions that may be contributing to the LUTS, such as bladder stones or urinary tract infections
- if the patient has significant complications from BPE, such as urinary retention, hydronephrosis or renal failure
- if the initial treatments are not effective in relieving symptoms
- if there is suspicion of prostate cancer based on abnormal prostate-specific antigen levels or physical examination findings.
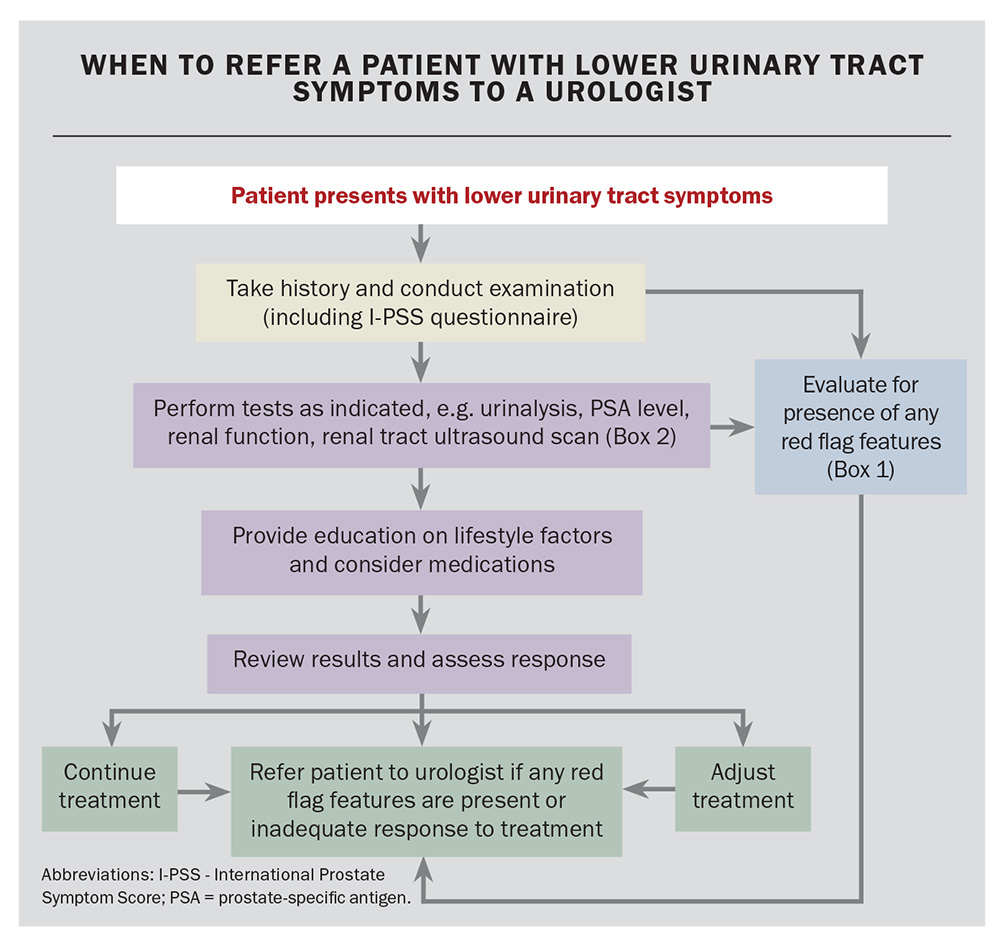
Patients should also be referred to a urologist if they are experiencing bothersome side effects associated with medications or if they desire surgical treatment options. Referrals to a urologist should be made in collaboration with the patient, ensuring their understanding and involvement in the decision-making process. Absolute and relative indications for a referral to a urologist are listed in Box 3. An overview of when to refer patients to a urologist is presented in the Flowchart.
What type of tests may a urologist order?
After the baseline tests (Box 2) have been performed, patients with LUTS may undergo a series of specialised tests. Some of these include a voiding flow study, urodynamics testing and cystoscopy or urethroscopy.
Voiding flow study
The authors strongly recommend extensive utilisation of voiding flow studies when accessible. This simple five-minute procedure is conducted in the clinic alongside a post-void residual bladder scan. It can aid in identifying whether an obstruction exists, distinguishing the type of obstruction (e.g. bladder outlet obstruction vs urethral stricture) and measuring the post-void residual volume. These results serve as a baseline measurement for evaluating a patient’s therapeutic response.
Urodynamics testing
Urodynamic testing, which assesses how well the bladder and urethra store and release urine, can be performed in the outpatient setting. It involves filling the bladder with water through a catheter while measuring the bladder pressure and recording the flow of urine. The test is indicated in patients who are suspected of having a neurogenic cause of LUTS, to assess bladder function and integrity or to determine the degree of bladder outlet obstruction more accurately.
Cystoscopy or urethroscopy
In this procedure, a cystoscope is inserted through the urethra into the bladder, allowing for direct visual examination of the interior lining of the bladder and urethra. This aids in identifying abnormalities such as strictures, tumours or stones. It is also used to assess the prostatic or bladder neck anatomy, which can help in choosing the best surgical treatment option for a patient with LUTS.
Which medication should be prescribed first in patients with LUTS?
General measures
Conservative measures for patients with LUTS include:
- fluid management: moderating caffeine consumption, restricting alcohol consumption and limiting fluid intake in the evening
- behavioural therapy: double voiding, urethral milking
- adjusting medication timing, such as avoiding diuretics in the evening in patients with nocturia
- addressing constipation.
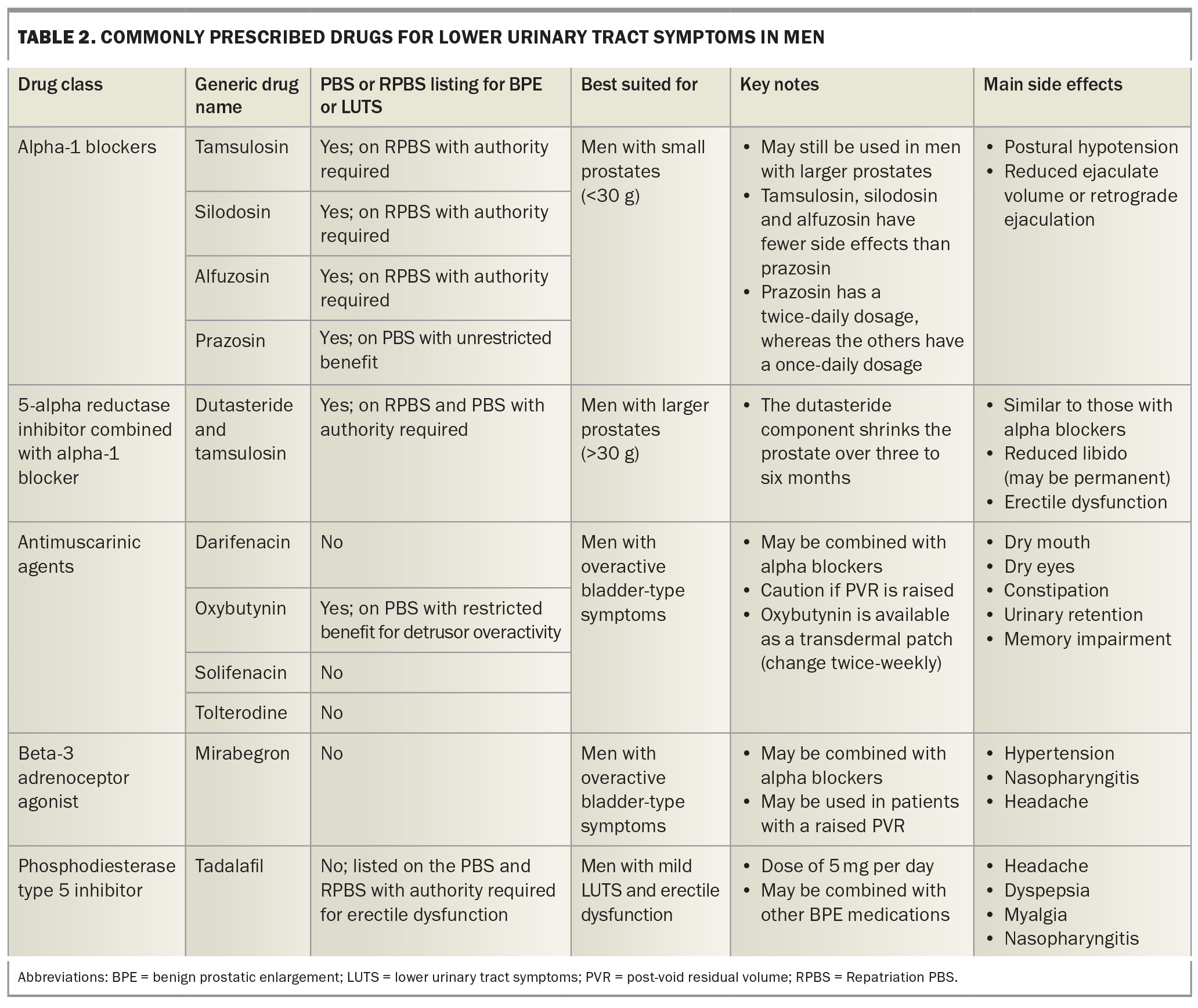
Medical treatment options
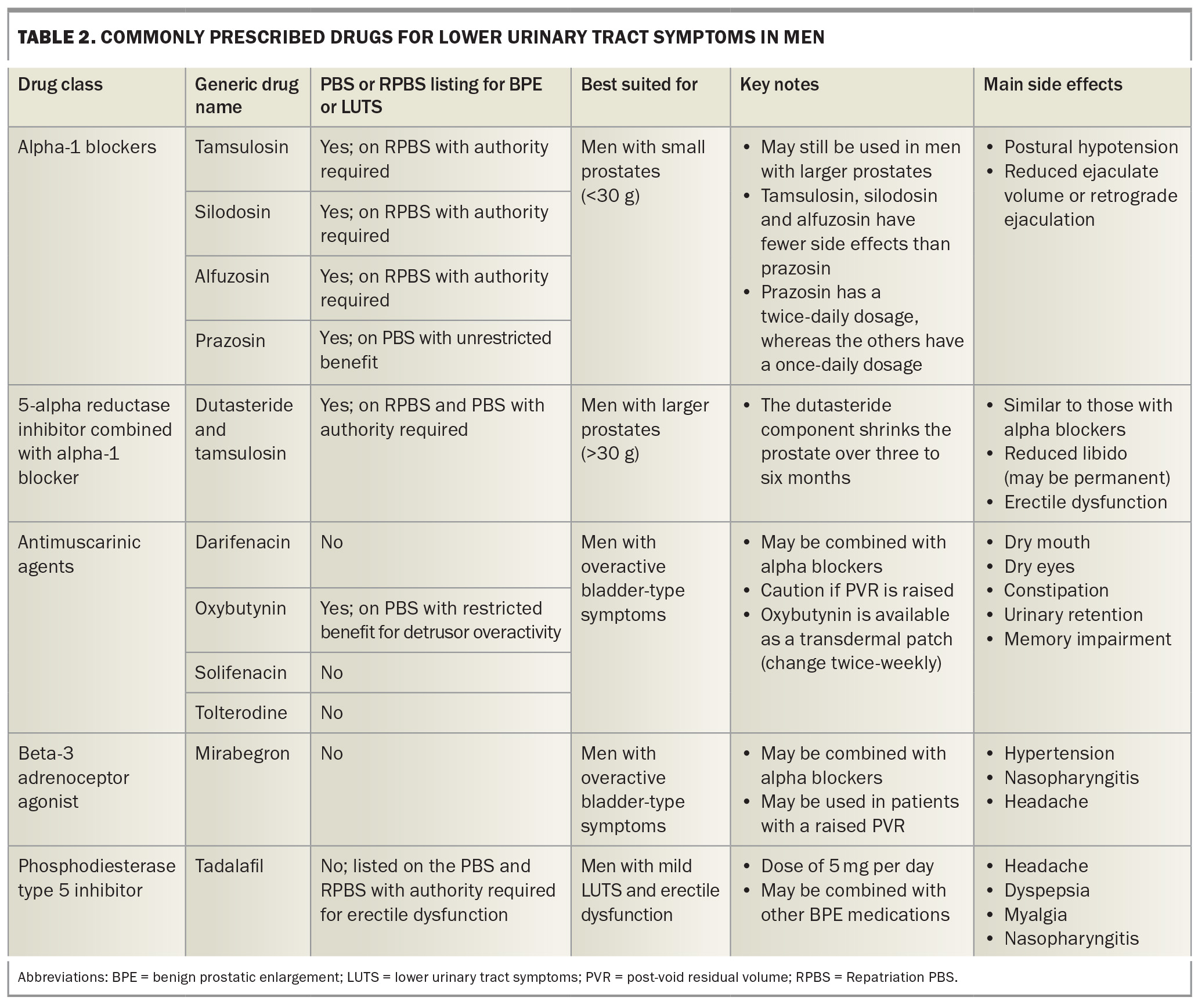
A failure to respond to conservative measures can lead to the consideration of medical treatment, which is generally indicated in patients with LUTS who experience bothersome symptoms, often indicated by an I-PSS greater than 7. Commonly used medications for men with LUTS are outlined in Table 2. Understanding different drug classes helps in selecting the most suitable medication for each patient. Some patients may benefit more from a combination of drugs from different classes rather than using them separately.
Alpha-1 blockers
Studies have shown that alpha-1 blockers (e.g. tamsulosin, silodosin, alfuzosin, prazosin) reduce the I-PSS by about 30 to 40% and increase the maximum flow rate by about 20 to 25%.9
Typically, the authors recommend tamsulosin 400 mcg daily as the first-line treatment for men with LUTS. This medication is well tolerated, confers minimal side effects and offers a convenient once-daily dosage. An alternative treatment is silodosin. Tamsulosin has a lower incidence of retrograde ejaculation, whereas silodosin has the advantage of being available in two strengths: 4 mg (half strength) and 8 mg (full strength). In Australia, tamsulosin is available on the Repatriation PBS (RPBS) but there are generic options with a cost of about $35–50 per month. Silodosin is also listed on the RPBS.
Alfusozin is another selective alpha-1 blocker that seems to have an efficacy similar to that of tamsulosin. It may be associated with an increased incidence of postural hypotension and a decrease in ejaculatory dysfunction. It is also only available on the RPBS or via a private script.
Prazosin is not recommended for LUTS as a first-line treatment as it is a nonselective alpha-1 blocker with increased side effects. Its main advantage is that it is PBS listed, so it may be cheaper than the other alpha-1 blockers.
5-alpha reductase inhibitors
Recent studies have looked at combining alpha-1 blockers with 5-alpha reductase inhibitors (5-ARIs; e.g. dutasteride) and have achieved varying results, although they have revealed an improvement in symptoms and quality of life. After two to four years of treatment, 5-ARIs improve the I-PSS by about 15 to 30%, decrease the prostate volume by 18 to 28% and increase the maximum flow rate by 1.5 to 2.0 mL/s in patients with LUTS caused by prostate enlargement.10 5-ARIs can also prevent disease progression with regard to acute urinary retention and the need for surgery.11 Long-term data from studies have shown that combination treatment is superior to monotherapy to improve symptoms and maximum flow, and superior to alpha-1 blockers alone in reducing the risk of retention or need for surgery, especially for larger prostates.12,13
A combined formulation of dutasteride and tamsulosin can be used for patients with LUTS and prostate volumes greater than 30 cc, which may be cheaper per month than the individual medications, as it is available on PBS (under authority). Patients should be informed that dutasteride and consequently this combination may cause sexual dysfunction, including potentially low libido. In a minority of patients, these sexual dysfunctions may be permanent, even after cessation of the medication.
Antimuscarinic agents and beta-3 adrenoceptor agonists
Other medications used for LUTS are antimuscarinic agents and beta-3 adrenoceptor agonists (e.g. mirabegron), which are used to help with storage symptoms (Table 2).14-16 Mirabegron generally has better tolerance than antimuscarinics in terms of side effects.
Phosphodiesterase type 5 inhibitors
Tadalafil is the only phosphodiesterase type 5 inhibitor to be TGA approved for BPE. At a dose of 5 mg daily, it has been shown to improve LUTS in men with BPE in large meta-analyses.17,18 It is particularly beneficial for those with coexisting LUTS and erectile dysfunction. A combination of phosphodiesterase type 5 inhibitors and alpha-1 blockers can improve the I-PSS, but the magnitude of effect of clinical significance is low. This can be a useful combination in a patient with coexisting LUTS and erectile dysfunction.17
Herbal remedies
There is no substantial evidence to support the efficacy of herbal remedies in significantly improving LUTS. However, among the different options, there is some low-level evidence for saw palmetto.19
When should a patient be considered for surgery?
A surgical procedure should be considered for patients who meet the following criteria:
- the patient is experiencing complications of BPE, such as urinary retention, hydronephrosis or renal failure
- the patient wishes to discontinue medical treatment for reasons such as:
– ineffectiveness of current medications in alleviating symptoms
– adverse side effects associated with current medications
– financial burden or high costs related to ongoing treatment
– a preference to avoid long-term or lifelong medication dependency.
In such cases, surgery may offer a more definitive solution to manage their condition effectively.
Are there any new surgical options for men with BPE?
Surgical options for men with BPE can be divided into five categories:
- resection (monopolar or bipolar transurethral resection of the prostate [TURP])
- vapourisation (greenlight laser prostatectomy, Rezum therapy, Aquablation)
- nonablative techniques (UroLift procedure, iTind procedure)
- enucleation (robotic or open simple prostatectomy, holmium laser enucleation of the prostate [HoLEP])
- alternative ablative techniques (prostatatic artery embolisation).
Ultimately, the choice of surgical procedure will depend on individual patient factors, such as the size and shape of the prostate, the patient’s overall health and the patient’s preferences. The decision should be made in consultation with a urologist, who can provide expert advice and help weigh the potential risks and benefits of each option. It is important for patients to consider these factors and the possibility of postsurgery complications before making a decision.
Resection
TURP has been extensively studied, with long-term data demonstrating sustained improvements in urinary symptoms and quality of life. A meta-analysis of randomised controlled trials indicated that TURP remains superior to many alternative therapies in terms of symptom relief and flow rate improvement, although it carries a risk of complications such as bleeding and retrograde ejaculation.20,21
Vapourisation
Greenlight laser prostatectomy is similar to TURP but uses laser energy to vapourise the prostate. It is useful in men who must remain on antiplatelet agents or anticoagulants, or to limit the time these agents are withheld in the perioperative period.21 Greenlight lasers can be associated with irritative voiding symptoms in the recovery phase.
Rezum therapy uses a device to deliver steam to the prostate, which results in shrinkage of the prostatic tissue. This results in a significant reduction in the I-PSS, with studies affirming the therapy’s minimally invasive nature and rapid recovery time. Its main advantages are that it is associated with very low sexual side effects compared with those associated with TURP and it can be a day case procedure; however, it does not have the evidence-based durability of TURP.22 Although Rezum therapy can be undertaken as a day case procedure, patients are usually discharged with a catheter for five to seven days.
Aquablation involves a surgical robotic system using high-pressure water to remove prostate tissue. The procedure is performed transurethrally, with promising results. This procedure is not yet available in Australia, other than in trial settings.23
Nonablative techniques
The UroLift procedure, supported by several studies, has demonstrated durable symptom relief over five years. It confers a 0% chance of erectile dysfunction and retrograde ejaculation, which is the major benefit.24-26
The iTind is a new temporary prostatic stent that is placed for five to seven days. It has the advantage of minimal sexual dysfunction side effects. The iTind operation involves two day case procedures: one to place the stent in, and the other to remove it five to seven days later.27
Given that certain prostatic anatomical configurations may not be well suited to the Urolift or iTind procedures, a cystoscopy is usually necessary beforehand.
Enucleation
HoLEP has emerged as a comparable technique to TURP, with randomised trials showing similar efficacy but with reduced hospital stays and catheterisation times. It is particularly useful for larger prostates (>100 cc) and in patients on anticoagulation therapy.28,29 Owing to their complexity, HoLEP operations generally take longer than other BPE surgeries and can lead to a slightly higher incidence of incontinence.
Robotic simple prostatectomy, although being newer in the field, has shown promising outcomes in terms of efficiency and patient recovery in retrospective analyses and early clinical trials, making it a suitable choice for specific patient populations, especially those with very large prostates.29 Compared with an open approach, the robotic approach resulted in a shorter length of stay and less blood loss.30
Alternative ablative techniques
Prostatic artery embolisation is a technique initially developed to control prostatic bleeding that has recently gained favour as a minimally invasive radiological intervention designed to treat LUTS. This is mainly used as an option in patients who are not suitable for other operative measures, as it is not considered a routine treatment for men with LUTS.31
Conclusion
The management of LUTS and BPE requires a comprehensive approach tailored to individual patient profiles. Incorporating lifestyle modifications, pharmacological treatments and, when necessary, surgical interventions can effectively alleviate symptoms and improve quality of life. Continual assessment of treatment efficacy and patient preferences is essential, ensuring that management strategies remain aligned with evolving clinical needs and personal health goals. MT
COMPETING INTERESTS: None.
References
1. EAU Guidelines. Edn. Presented at the EAU Annual Congress Paris 2024. ISBN 978-94-92671-23-3.
2. Barry MJ, Fowler Jr FJ, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148: 1549-1557.
3. Martin SA, Haren MT, Marshall VR, Lange K, Wittert GA; Members of the Florey Adelaide Male Ageing Study. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol 2011; 29: 179-184.
4. Gacci M, Corona G, Vignozzi L, et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int 2015; 115: 24-31.
5. Gacci M, Corona G, Sebastianelli A, et al. Male lower urinary tract symptoms and cardiovascular events: a systematic review and meta-analysis. Eur Urol 2016; 70: 788-796.
6. Martin RM, Vatten L, Gunnell D, Romundstad P, Nilsen TI. Lower urinary tract symptoms and risk of prostate cancer: the HUNT 2 Cohort, Norway. Int J Cancer 2008; 123: 1924-1928.
7. Sriprasad S, Thompson PM. Are men with lower urinary tract symptoms at increased risk of prostate cancer? A systematic review and critique of the available evidence. BJU Int 2001; 87: 127-128.
8. The Royal Australian College of General Practitioners (RACGP). Guidelines for preventive activities in general practice. 9th edn, updated. East Melbourne, Vic: RACGP, 2018.
9. Michel MC, Mehlburger L, Bressel H-U, Goepel M. Comparison of tamsulosin efficacy in subgroups of patients with lower urinary tract symptoms. Prostate Cancer Prostatic Dis 1998; 1: 332-335.
10. Roehrborn CG, Siami P, Barkin J, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol 2010; 57: 123-131.
11. McConnell JD, Roehrborn CG, Bautista OM, et al.; Medical Therapy of Prostatic Symptoms (MTOPS) Research Group. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 2003; 349: 2387-2398.
12. Kaplan SA, Lee JY, Meehan AG, Kusek JW. Time course of incident adverse experiences associated with doxazosin, finasteride and combination therapy in men with benign prostatic hyperplasia: the MTOPS trial. J Urol 2016; 195: 1825-1829.
13. Roehrborn CG, Barkin J, Tubaro A, et al. Influence of baseline variables on changes in International Prostate Symptom Score after combined therapy with dutasteride plus tamsulosin or either monotherapy in patients with benign prostatic hyperplasia and lower urinary tract symptoms: 4-year results of the CombAT study. BJU Int 2014; 113: 623-635.
14. Burgio KL, Kraus SR, Johnson 2nd TM, et al. Effectiveness of combined behavioral and drug therapy for overactive bladder symptoms in men: a randomized clinical trial. JAMA Intern Med 2020; 180: 411-419.
15. Kim HJ, Sun HY, Choi H, et al. Efficacy and safety of initial combination treatment of an alpha blocker with an anticholinergic medication in benign prostatic hyperplasia patients with lower urinary tract symptoms: updated meta-analysis. PLoS One 2017; 12(1): e0169248.
16. Kaplan SA, Herschorn S, McVary KT, et al. Efficacy and safety of mirabegron versus placebo add-on therapy in men with overactive bladder symptoms receiving tamsulosin for underlying benign prostatic hyperplasia: a randomized, phase 4 study (PLUS). J Urol 2020; 203: 1163-1171.
17. Gacci M, Corona G, Salvi M, et al. A systematic review and meta-analysis on the use of phosphodiesterase 5 inhibitors alone or in combination with alpha-blockers for lower urinary tract symptoms due to benign prostatic hyperplasia. Eur Urol 2012; 61: 994-1003.
18. Liu L, Zheng S, Han P, Wei Q. Phosphodiesterase-5 inhibitors for lower urinary tract symptoms secondary to benign prostatic hyperplasia: a systematic review and meta-analysis. Urology 2011; 77: 123-129.
19. Russo GI, Scandura C, Mauro MD, et al.; European Association of Urology Young Academic Urologists (EAU-YAU) Men’s Health and Functional Urology Working Groups. Clinical efficacy of serenoa repens versus placebo versus alpha-blockers for the treatment of lower urinary tract symptoms/benign prostatic enlargement: a systematic review and network meta-analysis of randomized placebo-controlled clinical trials. Eur Urol Focus 2021; 7: 420-431.
20. Cornu J-N, Ahyai S, Bachmann A, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 2015; 67: 1066-1096.
21. Reich O, Gratzke C, Stief CG. Techniques and long-term results of surgical procedures for BPH. Eur Urol 2006; 49: 970-978.
22. Miller LE, Chughtai B, McVary K, et al. Water vapor thermal therapy for lower urinary tract symptoms secondary to benign prostatic hyperplasia: systematic review and meta-analysis. Medicine (Baltimore) 2020; 99: e21365.
23. Nedbal C, Castellani D, De Stefano V, et al. Will Aquablation be the new benchmark for robotic minimally invasive surgical treatment for benign prostatic hyperplasia? Eur Urol Focus 2024; 10: 581-593.
24. Roehrborn CG, Gange SN, Shore ND, et al. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L.I.F.T. Study. J Urol 2013; 190: 2161-2167.
25. Perera M, Roberts MJ, Doi SAR, Bolton D. Prostatic urethral lift improves urinary symptoms and flow while preserving sexual function for men with benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol 2015; 67: 704-713.
26. Tzeng M, Basourakos SP, Lewicki PJ, Hu JC, Lee RK. New endoscopic in-office surgical therapies for benign prostatic hyperplasia: a systematic review. Eur Urol Focus 2022; 8: 522-531.
27. Liu Y, Cheng Y, Zhuo L, et al. Impact on sexual function of endoscopic enucleation vs transurethral resection of the prostate for lower urinary tract symptoms due to benign prostatic hyperplasia: a systematic review and meta-analysis. J Endourol 2020; 34: 1064-1074.
28. Higazy A, Tawfeek AM, Abdalla HM, Shorbagy AA, Mousa W, Radwan AI. Holmium laser enucleation of the prostate versus bipolar transurethral enucleation of the prostate in management of benign prostatic hyperplasia: a randomized controlled trial. Int J Urol 2021; 28: 333-338.
29. Fuschi A, Al Salhi Y, Velotti G, et al. Holmium laser enucleation of prostate versus minimally invasive simple prostatectomy for large volume (≥120 mL) prostate glands: a prospective multicenter randomized study. Minerva Urol Nephrol 2021; 73: 638-648.
30. Sorokin I, Sundaram V, Singla N, et al. Robot-assisted versus open simple prostatectomy for benign prostatic hyperplasia in large glands: a propensity score-matched comparison of perioperative and short-term outcomes. J Endourol 2017; 31: 1164-1169.
31. Urological Society of Australia and New Zealand (USANZ). Statement on Prostate Artery Embolization & Benign Prostate Enlargement. Sydney: USANZ; 2021. Available online at: https://usanz.org.au/info-resources/position-statements-guidelines/prostate-artery-embolization---benign-prostate-enlargement (accessed May 2025).