Chronic subdural haemorrhage. Untangling the complexities
Chronic subdural haemorrhage (CSDH) is a common presentation in both the emergency department and in general practice. It is primarily a disease of the elderly that, if symptomatic, requires surgical evacuation. It is common for these patients to take anticoagulation or antiplatelet medication, which commonly delays surgery. Given the frequent multiple comorbidities, management requires careful discussion with the patient and family.
- Chronic subdural haemorrhage (CSDH) is a separate entity to acute subdural haemorrhage with different pathophysiology and management.
- Risk factors for CSDH are old age, recurrent falls, anticoagulation or antiplatelet medication and alcohol use.
- Just under half of the patients presenting with CSDH will be on anticoagulation or antiplatelet medication.
- Percutaneous twist drill, burr hole and minicraniotomy have been shown to have similar efficacy in the evacuation of CSDH.
- When deciding when to restart anticoagulation or antiplatelet medication in postoperative patients with a thromboembolic risk, the risk of recurrent haemorrhage must be weighed against the risk of a thromboembolic event while the medication is being withheld.
- Careful discussion with the patient and their family regarding the risks, benefits and expectations of surgery is key in the management of CSDH.
- Often CSDH can be managed conservatively as many collections will resolve without any specific intervention. In general, intervention is determined on clinical grounds.
- Medical therapy, such as corticosteroids, is not usually used to treat this condition.
- Recurrence/persistence of subdural collection is relatively common (more than 15% of cases), and most patients with CSDH need to be followed to resolution with imaging.
Picture credit: © GCA/SPL
Chronic subdural haemorrhage (CSDH) is predominantly a disease of the elderly.1,2 It is a collection of ‘old’ blood that has mostly or partly liquefied and has accumulated under the dura mater, between it and the arachnoid. It is important to make the distinction between acute subdural haemorrhage (ASDH) and CSDH. ASDH presents following severe trauma and often occurs in younger adults, whereas CSDH mostly occurs in the elderly, and head trauma is often occult leading to a delayed diagnosis (Box 1). ASDH is caused by structural brain injury, i.e. a burst temporal lobe, whereas CSDH results from tearing the veins on the surface of the cortex that drain into the dural sinuses.1
CSDH is thought to begin with a trauma to the bridging veins resulting in subdural haemorrhage.1,3 Migration of clotting factors liquefies the clot.4 It is widely accepted that the clot evokes an inflammatory response that creates a friable neovascular membrane. Recurrent microhaemorrhages occur within the membrane and create a cascade that causes progression of the CSDH.5 Occasionally the fluid is clear, identical to CSF. This is called subdural hygroma and rarely requires surgical management.4
Presentation and diagnosis
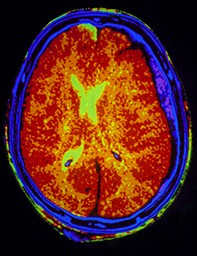
The diagnosis of CSDH can be difficult to make clinically because the presentation is insidious and occult head trauma is unrecognised by the patient and distant from the presentation.6 Symptoms are often non-specific and can range from mild headache or gait disturbance, to vertigo, confusion or focal neurological deficits including focal seizures, hemiparesis or dysphasia (Figure 1 and Figure 2).3,7 Reported head trauma is absent in one-third of cases.7,8 Further, CSDH may be found incidentally on brain imaging.
Non-contrast CT scan is a simple investigation that can clearly diagnose CSDH. It is the most sensitive for acute haemo-rrhage, easy to do and less costly than MRI.9
Although MRI is more sensitive than CT at delineating CSDH membranes, providing information regarding the brain parenchyma, and at diagnosing isodense CSDH, CT alone is sufficient in most cases.9
The two most common causes of cerebral atrophy are increasing age and chronic alcohol use. Cerebral atrophy stretches the bridging vessels in the subdural space and increases the risk of CSDH. The risk doubles with haematological diathesis, and anticoagulant or antiplatelet medications.1,7,10,11 CSDH can also be a rare complication of CSF over-drainage from a ventriculoperitoneal shunt.1,7,10,11
Transient neurological deficit
Transient neurological deficit can be a presentation of CSDH in up to 5% of cases and mimics transient ischaemic attacks.12,13 It is difficult to distinguish between the two in patients with transient neurological deficit when the CSDH is isodense and causes minimal mass effect.6 In this instance, a brain MRI should be performed in the first place to identify diffusion weighted changes indicating infarction. The carotid arteries should be also investigated for an embolic source.13
The aetiology is postulated to be due to epileptiform activity or compression of the cortical vessels resulting in transient cortical ischaemia.13 Evacuation of the CSDH is curative in most cases.12,13
Parkinsonism
Although rare, Parkinsonian symptoms, including rigidity, bradykinesia, tremor and postural instability, may develop in the context of CSDH.8,14 Reversal of Parkinsonism in patients with unilateral and bilateral CSDH is increasingly being reported in the literature.8,14 It is postulated that the mass effect from the CSDH in a susceptible patient with preclinical nigrostriatal dysfunction distorts the basal ganglia responsible for the movement disorder.14
Dementia
Alteration in mental state is another reversible manifestation of CSDH.15 Just under half of patients who present with a CSDH have a history of pre-existing confusion or dementia, making the diagnosis difficult.11 Generally, if the confusion is pre-existing for more than six months before the diagnosis of the CSDH, evacuation is unlikely to help.11 However, a non-contrast CT brain scan is an essential investigation in the workup for chronic confusion in the elderly, and a diagnosis of idiopathic or degenerative dementia should not be made until this is done.11
Cases in young adults
CSDH can also occur in young adults. This is discussed in Box 2.16-19
Management and outcome
Surgical intervention is considered in patients with CSDH when mass effect on the underlying cerebral cortex and midline shift causing symptomatology are present (Flowchart).2,11 Surgery is generally very successful in evacuating the clot and acutely resolving the patient’s symptoms.2 The three principle techniques neurosurgeons use to evacuate CSDH are twist-drill craniostomy, burr-hole drainage and mini-craniotomy drainage. Twist-drill craniostomy is less invasive with low morbidity whereas minicraniotomy drainage is more invasive with better visibility. Burr-hole drainage is somewhere in between.20
Minicraniostomy is commonly used to evacuate loculated CSDH because of the theoretical advantage of being able to perform a membranectomy.2,21 However, twist-drill craniosotomy and burr-hole evacuation are just as efficacious despite the presence of loculations with less morbidity. For recurrent/persistent CSDH, there is evidence in favour of minicraniostomy to prevent a third operation.2
Postoperative drainage systems decrease recurrence risk by more than half and are therefore common practice for neurosurgeons.2,22-24 No differences have been observed between subgaleal or subdural drain.24 Postsurgical bleeding related to removal has been rarely reported in postsurgery drainage systems.2 Neurosurgeons commonly leave the patient flat for 24 hours after surgery to allow the brain to come back to the convexity, but the evidence for this practice is not convincing.2
The use of antiplatelet and anticoagulation medications is increasing with the ageing population.25 Just under half of patients presenting with CSDH will be on antiplatelet or anticoagulation medication.26 This makes the decision of timing of surgery challenging. Generally, if the symptoms are minor, surgery should be delayed for one week if the patient is on aspirin, prasugrel or clopidogrel.26,27 If the patient is on warfarin, it may be reversed with vitamin K and/or fresh frozen plasma and/or prothrombin complex concentrate. Provided the International Normalised Ratio (INR) has normalised, surgery can safely proceed.28
If the patient is on the new oral anticoagulants (NOAC) such as dabigatran, rivaroxaban or apixaban, it is optimal for the surgery to be delayed for 48 hours after the cessation of these medications.27 If the patient rapidly deteriorates and the CSDH requires urgent vacuation, a higher bleeding risk is accepted. If the patient is on an antiplatelet, a platelet transfusion may be given.29 If the patient is taking a NOAC, prothrombin complex concentrate will be administered. Reversal agents for NOACs are in the pipeline.30
When it comes to medical management of CSDH, corticosteroid use is questionable and evidence is lacking.2 Moreover, prolonged use of corticosteroids may result in complications and is associated with higher morbidity than surgical evacuation.2 On this basis, if the CSDH is asymptomatic and/or small, only serial scans are required.31
Patient selection is one of the key factors in surgical management.7 Generally, as patients age, the risk of perioperative complications rises, mainly due to a higher rate of concomitant disease.3 For this reason, it is important to take a thorough history and have a careful discussion with the patient and their family regarding the risks, benefits and expectations of surgery.
By and large, the worse a patient presents, the less their chance of recovery, and the higher overall mortality rate.32,33 Hospital mortality in CSDH is about 15%, increasing to 26% and 32% at six months and one year, respectively.33 The recurrence/persistence rate of CSDH is significant, with a reported frequency of 15 to 30%.32,33 Risk factors for recurrence/persistence are advanced age, diathesis, brain atrophy, alcoholism, high-density haemorrhage and post-operative pneumocephalus.3,32
There is very little evidence about when to start patients back on antiplatelet or anticoagulation medication after CSDH.25 The risk of recurrent haemorrhage must be weighed against the risk of a thromboembolic event while the antiplatelet or anticoagulation medication is withheld.29 Current practice is variable and is generally a balance of the risks. It is recommended that the surgeon and GP prescribing these drugs collaborate to navigate a reasonable risk pathway.34 Generally, anticoagulation or antiplatelet therapy can be safely restarted three to four weeks after surgery if the progress CT is satisfactory. However, this decision must be tailored to the individual patient and may be restarted sooner in patients with a high thrombotic risk.35
Conclusion
CSDH occurs primarily in the elderly, in whom multiple comorbidities are frequently found. It may mimic other focal and global neurological conditions and should always be considered in differential diagnoses in the elderly. The presentation is insidious and is often characterised by headache and gait disturbance with focal neurology. Just under half of the patients presenting with CSDH will be on either anticoagulant or antiplatelet medication and this will often delay surgery. CSDH can atypically present as Parkinsonism or dementia. Awareness of these atypical presentations is important as these symptoms will resolve after an adequate intervention. CSDH can uncommonly occur in the young and requires vigilant investigation for specific causes. Evacuation can be achieved by twist-drill craniostomy, burr-hole evacuation or minicraniotomy, and there is no demonstrated superiority of any technique in the literature. Patients generally are restarted back on their antiplatelets or anticoagulants three to four weeks after surgery with a satisfactory CT scan. Recurrence/persistence rates are 15 to 30%. Careful discussion with the patient and their family about the risks, benefits and expectations of surgery is best practice. MT
References
154: 1549-1554.
5: 71-77.