New developments in COPD
COPD is a heterogeneous disease that presents many management challenges. This review presents an update on promising advances from research.
- Patients with chronic obstructive pulmonary disease (COPD) should be encouraged to maintain regular physical exercise, and referral to pulmonary rehabilitation is recommended.
- Inhaled corticosteroids should be reserved for patients with moderate to severe COPD to reduce exacerbations; and patients with a blood eosinophil count of 0.3 x 109/L or greater are most likely to benefit.
- Inhaled corticosteroids may be withdrawn safely in patients with COPD who do not have frequent exacerbations and have a blood eosinophil count of less than 0.3 x 109/L (excluding patients with an asthma overlap syndrome).
- Highly selected patients may be suitable for endobronchial valve placement or lung volume reduction surgery. Referral to a respiratory specialist and an expert centre is recommended.
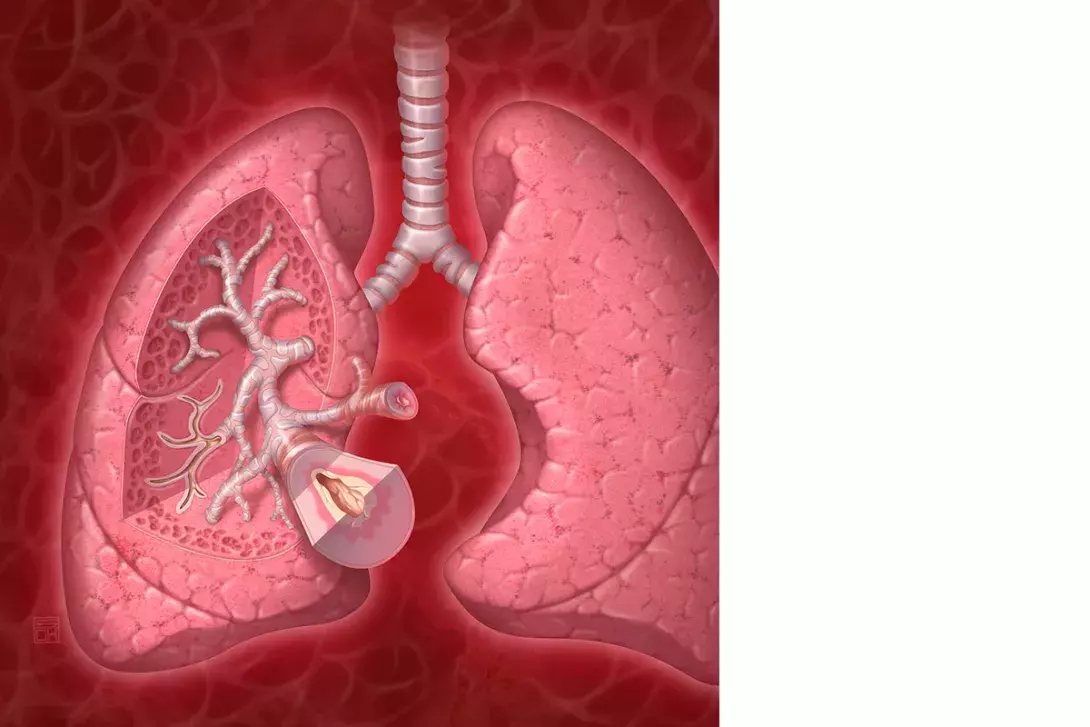
Chronic obstructive pulmonary disease (COPD) is characterised by fixed airway obstruction on spirometry, persistent respiratory symptoms including dyspnoea, chronic cough, wheeze or sputum production and a history of exposure to noxious stimuli, generally cigarette smoke.1 COPD was the fifth leading cause of death in 2015 and affects 5.2% of Australians aged over 45 years.2 Presentations due to COPD have a substantial impact on health service use, contributing to 1% of general practice encounters, and are the second leading cause of avoidable hospital admissions.3,4
The COPD-X guidelines are a useful resource for investigation, diagnosis and management of COPD.5 COPD should be considered in people aged over 35 years with a history of smoking or exposure to dust, gases or fumes. The diagnosis must be confirmed on spirometry with a forced expiratory volume in 1 second (FEV1) to forced vital capacity ratio of below 0.70.1 There is no evidence that COPD treatments have any benefit in patients without COPD diagnosed on spirometry. Smoking cessation is paramount to prevent further deterioration in lung function and symptoms. Other nonpharmacological interventions including annual influenza vaccination and referral to pulmonary rehabilitation are strongly recommended. For COPD patients with persistent symptoms or frequent exacerbations, a stepwise approach to inhaler therapy can be initiated (Figure 1).6
It has been identified that eosinophilic inflammation may play a role in COPD, and therefore may present a potential target for treatment options. Selected patients with severe COPD and persistent breathlessness despite optimal medical treatment may be suitable for advanced therapies including endobronchial valve placement or lung-volume reduction surgery. Frailty has been identified as a clinical syndrome and has significant impacts in patients with COPD. This review examines these three topics in further detail.
The role of eosinophils in COPD
Eosinophils are innate immune cells that are believed to play a role in host defences in allergic disease. Historically, eosinophilic inflammation in airways disease has been considered to be suggestive of asthma, with neutrophilic inflammation predominantly seen in COPD. However, over recent years there has been increasing interest in the role of eosinophilic inflammation in COPD including its impact on morbidity and the potential role for treatment targeting this form of inflammation.
A normal blood eosinophil count is less than 0.5 × 109/L. A blood eosinophil count of 0.3 × 109/L or greater, which may still be within the normal range, is associated with an increased risk of acute exacerbations of COPD.7,8 In 37 to 68% of people with COPD, blood eosinophil count was shown to be consistently 0.3 × 109/L or greater and to correlate with elevated levels of eosinophils in sputum.9,10 In a small retrospective cohort study undertaken in Canada involving 167 patients hospitalised with an acute exacerbation of COPD, an elevated blood eosinophil count at initial admission was associated with an increase in readmissions for exacerbations (odds ratio [OR], 3.59; 95% confidence interval [CI], 1.65-7.82]; p = 0.01) and an increase in all-cause readmissions over a 12-month period (OR, 2.32; 95% CI, 1.10-4.92]; p = 0.03). Patients with blood eosinophilia also had a shorter time to first exacerbation.11
Eosinophils have been proposed to be a useful biomarker in COPD for prognostic purposes and to guide treatment with inhaled and oral corticosteroids. It has been suggested that patients with COPD and elevated blood eosinophil counts (defined as ≥0.3 × 109/L) may benefit from inhaled corticosteroid therapy to reduce the risk of exacerbations; however, this has not been assessed prospectively in a randomised controlled trial.12,13
Withdrawal of inhaled corticosteroids (ICS) is safe in some patients with COPD, as shown by a randomised, double-blind, multicentre controlled trial involving 1053 patients with COPD who were receiving long-term triple therapy. Withdrawal of ICS to de-escalate to dual bronchodilator therapy with a long-acting muscarinic antagonist (LAMA) and long-acting beta agonist (LABA) in patients without evidence of eosinophilic inflammation was safe, with no difference in exacerbation rate over a six-month period compared with participants who remained on triple therapy.12 However, in patients with an elevated blood eosinophil count (≥0.3 × 109/L), ICS withdrawal was associated with an increased risk of exacerbations and a small decrease in lung function.
Data suggest that treatment with oral corticosteroids for acute exacerbations of COPD may also be directed by baseline blood eosinophil count. Retrospective analysis of three randomised controlled trials comparing prednisolone to placebo showed a higher rate of treatment failure in patients with an elevated blood eosinophil count of 0.3 × 109/L or greater who did not receive prednisolone, whereas in patients with a blood eosinophil count of less than 0.3 × 109/L there was no difference in treatment failure in the prednisolone group compared with the placebo group.14 However, in at least one of these trials, patients with a history of asthma were not specifically excluded. Asthma-COPD overlap is an increasingly recognised condition and corticosteroid treatment for acute exacerbations remains a key management strategy in patients with this condition.
The current evidence on the role of eosinophils in COPD is intriguing; however, the data are retrospective and based on post-hoc analyses. There are no current clear cut-offs for blood eosinophil count to guide management, and further prospective trials are required to determine the association and guide treatment recommendations.
Biologic therapy in COPD
The introduction of targeted biologic therapy in eosinophilic asthma has had a significant impact among patients with symptomatic severe asthma. Benralizumab and mepolizumab are humanised monoclonal antibodies that are administered subcutaneously and block interleukin-5, thereby reducing peripheral circulating eosinophils in blood and tissue.15,16 Mepolizumab significantly reduces exacerbation rates and symptoms and improves quality of life in patients with severe eosinophilic asthma.17
The data with regard to COPD are less clear. The METREX and METREO trials were multicentre, double-blind, placebo controlled parallel trials conducted over one year, predominantly involving patients with COPD who were symptomatic and had frequent exacerbations.18 In METREX, patients with an eosinophilic phenotype receiving mepolizumab 100 mg every four weeks in addition to triple inhaled therapy had a reduced rate of exacerbations and a longer time to first exacerbation compared with placebo, with no significant differences in lung function or quality of life scores. In METREO, all included patients had an eosinophilic phenotype and were randomised to receive mepolizumab 100 mg, mepolizumab 300 mg or placebo every four weeks in addition to triple inhaled therapy Interestingly, there was no significant difference in exacerbation rates between the groups (Figure 2).18
Benralizumab has been shown to significantly reduce exacerbation rates, improve lung function and reduce symptoms in patients with severe eosinophilic asthma.19,20 However, in the GALATHEA and TERRANOVA studies, in which over 2500 patients with COPD and a blood eosinophil count of 0.22 × 109/L or greater were randomly allocated to benralizumab or placebo, there was no significant difference in rates of acute exacerbations of COPD or hospitalisations over the 56-week follow-up period.21,22
At this stage, there is insufficient evidence to support the use of biologic therapy in patients with COPD. However, there may be some benefit in a subgroup of patients with eosinophilic inflammation, and further prospective trials are required.
Endobronchial valves
Insertion of endobronchial valves may be an option for carefully selected patients with severe COPD with an FEV1 of less than 50% predicted, hyperinflation with a total lung capacity of more than 100% predicted and residual volume of more than 175%.23 Valves are inserted via bronchoscopy and occlude emphysematous lobes to block inspiratory airflow while allowing expiratory airflow, with the aim of reducing gas trapping by creating areas of atelectasis and shunting airflow elsewhere.24
Retrospective analysis of the large early endobronchial valve trials showed that patients with intact pleural fissures were most likely to benefit.25 Several subsequent randomised controlled studies only recruited COPD patients with intact pleural fissures and have shown a significant improvement in FEV1, six-minute walk distance (6MWD) and quality of life in carefully selected patients.26-30 In a recent study, 40% of patients treated with endobronchial valve placement had a significant improvement in their 6MWD from baseline, and more than 40% of patients had a significant improvement in FEV1.29 In this study, improvements in FEV1, 6MWD and quality of life scores remained at 12-months.
However, it is important to recognise that there are potential major complications with endobronchial valve placement including pneumothorax (in 1.4 to 26% of patients) and COPD exacerbation (in 4 to 20% of patients).31 One recent study reported a 3% mortality rate within 45 days in the endobronchial valve group; however, a meta-analysis has shown no significant difference in mortality within a 12-month period.29,31
Endobronchial valves are not yet recommended as routine care. However, in highly selected patients with significant breathlessness despite optimised medical care and pulmonary rehabilitation, endobronchial valves may be a potential treatment option and patients should be assessed in a centre of expertise.32
Lung volume reduction surgery
Lung volume reduction surgery (LVRS) involves resection of emphysematous lung to decrease hyperinflation with the proposed benefits of improving diaphragmatic function, reducing respiratory muscle fatigue and intrathoracic pressure and improving cardiac ventricular filling.33-36
Patients with severe COPD who may benefit from LVRS include those aged under 75 years with persistent dyspnoea despite optimal medical treatment and pulmonary rehabilitation, who have heterogeneous emphysema (with varying emphysema tissue destruction between pulmonary lobes) and a 6MWD of greater than 140 metres.37
The National Emphysema Treatment Trial (NETT) was a large multicentre study involving 1218 patients with severe emphysema who were randomly allocated to either lung volume reduction surgery or standard medical care following completion of a pulmonary rehabilitation program.37 Patients in the surgical group had a significant improvement in exercise capacity, FEV and quality of life scores. There was an increased 90-day mortality in the surgical group (7.9% compared with 1.3%); however, there was no overall difference in mortality at the end of follow up (mean follow up, 29 months). A recent systematic review and meta-analysis – heavily influenced by NETT data – concluded that LVRS reduces gas trapping and significantly improves FEV1 and quality of life with an early increase in mortality but no difference in overall mortality.31 Postoperative complications included prolonged air leak.
LVRS may be a suitable treatment option for highly selected patients with severe COPD. Patients should undergo pulmonary rehabilitation before considering surgery and should be assessed in an expert centre with a multidisciplinary panel including a respiratory physician, thoracic surgeon, radiologist and interventional pulmonologist.32
Frailty and COPD
Frailty is a clinical syndrome in which there is a decline in physiological and functional reserve associated with increasing age, resulting in a reduced ability to cope with daily and acute stressors.38,39 Frailty affects 7 to 13% of the older population aged above 65 years with the prevalence increasing with advancing age.40-42 The syndrome is characterised by the presence of three or more of the following characteristics: loss of weight, slow walking speed, low physical activity, reduced grip strength and reduced endurance.40 The phenotype is useful for identifying people at risk of poor health outcomes and is an independent predictor of increased risk of falls, hospitalisation and mortality among the elderly population.40
People with COPD are twice as likely to be frail as people without the condition, with the prevalence of frailty ranging between 19 and 57%.39,42-45 Frailty in people with COPD has significant impacts, including increased risk of acute exacerbations and of readmission due to a new exacerbation episode during the 90 days after hospitalisation for an acute exacerbation of COPD.42,44 Furthermore, frailty in COPD is associated with worsening impairment of lung function, poorer exercise tolerance (including a reduced 6MWD), increased levels of depression and anxiety and low socioeconomic status.42,43,45 People with COPD and frailty are more likely to have multiple comorbidities, in particular cardiovascular disease.42
Exercise has been shown to improve frailty, and the addition of nutritional intervention is associated with further benefits.46,47 Although exercise appears to be an essential component in addressing frailty, the optimal exercise program has not yet been determined. Despite the benefits of pulmonary rehabilitation in patients with COPD being widely known, to date there have been no randomised controlled trials assessing the impact of pulmonary rehabilitation on frailty markers in COPD. A single centre prospective cohort study undertaken in the UK involving 816 patients with COPD and frailty showed that pulmonary rehabilitation improved exercise capacity, dyspnoea, hand grip strength, anxiety and depression. However, patients with frailty were also significantly less likely to complete pulmonary rehabilitation owing to either progression of their frailty or hospitalisation. Among the frail patients who persevered, 60% improved their frailty status to either prefrail or robust after completion of pulmonary rehabilitation.45
Increasing recognition of frailty among older adults and the population with COPD has highlighted the complex interplay between physiological, psychological and social factors. Although further data on effective exercise and nutritional interventions are needed, individuals at high risk of frailty may benefit from early identification and prompt referral to pulmonary rehabilitation.
Conclusion
Despite falling smoking rates in Australia, the burden of disease due to COPD remains substantial and has significant impacts on health care resources and utility.2 Although preventive health measures such as smoking cessation are vital, early identification and diagnosis of COPD is important to maintain lung function and prevent progression of symptoms. Both nonpharmacological and pharmacological interventions are recommended to reduce symptoms, prevent exacerbations and maintain lung function. Smoking cessation (beyond the scope of this article) is vital to prevent disease progression. Maintenance of physical activity and prevention of frailty is imperative in older adults with COPD and may improve their health outcomes. Further prospective studies assessing the impact of eosinophilic inflammation and targeted antieosinophilic treatments may be of benefit. In carefully selected patients with severe and persistent breathlessness in advanced COPD, advanced therapies including endobronchial valves or lung volume reduction surgery may be accessible. We recommend the COPD-X Guidelines as a useful resource to assist in identification, diagnosis and management of patients with COPD.5 MT
