Vaginal discharge – misconceptions, causes and treatments
Vaginal discharge is a common presentation to general practice. It is important to distinguish physiological discharge from that requiring further evaluation. Although the diagnosis and treatment may be straightforward, patients’ assumptions may be inaccurate, especially if there are concerns regarding sexually transmitted infections. The correct diagnosis can be missed if a full history and physical examination are not taken.
Correction
A correction for this article is published in the March 2020 issue of Medicine Today. The online version and the full text PDF of this article (see link above) have been corrected.
- Abnormal vaginal discharge is characterised by changes to the volume, odour, colour or consistency of a woman’s normal discharge, and may be associated with itch, pain, dyspareunia or abnormal vaginal bleeding.
- Bacterial vaginosis and vulvovaginal candidiasis are the most common causes of abnormal vaginal discharge.
- Providing effective treatment can be challenging in cases of recurring or chronic symptoms, and it is essential to ensure that predisposing factors are addressed.
- Consider sexually transmitted infections and pelvic inflammatory disease in those at risk. Missed diagnoses can increase risk of infertility, chronic pelvic pain and ectopic pregnancy.
- Other diagnoses include retained foreign body (e.g. tampon, condom), noninfective inflammatory disorders and genital tract malignancy.
Vaginal discharge is a common presenting problem in general practice. Patients may be embarrassed, and often attend with their own assessment as to the likely cause. Self-treatment can also confuse the diagnosis of recurrent symptoms. This article provides an approach to diagnosing and managing vaginal discharge in primary care.
Physiological vaginal discharge
Physiological vaginal discharge is formed from vaginal transudate, exfoliated epithelial cells and secretions from endocervical glands. The discharge varies throughout a woman’s menstrual cycle, from clear mucoid to thicker white discharge, in response to cyclical changes in progesterone and oestrogen levels. The amount of normal discharge varies between women, and may be affected by stress, pregnancy, sexual activity, intrauterine devices (IUDs) and hormonal medications.
Abnormal vaginal discharge
Abnormal vaginal discharge is characterised by changes in the volume, colour, odour or consistency of a woman’s normal discharge, and the causes could be infective or noninfective (Box 1). Further, presence of other associated symptoms (such as itch, pain, dyspareunia or irregular bleeding) is suggestive of pathological discharge.
Approach to the assessment of abnormal vaginal discharge
History
Vaginal discharge
- How is this different from the patient’s normal discharge (e.g. malodour, increased volume, colour, consistency)?
- When did it begin? Does it come and go? Is there a relationship to the menstrual cycle or sexual activity?
- Has it occurred before? What tests and treatments have been tried (including patient-initiated ones), and what was the impact?
Associated symptoms and signs
- Vulval itch, irritation, burning or discomfort
- Abnormal bleeding: postcoital or intermenstrual bleeding, postmenopausal bleeding or bloodstained discharge
- Abdominal, lower back or pelvic pain, or deep dyspareunia
- Urinary symptoms such as dysuria
- Genital ulceration or rash
- Systemic symptoms such as fever, nausea
Gynaecological and contraceptive history
- Cervical screening history
- Recent instrumentation, e.g. IUD insertion, surgical termination of pregnancy
- Is there a chance of pregnancy? Ask about contraceptive use and the last normal menstrual period
Sexual history
- Assess STI risk: condom use, sexual partners and practices, last sexual contact, past STIs, age under 30 years
General medical history
- Consider comorbidities, including chronic conditions, e.g. diabetes or immunosuppression
- Review medications, including corticosteroids, antibiotics, sodium-glucose cotransporter-2 (SGLT-2) inhibitors
- Ask about exposure to vulval irritants or allergens (Box 2)
- Personal or family history of atopy
Examination
When performing intimate examinations, always offer an observer, and advise that the examination can be stopped at any time if the patient wishes.
- Examine the vulva for signs of inflammation (erythema, swelling, fissures), and other dermatoses or ulcers.
- Perform speculum examination to visualise the vaginal walls and cervix (for erythema, friability, bleeding, fistulae, polyps, vaginal cysts and skin tags). Confirm presence of discharge (note colour, malodour, amount and, if possible, source). Check for foreign bodies.
- Abdominal examination and bimanual examination are indicated if there is pelvic pain or deep dyspareunia. Check for cervical motion tenderness, adnexal or uterine tenderness and any abnormal masses.
Bedside investigations in primary care
- Test the pH of vaginal discharge using a swab from the vaginal walls applied to narrow-range pH paper (pH 4 to 7). Bacterial vaginosis (BV) and Trichomonas vaginalis (Figure 1) infection are associated pH greater than 4.5 (normal vaginal pH is between 3.5 and 4.5) In addition, the pH can be affected by presence of semen, blood, lubricating jelly, and may be raised in atrophic vaginitis and desquamative inflammatory vaginitis.1
- Whiff test: amine or fishy odour noted on clinical examination.
Further investigations
- Low vaginal swab (if signs of vulvitis) or high vaginal swab for microscopy, culture and sensitivities (MCS). Presence of clue cells on vaginal secretion microscopy can support diagnosis of BV, and presence of yeast spores or hyphae can indicate candidiasis.
- Endocervical or high vaginal swab for chlamydia, gonorrhoea and T. vaginalis polymerase chain reaction (PCR) testing, if the patient is at risk of STIs. If the PCR test for gonorrhoea is positive, take a swab for culture and antibiotic sensitivity testing and give immediate treatment as per Australian STI management guidelines (Box 3).
- Swab for herpes simplex virus (HSV) PCR if ulcers, blisters or skin splits are seen.
- If there is evidence of PID or cervicitis, take an endocervical swab for Mycoplasma genitalium for PCR testing.
- Perform a co-test (human papillomavirus [HPV] and liquid-based cytology) for symptomatic patients with unexplained, persistent, offensive or bloodstained discharge.2
- Consider serology for bloodborne viruses according to risk: HIV and hepatitis A, B and C, depending on vaccination history and risk factors. Include syphilis serology.
Common infective causes of abnormal vaginal discharge
Common infective causes of vaginal discharge include bacterial vaginosis, candida and some sexually transmitted infections (Table).
Bacterial vaginosis
BV is the commonest cause of vaginal discharge. In Australia, it has been estimated to affect 12% of women, although a prevalence of 30% was found in a study of remotely located Indigenous women.3-5 Up to 50% of women are asymptomatic.4
The aetiology, microbiology and transmission of BV is not fully understood. It is a polymicrobial condition, associated with reduction in vaginal lactobacilli and overgrowth of anaerobic bacteria (including Gardnerella vaginalis). This leads to increased vaginal pH (greater than 4.5), and malodourous (‘fishy-smelling’) vaginal discharge, which may be more apparent during menses or after sexual activity. A thin, grey-white discharge is often seen and may coat the vaginal walls. Studies have shown a polymicrobial biofilm adherent to the vaginal epithelium in women with BV that is absent in controls. This biofilm is thought to possibly contribute to poor antibiotic penetration and difficulty re-establishing normal lactobacillus-predominant flora and normal vaginal pH.6 BV has been associated with adverse pregnancy outcomes including preterm birth, increased risk of acquiring some STIs (including HIV) and ascending infection causing PID following gynaecological procedures.4
Although not traditionally considered an STI, BV is associated with new or multiple sexual partners and lack of condom use, and is not identified in people who have never engaged in sexual activity.7,8 It is more common in women who have sex with women.9 It is also associated with vaginal douching. Clinical diagnosis is based on modified Amsel criteria, when three of the following four criteria are met:10
- homogenous, thin, grey-white vaginal discharge
- vaginal pH greater than 4.5
- positive whiff test/genital malodour
- clue cells on microscopy.
As point-of-care microscopy is not routinely available in primary care, diagnosis can be made based on the first three criteria, allowing for immediate treatment. In fact, one study concluded that using two of the Amsel criteria is as good as using three (sensitivity 61 to 69% and specificity 86 to 95%). The study suggested that if the vaginal pH is 4.5 or more, and one other criteria is positive (usually the presence of discharge typical of BV), the diagnosis of BV can be made.11
Although the diagnosis of BV may be supported by microscopy of the vaginal discharge showing clue cells, presence of coccobacilli and absence of lactobacilli, reliance on culture is not usually helpful in diagnosis or management of BV.11
Treatment is indicated for symptomatic women and for women undergoing invasive gynaecological procedures (such as surgical termination of pregnancy or IUD insertion). Evidence of benefit is lacking for screening and treatment of asymptomatic women in pregnancy. Early treatment (before 20 weeks’ gestation) can be considered for pregnant women with BV who are at high risk (previous preterm birth).12 There is insufficient consistent evidence to recommend partner treatment, although this is currently being investigated by an Australian trial.13
Prescribe oral metronidazole 400 mg or clindamycin 300 mg twice a day for 7 days. Metronidazole gel or clindamycin vaginal cream for 7 days can also be considered for symptomatic women who are not undergoing gynaecological procedures. Single dose (stat) treatments with antimicrobials are associated with higher recurrence rates, so are no longer recommended as first-line treatment. Tinidazole may be useful for women who do not tolerate the gastrointestinal side effects of metronidazole. For further details see the Australian STI management guidelines (Box 3).
Although recurrent BV is common, there is limited evidence regarding optimal treatment. It is unclear whether recurrences represent reinfection or persistence of bacterial pathogens because of poor biofilm penetration by antibiotics. Treatment options include metronidazole gel 0.75% twice weekly for 4 to 6 months after initial treatment, or oral metronidazole 400 mg twice a day for 3 days at the start and end of menstruation.4 Use of boric acid vaginal pessaries after nitroimidazole treatment has also been suggested, to assist with biofilm disruption.14 A new over-the-counter product, which contains a dendrimer in a vaginal gel, may be useful in women who do not wish to use antibiotic treatment options, but as yet there are limited clinical data available for this.
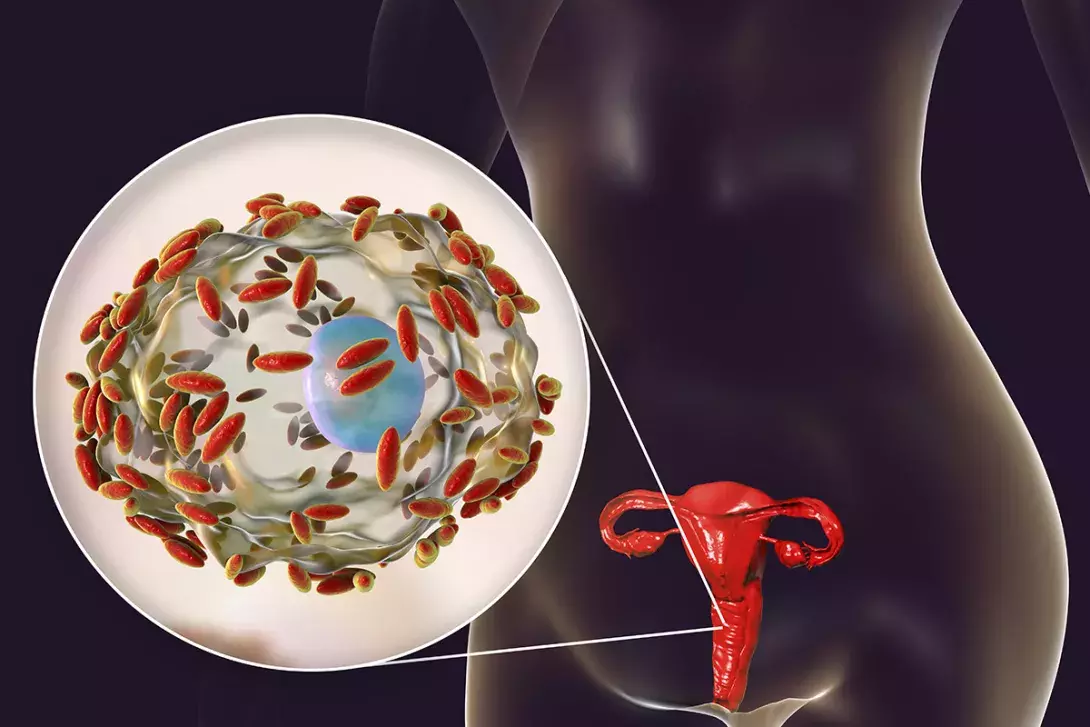
Vulvovaginal candidiasis
Vulvovaginal candidiasis (VVC) (Figure 2) is considered an overgrowth of commensal endogenous candida yeast in the vagina (from the bowel or vagina), and not an STI. Candida albicans is responsible for up to 90% of cases, and the remainder are caused by nonalbicans Candida species (predominantly Candida glabrata).4 VVC is common, with up to 75% of women experiencing an episode in their lifetime.15
Susceptibility to VVC generally requires tissues to be oestrogenised, hence VVC is rare in premenstrual and postmenopausal women, unless the woman is using hormone therapy.
Other risk factors include pregnancy, antibiotic use, immunosuppression and diabetes. Further, in patients with diabetes, use of SGLT-2 inhibitors is associated with additional risk of VVC.16 Women with diabetes have a higher rate of nonalbicans candida; therefore, taking a culture is an important part of management in this setting.
In addition to increased vaginal discharge, VVC often causes genital itch, soreness, superficial dyspareunia and/or dysuria. On examination, there is usually evidence of vulval and vaginal inflammation (skin erythema, oedema, fissures) and there may be the characteristic thick, white, adherent, ‘cottage cheese-like’ vaginal discharge. Vaginal pH remains less than 4.5.
Vaginal swab for MCS can confirm candida and identify the species responsible, and should be taken when there have been recurrent episodes of symptoms with poor response to standard topical azole preparations or oral antifungals.
Like BV, treatment is indicated if the woman is symptomatic; a positive culture result in an asymptomatic woman represents colonisation rather than pathology. Treatment of C. albicans can be with intravaginal azole creams (e.g. clotrimazole 10% as a single dose (stat), or a 3-day or 7-day course of 1% vaginal cream) or oral fluconazole 150 mg as a single dose (stat). If C. glabrata is identified, prescribe boric acid 600 mg vaginal pessaries from a compounding pharmacy, to be inserted at night for 14 days.17 Nystatin vaginal cream also has some effectiveness against nonalbicans candida.
Recurrent VVC is defined as four or more episodes of microscopically proven candidiasis per year.18 In chronic VVC, women experience a chronic, nonerosive, nonspecific vulvovaginitis, plus three to five of the following: positive vaginal swab for candida; soreness; cyclical symptoms (often exacerbated before menses, improvement with menses); dyspareunia; previous response to antifungal therapy; exacerbation with antibiotics; swelling; and vaginal discharge.
Ensure nonalbicans candida has been excluded. Also exclude diabetes, immunosuppression (including HIV) and broad-spectrum antibiotic use. The cause of recurrence is controversial. In otherwise healthy women, it has been suggested that chronic VVC may represent a hypersensitivity response to commensal candida rather than simple overgrowth.19
Treatment recommendations for recurrent VVC include initial intensive therapy (e.g. clotrimazole 1% vaginal cream for 7 days, or fluconazole 150 mg every 72 hours for 3 doses), followed by a weekly vaginal or oral antifungal as maintenance (e.g. clotrimazole 500 mg pessary or fluconazole 100 to 150 mg oral tablet) for 6 months. Higher induction and maintenance doses may be required for chronic VVC.20 Unfortunately, there is a high rate of relapse.21
Note that fluconazole treatment is not recommended in pregnancy.
Sexually transmitted infections
Abnormal discharge may also arise from STIs that typically cause vaginitis (T. vaginalis) or cervicitis (such as chlamydia, gonorrhoea or M. genitalium), or ulceration (HSV). Consider the diagnosis of PID if there are symptoms or signs of pelvic pain or deep dyspareunia.
T. vaginalis is discussed below. In the past, it was often detected in cytology samples in asymptomatic women having cervical screening. Testing for trichomonas now needs to be considered when examining women with vaginal symptoms as it is not detected by HPV PCR testing, which is now the initial cervical screening test. Detailed discussion regarding other STIs is beyond the scope of this article.
Diagnosis of an STI can cause significant distress and impact relationships, so it is helpful to provide supportive counselling and fact sheets. Advise avoiding sexual intercourse until 7 days after treatment completion, support contacting tracing and notify public health authorities if required. The Australian STI management guidelines and Australasian contact tracing guidelines provide further guidance (Box 3). Advise condom use, particularly with new partners, to prevent reinfection.
Trichomonas vaginalis
T. vaginalis is a sexually transmitted protozoan infection, more common in remote areas of Australia, in some Indigenous Australian communities and overseas.4 When a woman is symptomatic, the infection typically causes a profuse, frothy, malodourous, yellow-green vaginal discharge. There may also be vulval itch and soreness, and cervicitis. Males are usually asymptomatic but sexual partners should be treated concurrently. In general practice, trichmonas is best diagnosed via a PCR test on a high vaginal swab. First-line treatment is with oral metronidazole or tinidazole 2 g as a single dose (stat).17
Other causes of vaginal discharge
- Contact vaginitis and vulvitis – patients may not relate an allergen or irritant to their vaginal discharge. Careful history taking and examination are often required. Minimise exposure and consider mild topical corticosteroid ointment. See Box 2 for common irritants and allergens.
- Retained foreign body – a foreign body in the vagina (such as tampon or condom) may be present with a malodourous, coloured discharge and will be missed if a speculum examination is not performed. Discuss the need for emergency contraception in cases of retained condoms. Removal of the foreign body leads to resolution of symptoms. Antibiotics are not required unless testing finds pathogenic bacteria present.
- Atrophic vaginitis – occurs when there is a reduction in oestrogenisation of genital tissues (such as postmenopause or when breastfeeding). The vaginal walls and cervix become pale, less lubricated and elastic, and may bleed with contact. Treatment with topical vaginal oestrogens can be useful.
- Group B streptococcus is commonly isolated on vaginal swabs. It is a commensal organism in the gastrointestinal and genital tracts in up to 30% of healthy women. It is not generally considered pathological outside of pregnancy, when it can lead to neonatal infection. If there is symptomatic vulvovaginitis and Group B streptococcus is the only bacteria isolated, it can be treated with oral phenoxymethylpenicillin 500 mg twice a day for 10 days or clindamycin 2% vaginal cream for 7 to 14 nights.
- Desquamative inflammatory vaginitis (DIV) – consider after excluding other causes of vaginitis. DIV is an uncommon, poorly understood, chronic, noninfectious, inflammatory condition, often associated with pain and yellow discharge, with elevated pH. Seek specialist advice if DIV is thought to be the cause of persisting symptoms.
- Cervical polyps or ectropion – perform cervical screening and arrange gynaecological referral.
- Gynaecological malignancy – cancers such as those of the vagina, cervix and endometrium can present with abnormal vaginal discharge.
Conclusion
Abnormal vaginal discharge is a common symptom which can be effectively managed in general practice. Clinical examination is important for accurate diagnosis, testing and treatment. If, after evaluation and initial investigations, the diagnosis remains unclear or does not respond to treatment, consider further gynaecology or sexual health review. MT
