Skin and hair changes in menopause - it’s not just ageing!

Menopause can cause many symptoms, such as hot flushes and emotional changes; however, the skin and hair changes of menopause are rarely addressed. There are a range of topical and oral treatment strategies that can help women address these problems.
- Skin and hair symptoms are common in menopause; however, they often receive less attention than other symptoms, such as hot flushes and night sweats.
- GPs are perfectly placed to help inform women about these skin changes, why they occur and how they can be helped.
- Skin changes, such as dryness and wrinkles, may contribute to ageing and impact on quality of life.
- The plethora of skin and hair changes should form part of the holistic decision about whether to commence menopausal hormone therapy.
The skin is a large and dynamic organ that reflects various changes within an individual’s general health. This is particularly true for hormonal profile alterations seen during menopause because the skin, mucosa and hair follicles are heavily oestrogen dependent.1 Menopause is a mid-life event associated with decreasing oestrogen levels because of ovarian follicle depletion.2
The diagnosis of menopause
The diagnosis of menopause can be made without laboratory investigations in women aged over 45 years who have not menstruated for at least 12 months. This excludes women using hormonal contraception and women who do not have a uterus. For women aged younger than 40 years, the diagnosis of menopause is made following the detection of an elevated follicle- stimulating hormone level on two occasions four to six weeks apart.3
The median age of menopause is 51 years. It is often preceded by a perimenopausal period of several years. During this perimenopausal period of about two to eight years, symptoms can be variable. The transition from the perimenopause to menopause is influenced by genetics and environmental factors, such as nutrition, alcohol consumption and stress. Some women undergo a premature menopause, which can be secondary to ovarian failure caused by conditions such as autoimmune conditions. It may also be induced by removal of the ovaries, radiotherapy, chemotherapy and other conditions.3,4
Hormone changes during menopause
Menopause is associated with decreasing oestrogen levels because of ovarian follicle depletion. In premenopausal women, oestrogen production is predominantly ovarian; however, in postmenopausal women, it is from adipose tissue.5
Noncutaneous menopausal symptoms
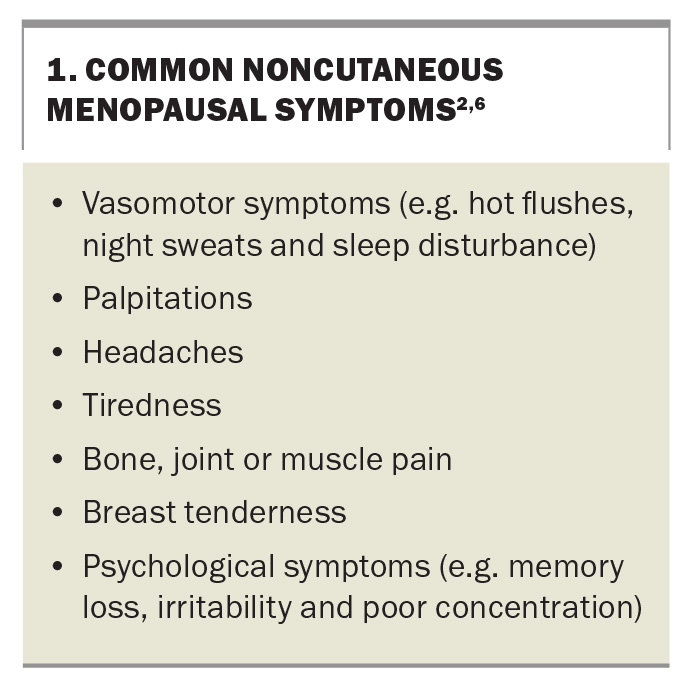
Many patients are unaware of how their body changes during menopause. Although this article concentrates on the skin and hair, it is important to list some other common symptoms that women experience (Box 1).2,6
Additionally, there are other health risks associated with menopause, including bone loss and osteoporosis, cardiovascular disease, diabetes, obesity and cognitive decline. Therefore, clinicians need to be aware of the diverse symptomatology that can occur, and be proactive in screening for and managing the early symptoms and signs with a holistic approach.
Skin and hair changes in menopause
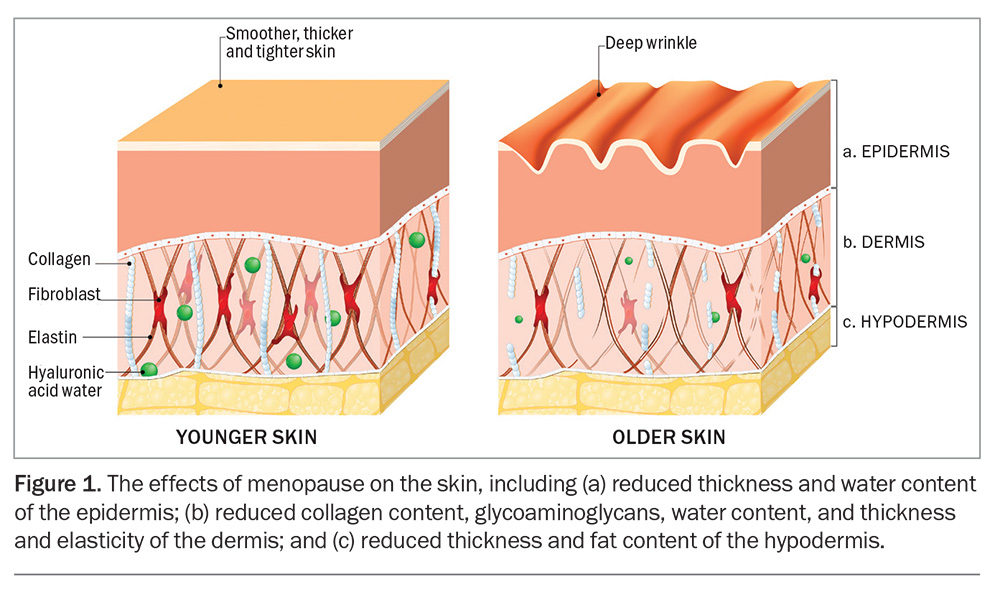
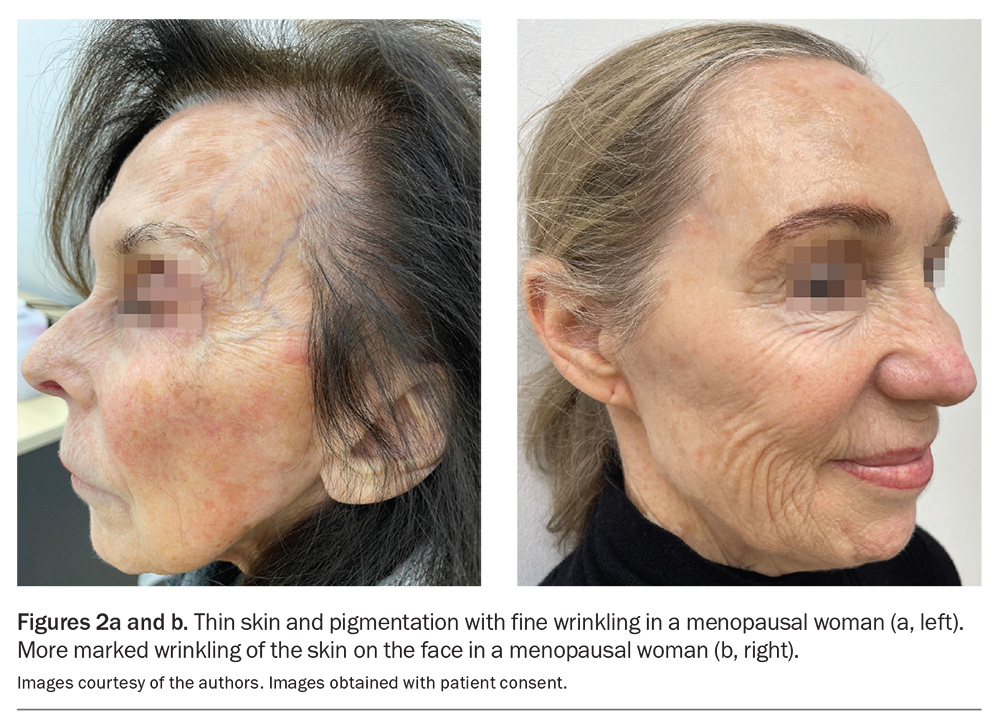
Skin and hair changes during menopause are often not discussed with patients and are merely considered an inevitable part of ageing. One study found that patients felt insufficiently informed about their skin changes.7 This underpins the need to educate both doctors and patients about skin and hair changes in menopause. The dryness, reduced thickness and increased wrinkling of the skin that may occur during menopause (Figure 1)
can contribute to the visible facial features of ageing (Figures 2a and b). These can often cause a negative effect on a woman’s quality-of-life, especially in a western society.1,2 There has been much confusion in the literature as to how much intrinsic ageing and photoageing contribute to the menopausal ageing.
These are some skin, mucosal and hair disorders that patients report to be more common during menopause, including:
- dryness, itch and dermatitis
- ageing skin with wrinkling and skin atrophy
- impaired wound healing
- acne and rosacea
- hyperhidrosis
- hirsutism
- female pattern hair loss
- frontal fibrosing alopecia
- flushing
- genitourinary syndrome (vaginal dryness, soreness, burning and itching, and urinary symptoms)
- genital dermatoses (e.g. lichen planus and lichen sclerosis)
- oral dermatoses (e.g. lichen planus, burning mouth syndrome and xerostomia [dry mouth]).1,2,8,9
Changes to skin and supporting tissues during menopause
Oestrogen is implicated in transepidermal water loss and reduced volume of collagen in the dermis because oestrogen receptors are very dense on the skin, especially on the face, genitalia and legs.1,2,6 About 30% of the collagen in a woman’s skin is lost during the first five years after menopause. Following this, there is a decline of 2% per year in the 15 years following menopause. Similar changes are seen in elastin, which likely contributes to the increased skin laxity and wrinkles that can be seen in postmenopausal women.
Skin dryness, itch and dermatitis
Menopause is commonly associated with xerosis, pruritis and eczema.10 It is necessary to maintain the skin barrier with gentle, nonirritating cleansers and moisturisers. Abrasive and perfumed products may also need to be avoided, and thicker moisturisers may be required once or twice a day, not just on the face, but also on the body and limbs, especially when the weather is dry and cold. Allergic contact dermatitis may occur, as well as asteatotic eczema – the most reported skin disease in menopausal women, caused by a loss of skin barrier function with increased transepidermal water loss.2,6
Psoriasis
Psoriasis data are insufficient and conflicting at times; however, in most cases, psoriasis is unchanged during and following menopause.
Postmenopausal acne
The pathogenesis of postmenopausal acne is currently unclear; however, it is believed to be caused by an imbalance of oestrogen and androgens, leading to a relative hyperandrogenic state. The same therapeutic ladder can be used for postmenopausal women experiencing acne as for the general population, consisting of topical treatments, antiandrogen therapy (e.g. spironolactone and cyproterone acetate) and isotretinoin.1,8
Hidradenitis suppurativa
It has been generally accepted that hidradenitis suppurativa improves with menopause; however, a large-scale study has shown that 40% of participants reported a flare of disease and 44% of participants reported no improvement in hidradenitis suppurativa after menopause.11 Menopausal hormone therapy (MHT) does not improve symptoms; however, antiandrogenic therapy appears to be clinically beneficial.12
Pigmentation
There is a well-known association between oestrogen and melasma, demonstrated by the disease exacerbations that can occur in pregnancy and with contraception use. Although some postmenopausal women experience melasma, there is no association with menopause itself.8
Keratoderma climactericum
Keratoderma climactericum is a thickening of the hands and feet, with the soles more severely affected postmenopause. Topical treatments can soften the skin, with options including topical oestradiol 0.05% and 25% urea cream.
Hyperhidrosis
Between 30 and 80% of postmenopausal women are affected by significant hyperhidrosis, which usually responds well to MHT. Other treatments include 20% aluminium chloride topically to the affected areas at nighttime, glycopyrronium 2.4% topically once daily and botulinum toxin injections.3 Oral treatment options include glycopyrrolate 1 to 2 mg three times daily or oxybutynin 2.5 to 10 mg once daily.
Hair changes during menopause
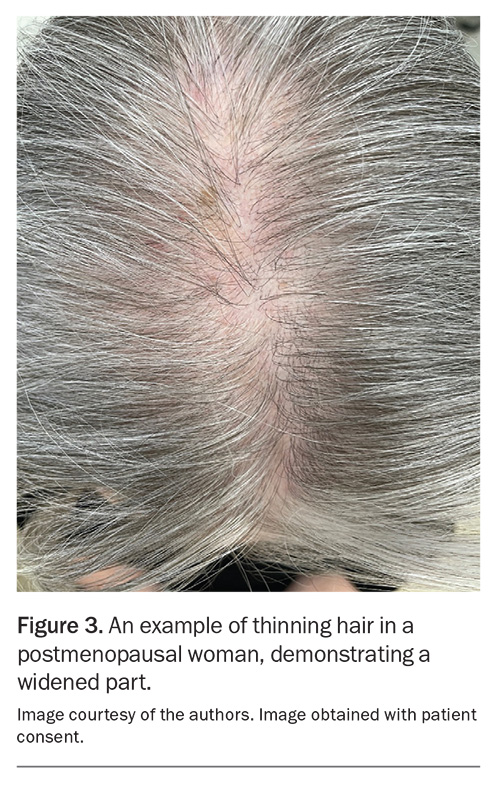
High levels of oestrogen promote anagen (the growth phase of hair). A reduced amount of hair in the growth phase has been measured in menopausal women, especially over the frontal scalp region.2 The relative increase in androgen levels can increase the density of facial, pubic and axillary hair, as well as reducing the density of scalp hair, leading to female pattern hair loss.
Female pattern hair loss
Although female pattern hair loss is more common in postmenopausal women, it is still important to screen for thyroid dysfunction (by measuring thyroid-stimulating hormone levels and levels of T3 and T4), anaemia (by measuring a patient’s full blood count) and iron deficiency (by conducting iron studies) when first assessing the patient.
Classically, the pattern of alopecia begins with hair density reduction on the midfrontal hairline. The anterior part width then widens, resulting in prominent thinning in a Christmas tree pattern (Figure 3). Generalised and rapid shedding with global hair thinning is unusual and points to other causes, such as hyperadrenalism, medication exposure, major stressors or a change in hair care practices.1,3,6,10,11 Hair loss over the temporal region is uncommon in female pattern hair loss, compared with male pattern alopecia. If temporal thinning is the first symptom, telogen effluvium, frontal fibrosing alopecia, tractional alopecia and hypothyroidism should be considered.2,13
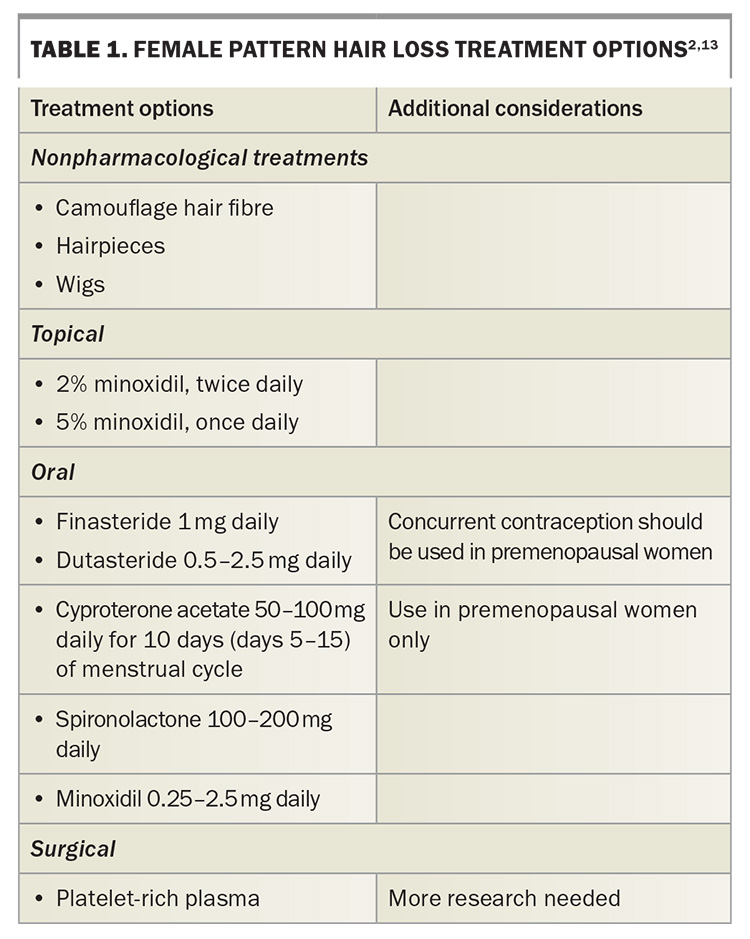
Common management options are listed in Table 1. Topical treatments are usually trialled first, prior to oral medications. There is insufficient evidence for recommending MHT for female pattern hair loss.
Senile hair fragility
Senile hair fragility occurs with increasing age. Patients should be encouraged to minimise their use of flat irons and other hot hair styling tools, regular hair colouring and hairstyles that twist or tug the shaft. The effects of MHT on senile hair fragility, which has a multifactorial pathophysiology, requires more research.
Frontal fibrosing alopecia
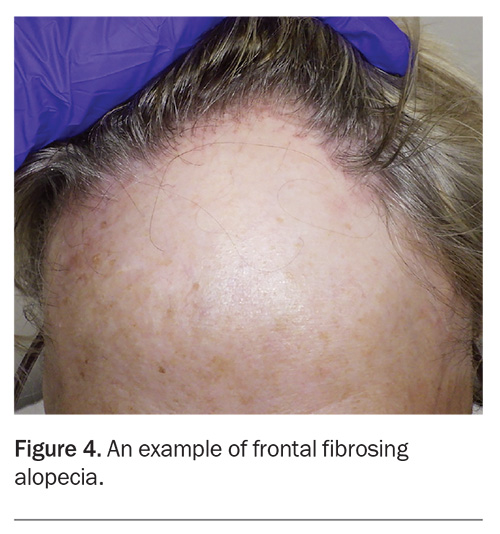
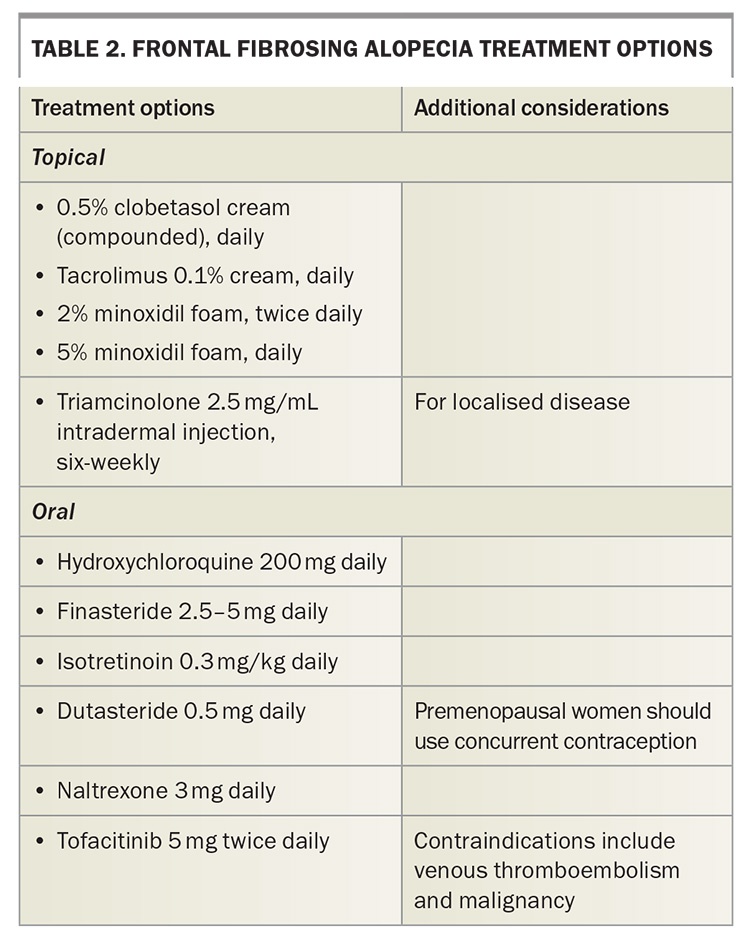
Frontal fibrosing alopecia is a scarring hair loss condition seen in perimenopausal women (Figure 4). It presents as progressive hair loss of the frontal hairline, accompanied by redness and scale around lonely hair shafts. As there is a lack of understanding about the precise aetiology, treatment options are aimed at preserving further hair loss, rather than promising regrowth.2 Treatment options are listed in Table 2.
Facial hirsutism
Facial hirsutism is common and seen in 50% of postmenopausal women. Investigations are not usually required; however, a normal serum testosterone level will exclude hyperandrogenism. Hair removal methods such as waxing, threading, epilation and the use of depilatory creams may be useful suggestions for patients. Topical eflornithine now needs to be compounded and used twice daily, making it an expensive treatment option. Oral spironolactone (at doses of 50 to 100 mg, once daily) may improve symptoms, in addition to epilation and laser hair removal.
Menopausal flushing
Most patients are aware of and, to a degree, tolerant of flushing as a symptom of menopause. However, if symptoms interfere with daily activities, the following are some of the potential treatment options that can be prescribed by GPs or specialists with an interest in menopause, such as gynaecologists.8,14 More information about MHT and nonhormonal treatments for menopausal symptoms can be found on the Australian Menopause Society website (https://www.menopause.org.au/images/pics/ptmm/a-practitioners-toolkit-for-managing-menopause.pdf).
Hormonal treatments
Hormonal treatment options include:
- oestradiol (oral or transdermal), in combination with progesterone for women who have a uterus
- tibolone (for postmenopausal women).
Nonhormonal treatments
Nonhormonal treatment options include:
- selective serotonin reuptake inhibitors (e.g. paroxetine 7.5 mg daily, citalopram 10mg daily or escitalopram 10 to 20 mg daily)
- selective noradrenaline reuptake inhibitors (e.g. venlafaxine 36.5 to 75 mg daily or desvenlafaxine 50 to 100 mg daily)
- gabapentin 300 to 900 mg three times daily
- pregabalin 10 to 50 mg three times daily
- fezolinetant 45 mg once daily.
Genitourinary effects of menopause
The vulva is rich in oestrogen receptors. The labia majora has fewer oestrogen receptors but more androgen receptors. The low oestrogen state of menopause leads to pubic hair loss, thinning of the skin, and loss of collagen, elastin and adipose tissue, as well as a more alkaline pH.
Genitourinary syndrome of menopause
The signs and symptoms of the low oestrogen state on the genitourinary system is collectively known as genitourinary syndrome of menopause. It is believed to affect up to 84% of all postmenopausal women. The symptoms include vaginal dryness, soreness, burning and itching. Urinary symptoms, including urinary frequency, urgency and stinging, can also be part of this syndrome. Clinically, there is atrophy of the labia and clitoris, as well as phimosis of the clitoral prepuce. This is a diagnosis of exclusion and there is no confirmatory testing.9,15
Treatments for genitourinary syndrome of menopause are as follows.
- Topical nonhormonal therapy:
– vaginal and vulval lubricants (water-based lubricants are preferred to minimise irritation)
– hyaluronic acid in the form of gel, pessary and vaginal tablets16 - Topical hormonal therapy:
– the mainstay of treatment for genitourinary syndrome of menopause: highly effective, especially for vulvovaginal atrophy
– recommended to be used daily for two weeks, then twice-weekly for as long as needed (expect response in three months); symptoms are likely to return on stopping the topical oestrogen therapy
– topical testosterone can also be used to help with dyspareunia and urinary symptoms.9,17
Systemic MHT and devices are effective but not approved for genitourinary syndrome of menopause alone. Laser and radiofrequency devices can help with symptoms by increasing collagen and elastin growth.9,18
Vulval skin conditions
Vulval skin conditions that are exacerbated by menopause include lichen sclerosus, lichen planus, irritant dermatitis and vulvodynia. Malignant and premalignant conditions also occur more frequently in postmenopausal women, including Bowen’s disease, extra-mammary Paget’s disease, vulval melanoma and vulval intraepithelial neoplasia. In women taking MHT, vulvovaginal candidiasis is more common than in women not on MHT.1,8,9,16
The role of MHT in menopausal skin and hair disorders
Several randomised and nonrandomised clinical trials have shown that both oral and transdermal MHT increases skin elasticity. Increases in skin thickness following oral and transdermal MHT have been shown to be less consistent across various trials.1 Holzer et al. showed that skin firmness was increased.19 MHT also reduces skin dryness. A systematic review by Pivazyan et al. demonstrated that MHT slows down the ageing process as it boosts collagen and elastin density, and skin firmness.1
MHT is considered to offer more benefits than disadvantages for women aged younger than 60 years who have had menopause for less than 10 years.1 However, there are no unequivocal data for its efficacy and safety in its use for the skin and hair effects of menopause and genitourinary syndrome of menopause. The wider potential benefits of MHT for hair, skin and mucosal symptoms, in addition to its potential risks, should be discussed with women so they can make an informed decision. Current data on the effect of MHT on hair quality and density are sparse.6
It has become a recent trend to apply topical oestrogen facial cream. In a review of 23 studies in which topical oestrogen was applied in various forms (e.g. gel, ointment, patch or cream), there were very few systemic side effects reported. There was one report of breast tenderness. Beneficial effects were seen in more than half of the participants, with increased collagen and elastin fibres at the site of application, as well as increased epidermal thickness and faster healing. It is prudent to note that some studies had concurrent administration of oral progesterone.20
Conclusion
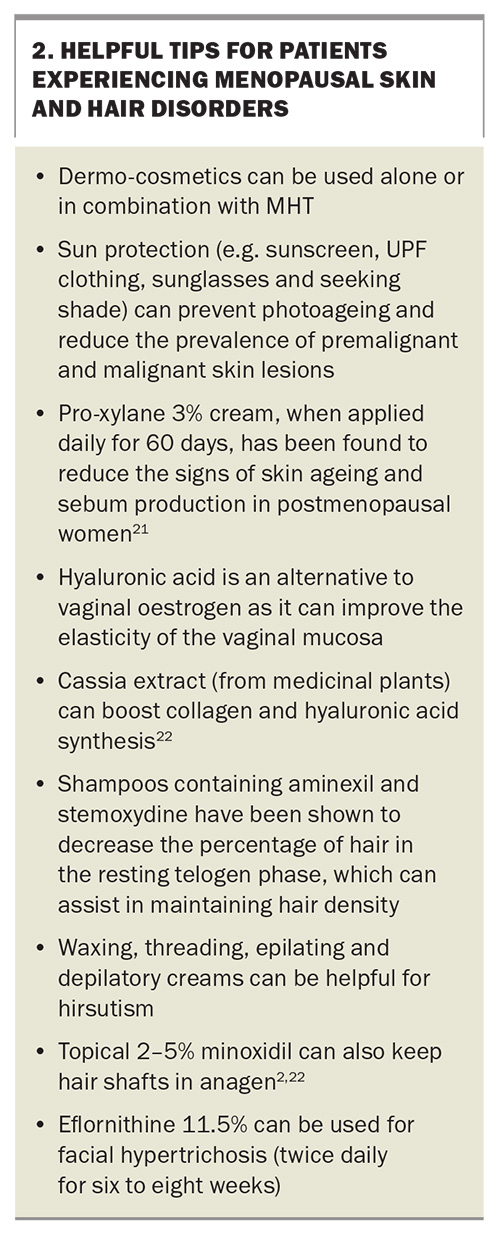
Menopause has a wide range of effects on hair and skin, beyond the expected effects of ageing. The symptoms and signs can vary, and should contribute to the discussion about treatments, including consideration of MHT. Helpful tips for patients experiencing menopause-related skin and hair disorders can be found in Box 2.21,22 MT
COMPETING INTERESTS: Dr See has received payment or honoraria from Viatris, Galderma, Sun Pharma and L’Oreal; support for attending meetings and/or travel from Galderma and L’Oreal; has participated on a Data Safety Monitoring Board or Advisory Board for Sun Pharma, L’Oreal and Galderma; and has had unpaid roles for All About Acne and the Australasian College of Dermatologists’ Public Affairs and Isotretinoin Advisory Committees. Dr Chan: None.
References
1. Pivazyan L, Avetisyan J, Loshkareva M, Abdurakhmanova A. Skin rejuvenation in women using menopausal hormone therapy: a systematic review and meta-analysis. J Menopausal Med 2023; 29: 97-111.
2. Kamp E, Ashraf M, Musbahi E, DeGiovanni C. Menopause, skin and common dermatoses. Part 1: hair disorders. Clin Exp Dermatol 2022; 47: 2110-2116.
3. Wines N, Willsteed E. Menopause and the skin. Australas J Dermatol 2001; 42: 149-159.
4. Nair PA. Dermatosis associated with menopause. J Midlife Health 2014; 5: 168-175.
5. Cui J, Shen Y, Li R. Estrogen synthesis and signaling pathways during aging: from periphery to brain. Trends Mol Med 2013; 19: 197-209.
6. Zouboulis CC, Blume-Peytavi U, Kosmadaki M, et al. Skin, hair and beyond: the impact of menopause. Climacteric 2022; 25: 434-442.
7. Leitch C, Doherty V, Gebbie A. Women’s perceptions of the effects of menopause and MHT on skin. Menopause Int 2011; 17: 11-13.
8. Kamp E, Ashraf M, Musbahi E, DeGiovanni C. Menopause, skin and common dermatoses. Part 2: skin disorders. Clin Exp Dermatol 2022; 47: 2117-2122.
9. Musbahi E, Kamp E, Ashraf M, DeGiovanni C. Menopause, skin and common dermatosis. Part 3: genital disorders. Clin Exp Dermatol 2022; 47: 2123-2129.
10. Aboobacker S, Saritha M, Karthikeyan K. A retrospective analysis of dermatoses in the perimenopausal population attending a tertiary care centre in South India. J Midlife Health 2015; 6: 115-121.
11. Fernandez JM, Hendricks AJ, Thompson AM, et al. Menses, pregnancy, delivery, and menopause in hidradenitis suppurativa: a patient survey. Int J Womens Dermatol 2020; 6: 368-371.
12. Kozera EK, Lowes MA, Hsiao JL, Frew JW. Clinical considerations in the management of hidradenitis suppurativa in women. Int J Womens Dermatol 2021; 7: 664-671.
13. Chan L, Cook DK. Female pattern hair loss. Aust J Gen Pract 2018; 47: 459-464.
14. Freedman RR. Menopausal hot flashes: mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol 2014; 142: 115-120.
15. The NAMS 2020 GSM Position Statement Editorial Panel. The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause 2020; 27: 976-992.
16. Lewis FM. Vulval symptoms after the menopause - not all atrophy!. Post Reprod Health 2015; 21: 146-150.
17. Fischer G, Bradford J. Vulvovaginal candidiasis in postmenopausal women: the role of MHT. J Low Genit Tract Dis 2011; 15: 263-267.
18. Alexiades M. Device-based treatment for vaginal wellness. Semin Cutan Med Surg 2018; 37: 226-232.
19. Holzer G, Riegler E, Hönigsmann H, Farokhnia S, Schmidt JB. Effects and side-effects of 2% progesterone cream on the skin of peri- and postmenopausal women: results from a double-blind, vehicle-controlled, randomized study. Br J Dermatol 2005; 153: 626-634.
20. Rzepecki AK, Murase JE, Juran R, Fabi SG, McLellan BN. Estrogen-deficient skin: The role of topical therapy. Int J Womens Dermatol 2019; 5: 85-90.
21. Bouloc A, Roo E, Moga A, Chadoutaud B, Zouboulis CC. A compensating skin care complex containing pro-xylane in menopausal women: results from a multicentre, evaluator-blinded, randomized study. Acta Derm Venereol 2017; 97: 541-542.
22. Limtrakul P, Yodkeeree S, Thippraphan P, Punfa W, Srisomboon J. Anti-aging and tyrosinase inhibition effects of Cassia fistula flower butanolic extract. BMC Complement Altern Med 2016; 16: 497.