What’s the diagnosis?
A woman with a painful, scaly nipple

Case presentation
A 58-year-old woman presents with an 18-month history of a scaly eruption on her right nipple. It is tender and mildly pruritic. The lesion has been unresponsive to treatment with a combination ointment containing triamcinolone acetonide, nystatin, neomycin sulfate and gramicidin.
The patient’s last mammogram and breast ultrasound, performed 12 months earlier, did not reveal any breast masses. She has a history of Hashimoto’s thyroiditis but is otherwise in good health. She has no history of atopy. Her father has had prostate cancer.
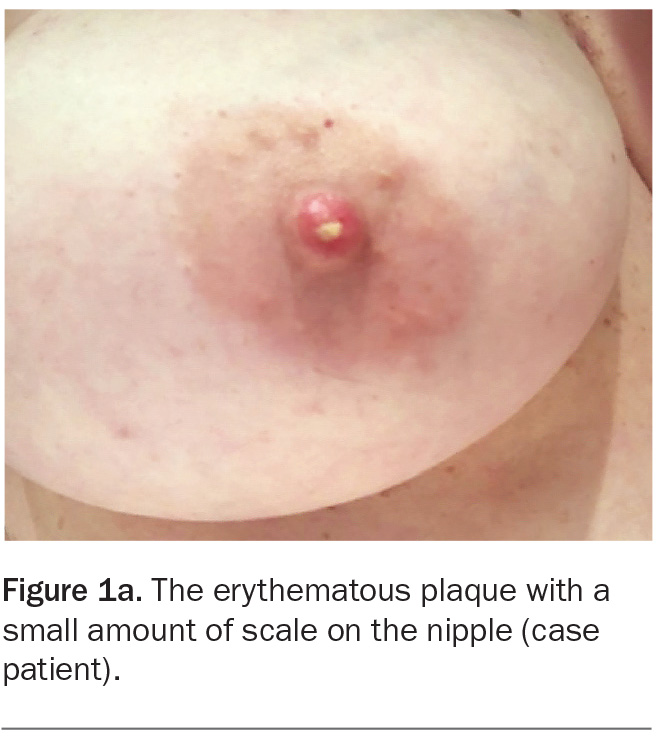
On examination, an erythematous plaque with a small amount of crust is observed on the nipple (Figure 1a). Erythematous round globules, pink structureless areas, dotted vessels and yellow scale are noted on dermoscopy (Figure 1b). There are no palpable masses on breast examination and no axillary lymphadenopathy.
Differential diagnoses
Conditions to consider among the differential diagnoses for a patient with a unilateral scaly eruption on the nipple include the following.
Eczema of the nipple and areola
Eczema of the nipple and areola, which may be unilateral or bilateral, mainly occurs in women but is occasionally seen in men.1 The condition has an intermittent course and is characterised by pruritus and eczematous changes with poorly defined margins.2 Nipple anatomy is preserved.
Eczema of the nipple has been associated with atopy, breastfeeding and contact allergens.3-7 Skin irritation caused by friction from undergarments may also cause nipple eczema (also known as jogger’s nipple and cyclist’s nipple).8,9 However, often no cause can be established.
For the case patient, a diagnosis of nipple eczema could be excluded. She has minimal associated pruritus and no history of atopy, and her symptoms are progressively worsening, not intermittent. In addition, her condition has not responded to topical corticosteroid treatment.
Nipple psoriasis
Psoriasis is a chronic inflammatory skin disease with an incidence of 1 to 3%.10 The scalp, extensors of the knees and elbows, and sacral area are the most commonly affected sites, but psoriasis can appear in atypical locations after trauma by the process of koebnerisation.11 Although very rare, there have been biopsy-proven cases of nipple psoriasis in breastfeeding women that have been provoked by the trauma of suckling.2
The case patient’s lesion is not consistent with nipple psoriasis, which would be expected to be marginated, scaly and pruritic. On dermoscopy, nipple psoriasis typically demonstrates uniformly distributed dotted vessels and white scales, which are not seen in this case.12 She has no other cutaneous signs of psoriasis.
Staphylococcal aureus infection
Pathological conditions caused by Staphylococcus aureus – an easily transmissible bacterium present in the anterior nares of up to 35% of healthy people in the community – are due to direct bacterial invasion through breaks in the skin.13,14 Infection is facilitated in areas that are kept moist and humid, which favours local multiplication of S. aureus.13 A traumatised and/or cracked nipple, especially after breastfeeding, provides an entry point for the bacterium, which may precipitate a deeper cellulitis, adenitis or mastitis.15 Puerperal mastitis is reported to affect 1.4% to 8.9% of nursing mothers presenting with general malaise, chills or sweats, and fever.16 However, half of patients will only have localised symptoms and signs of inflammation with no systemic features.14
Although the case patient’s lesion had yellow-coloured crust that can indicate S. aureus infection, an infective aetiology is unlikely given the protracted course of the lesion. She was not breastfeeding and did not have other inciting trauma to provide bacterial entry.
Paget’s disease of the nipple
This is the correct diagnosis. Paget’s disease of the nipple is a type of breast carcinoma that is thought to be caused by epidermal invasion of the nipple and areola by underlying in situ or invasive ductal carcinoma in the deeper breast tissue.17 It is a very rare condition, occurring in fewer than 3% of breast cancers overall.2 The disease most commonly affects postmenopausal women of Anglo-saxon descent who live in Western countries. However, rare cases have been noted in men and exceptionally cases are bilateral.2,17-19
The disease often presents as patches extending from the nipple and areola that resemble dermatitis.2 The early changes may be minimal, with a small, crusted and intermittently weeping area on the nipple that may leave brownish stains on clothing.2 These changes may be accompanied by itching, pricking or burning sensations, and the surface may become progressively thickened and erythematous.20 With more advanced lesions, erosions, ulceration, bleeding and extension may occur into the surrounding skin with a well-demarcated, slightly raised and irregular outline.17,21 On dermoscopy, pink structureless areas, fine white scale and dotted and short linear vessels are typically seen.12 About 30 to 50% of patients will have a palpable breast lump, which is associated with a poor prognosis as half of these will have axillary node involvement.2,22 It is not uncommon for patients to wait over 12 months before seeking medical advice.2
Nipple eczema is a common mimicker of Paget’s disease of the nipple, which may lead to a delayed or missed diagnosis.17,21 If nipple eczema is suspected but the diagnosis is unclear then a biopsy should be performed, particularly if there has been no response to topical corticosteroids.2
Investigations and management
A full-thickness biopsy of the nipple and areola is important if a patient presents with nipple-areola skin changes to establish the correct diagnosis but may not always detect an underlying breast carcinoma.2,17,21 All patients should have a mammogram or ultrasound to demonstrate whether there is deeper pathology in the underlying breast because this will help guide the extent of surgery required.2 However, breast MRI can identify changes that might not be detected by an ultrasound or mammogram.20,23,24 Breast MRI should be arranged if mammographic or ultrasound findings are normal or the extent of disease is uncertain.25,26
Referral of the patient to a breast surgeon is required. Management should be carried out as for carcinoma of the breast, which will likely involve surgery with or without axillary lymph node dissection and/or chemotherapy.2,20 In patients who have no evidence of an underlying carcinoma, breast conservation may be appropriate, with or without radiotherapy according to the presence or absence of an invasive component.27,28
Outcome
The case patient had a nipple biopsy, which confirmed the diagnosis of Paget’s disease of the nipple. She was referred to a breast oncoplastic surgeon, where further investigations, including biopsies and breast MRI, revealed high grade ductal carcinoma in situ. She underwent bilateral mastectomies and chemotherapy with paclitaxel and trastuzumab. Two years on, she is disease-free. MT
COMPETING INTERESTS: None.
References
1. Graham DF. Eczema of the nipple. Trans St Johns Hosp Dermatol Soc 1972; 58: 98-99.
2. Burns T, Breathnach S, Cox N, Griffiths C. Rook’s textbook of dermatology. 8th ed. Chichester UK: Wiley-Blackwell; 2010.
3. Mevorah B, Frenk E, Wietlisbach V, Carrel CF. Minor clinical features of atopic dermatitis. Evaluation of their diagnostic significance. Dermatologica 1988; 177: 360-364.
4. Amato L, Berti S, Chiarini C, Fabbri P. Atopic dermatitis exclusively localized on nipples and areolas. Pediatr Dermatol 2005; 22: 64-66.
5. Barankin B, Gross MS. Nipple and areolar eczema in the breastfeeding woman. J Cutan Med Surg 2004; 8: 126-130.
6. García M, del Pozo MD, Díez J, Muñoz D, de Corrès LF. Allergic contact dermatitis from a beeswax nipple-protective. Contact Dermatitis 1995; 33: 440-441.
7. McGeorge BC, Steele MC. Allergic contact dermatitis of the nipple from Roman chamomile ointment. Contact Dermatitis 1991; 24: 139-140.
8. Adams BB. Dermatologic disorders of the athlete. Sports Med 2002; 32: 309-321.
9. Kapur N, Goldsmith PC. Nipple dermatitis – not all what it ‘seams’. Contact Dermatitis 2001; 45: 44-45.
10. Saritas AG, Dalci K, Topal U, Beydola S, Açikalin A, Rencuuzogullari A. Psoriasis, a rare disease of the nipple-areola. A case report. Ann Ital Chir 2019 Nov; 8.
11. Verma SB. Striae: stretching the long list of precipitating factors for ‘true koebnerization’ of vitiligo, lichen planus and psoriasis. Clin Exp Dermatol 2009; 34: 880-883.
12. Apalla Z, Errichetti E, Kyrgidis A, et al. Dermoscopic features of mammary Paget’s disease: a retrospective case‐control study by the International Dermoscopy Society. J Eur Acad Dermatol Venereol 2019; 33: 1892-1898.
13. Parker M, Collier T, Leslie H. Topley & Wilson’s Principles of bacteriology, virology and immunity. 8th ed. London UK: Edward Arnold; 1990.
14. Livingstone VH, Willis CE, Berkow J. Staphylococcus aureus and sore nipples. Can Fam Physician 1996; 42: 654-659.
15. Duncan JT, Walker J. Staphylococcus aureus in the milk of nursing mothers and the alimentary canal of their infants: a report to the Medical Research Council. Epidemiol Infect 1942; 42: 474-484.
16. Cantlie HB. Treatment of acute puerperal mastitis and breast abscess. Can Fam Physician 1988; 34: 2221-2226.
17. Karakas C. Paget’s disease of the breast. J Carcinog 2011; 10: 31.
18. Desai DC, Brennan EJ Jr, Carp NZ. Paget’s disease of the male breast. Am Surg 1996; 62: 1068-1072.
19. Ucar AE, Korukluoglu B, Ergul E, Aydin R, Kusdemir A. Bilateral Paget disease of the male nipple: first report. Breast 2007; 17: 317-318.
20. Alkul M, Lin CP, Truitt J, Tarbox MB. A tale of three common nipple diseases. Proc (Bayl Univ Med Cent) 2022; 35: 354-356.
21. Meibodi NT, Ghoyunlu VM, Javidi Z, Nahidi Y. Clinicopathologic evaluation of mammary Paget’s disease. Indian J Dermatol 2008; 53: 21-23.
22. Dalberg K, Hellborg H, Wärnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat 2008; 111: 313-319.
23. Frei KA, Bonel HM, Pelte MF, Hylton NM, Kinkel K. Paget disease of the breast: findings at magnetic resonance imaging and histopathologic correlation. Invest Radiol 2005; 40: 363-367.
24. Morrogh M, Morris EA, Liberman L, van Zee K, Cody HS 3rd, King TA. MRI identifies otherwise occult disease in select patients with Paget disease of the nipple. J Am Coll Surg 2008; 206: 316-321.
25. Morrogh M, Morris EA, Liberman L, Borgen PI, King TA. The predictive value of ductography and magnetic resonance imaging in the management of nipple discharge. Ann Surg Oncol 2007; 14: 3369-3377.
26. Günhan-Bilgen I, Oktay A. Paget’s disease of the breast: clinical, mammographic, sonographic and pathologic findings in 52 cases. Eur J Radiol 2006; 60: 256-263.
27. Lagios MD, Westdahl PR, Rose MR, Concannon S. Paget’s disease of the nipple. Alternative management in cases without or with minimal extent of underlying breast carcinoma. Cancer 1984; 54: 545-551.
28. Fourquet A, Campana F, Vielh P, Schlienger P, Jullien D, Vilcoq JR. Paget’s disease of the nipple without detectable breast tumor: conservative management with radiation therapy. Int J Radiat Oncol Biol Phys 1987; 13: 1463-1465.
Skin cancer